Buscar
-
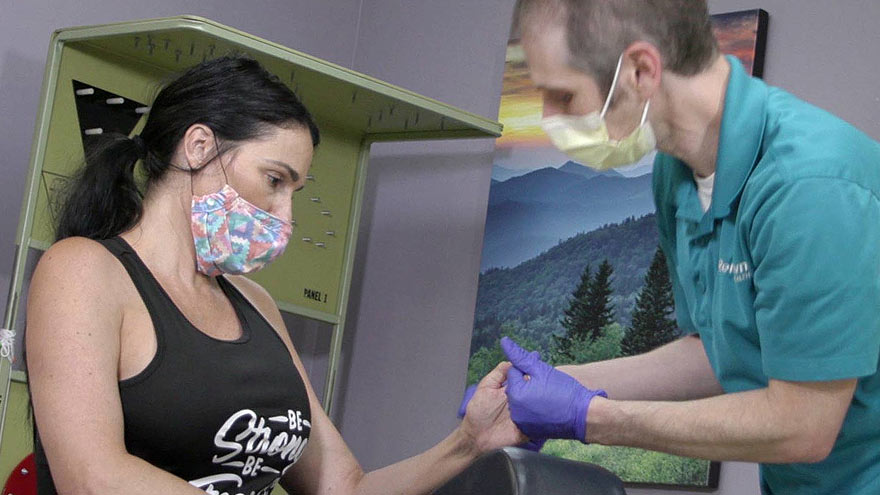
Departamento destacado: Special Procedures
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
How to Treat a Sprain or Strain
Injuries happen to everyone. They are caused by participating in sports, recreational activities like hiking, and even by accidentally stepping off a curb wrong. If you experience a sprain or strain, the first few days are often the most painful. Renown Sports Medicine physicians Luis Palacio, MD and Brandon Hockenberry, MD walked us through what to do after an injury. Listen to Your Body See a medical professional right away if: You know or suspect that a bone is broken You are having difficulties putting full weight on a joint of the leg Pain or swelling is severe There is a sign of an infection, such as redness and warmth in the joint The First 24-72 Hours Joint sprains tend to swell more than muscle strains. You can use ice as needed for comfort and to relieve any pain, but do not use ice for more than 15-20 minutes at a time. Ice and NSAIDs (such as ibuprofen) can help prevent excessive swelling and mask the pain, but they do not speed recovery. Some research shows that overuse of ice actually delays recovery. During the first 24-72 hours, your injury will go through an inflammation phase. Inflammation is your body’s natural way to dispose of dead tissue cells, build new healthy structures, and hopefully heal even stronger than before.
-
How to Manage and Prevent Tendonitis
Tendonitis occurs when a tendon in your body is inflamed or irritated. This painful condition can impact your day-to-day activities, but can be managed and prevented. Luis Palacio, MD, shared some insights into how to manage tendonitis. Overuse and Repetitive Motion Tendons are complex tissues in our body that connect muscles to bones, allowing us to move. Unfortunately, sometimes these tendons become inflamed, worn down or injured, a condition called tendonitis. Symptoms of tendonitis include pain or dull ache, tenderness and mild swelling at the site. While tendonitis can be caused by a sudden injury, it is more commonly seen in frequent motions, including: Repetitive motions in exercise, work or other physical activities. Awkward positions in a movement, including poor posture. Forced movements that strain your body. Sudden increase in frequency of movement or level of difficulty, including little to no recover time between new activity. Shoes without proper support or hard surfaces, such as concrete floors. Evaluation is Key If you suspect that you have tendonitis and it does not resolve on its own after a few days, you should get it evaluated by a primary care or sports medicine doctor. They can make recommendations to aid your recovery and refer you to the right sub-specialist if needed. With some intentional actions, you can help reduce the risk of tendonitis with the following suggestions: Add variety: Mixing up the type of exercise you do will help prevent repetitive motions that can result in overuse. Stretch and condition: Make sure the keep up with proper stretching and muscle strengthening to support your physical activities. Do it right: Make sure that the way you are completing exercise or work-related physical activities is correct. Seek out a professional for lessons or guidance if you are unsure.
-
7 Important Vasectomy Questions for Your Doctor
If you and your partner are looking for a more permanent birth control method, you might consider a vasectomy. Although vasectomies are common, knowledge about them isn’t quite as common or talked about. If you are considering a vasectomy, talking with your primary care doctor is a great way to learn more and start the process. We consulted with Dr. Aurosis Reddy a primary care doctor with Renown Health – South Carson, about key topics to discuss with your doctor when considering a vasectomy. What is a vasectomy? A vasectomy – also called male sterilization – is a form of male birth control that blocks sperm from reaching semen, according to the American Urological Association (AUA). How effective and safe are vasectomies? Vasectomies are one of the most effective methods of birth control with a long-term success rate of over 99%. A vasectomy has been a safe and successful birth control method for many years. More than 500,000 men elect to have vasectomies every year in the U.S., and the number is rising. A vasectomy is also generally a low-risk procedure with a low complication rate ranging between 1-2%. What does the recovery period look like? A vasectomy is typically a quick procedure that takes under thirty minutes and can be performed in an outpatient setting under local anesthesia. Recovery from a vasectomy is also considered relatively easy. After a vasectomy, most can: Resume everyday activities within two to three days Resume normal exercise in one week Start engaging in sexual activity again in one week Your doctor can provide more details on what your individualized recovery process will look like.
Read More About 7 Important Vasectomy Questions for Your Doctor
-
8 pruebas de evaluación de la salud importantes para hombres
Unfortunately, men are less likely to visit their doctor for exams, screenings, and consults than women. So with the help of Bonnie Ferrara, MD of Renown Health, we've put together a list of eight screenings to help men stay on top of their health game. 1. Blood Pressure Tests Ages 20+ Blood Pressure tests measure the pressure in your arteries as your heart pumps. Biennial (every two years) checks are recommended if you have normal blood pressure or more frequently if you have high blood pressure (hypertension) or low blood pressure (hypotension). The United States Preventative Services Taskforce cites normal blood pressure below 120 systolic (top number) and 80 diastolic (bottom number). 2. Cholesterol Screening Ages 20+ High levels of cholesterol increase your risk of stroke and heart disease. A simple blood test will help your healthcare provider determine your numbers and if you're at risk. If you have a family history of diabetes or heart disease, you may need yearly screenings. But, again, your doctor can provide the best course of action.
-
3 datos importantes de atención médica para la generación milenial
Many millennials are fortunate to have good health, but it’s important to be prepared for your next doctor’s visit. Here are three things that millennials should stay on top of for tracking and maintaining their health. For many millennials, doctor visits and preventive healthcare fall by the wayside. Alison Lynch, MD, a family medicine provider with Renown Medical Group says there are a few key things you can do now to set yourself up for a healthy future. 1. Establish with a Primary Care Provider Millennials are more likely to go to urgent care or consult the internet when a healthcare issue arises. While these are helpful tools, here’s a better one: a primary care provider. The benefit of establishing with a primary care provider is that your medical records, history and a baseline for your health will be documented. That means that when a problem or question comes up, your doctor will already have helpful information on file and can help you navigate your needs. Having a primary care provider is often required for prescription refills and referrals to a specialist. By establishing now, you’ll be able to get what you need in the future much faster. Make an Appointment Today 2. Protect Yourself and Your Community There are a few vaccinations and screenings that Dr. Lynch recommends for millennials. Flu Shots: These are available every year and are recommended for protecting not only yourself against the flu but also others you may come into contact with. Flu shots are usually available from August through December through your healthcare provider, pharmacies and pop-up events. Tetanus or Tdap: Most people receive a tetanus shot as a child, but it’s recommended that everyone get a booster every 10 years. If you are overdue, talk to your primary care provider or pharmacist about getting updated. Pap smear: If you’re a woman, a pap smear is recommended every three years in your 20s and every five years in your 30s. HPV vaccine: This vaccine helps prevent the virus that causes cervical cancer as well as the majority of head and neck cancers and warts. The HPV vaccine is recommended for all genders up until age 45. STD screening: Consider an STI/STD screening if you’re sexually active.
-
¿Está en riesgo de sufrir un derrame cerebral?
Did you know an estimated 1.9 million neurons and 14 billion synapses are lost per minute during a stroke? That’s why every second counts. Anyone can have a stroke, but your chances increase if you have certain risk factors. That’s why the best way to protect yourself or your loved ones from a stroke is to know the risks and how to manage them. You can make changes to your lifestyle to lower your risk of stroke by asking yourself the following questions: 1. Is my blood pressure normal? High blood pressure is the leading cause of stroke and the most important controllable risk factor. If you’ve had a stroke, lowering your blood pressure can help prevent future strokes. 2. Can I quit smoking? Smoking damages blood vessels, clogs arteries and raises blood pressure — doubling your risk of stroke. If you want to reduce your risk of stroke and heart attack, quitting smoking is the first step — and Renown can help you with this. Learn more: Renown Health Quit Tobacco Program. 3. Do I make time to exercise 30 minutes a day? Many studies link consistent exercise habits with lower stroke risk. Also, being overweight contributes to high cholesterol, high blood pressure, heart disease and diabetes, all increasing your stroke risk. You don’t need to run a marathon — just commit to making time to move each day. 4. Do I regularly eat processed food and sugar? Eating less cholesterol and fat, especially saturated and trans fats, may reduce the fatty deposits (plaque) in your arteries. Also, eating five or more servings of fruits and vegetables per day may reduce your stroke risk. If you are diabetic, follow recommendations to get your diabetes under control.
-
Take Charge of Your Sexual Health
Much like general physical and mental health, sexual health is an essential aspect of your overall well-being. Therefore, educating yourself on your sexual health is an important piece regarding your overall wellness. Secure & Private Virtual Visits Did you know that many sexually transmitted disease appointments can happen virtually, in the privacy of your own home? Our providers can perform a screening examination for sexually transmitted illness (without symptoms) when it’s convenient for you. This is a great option if the topic makes you uncomfortable during an in-person visit, or if you can’t find time to visit your primary care provider or local urgent care. After the telehealth appointment, your provider will determine the next steps for you. Remember, in-person visits are always an option as well. Here’s how you can take charge of your sexual health: Get Comfortable with Getting Tested Surprisingly, some people with STDs don't show symptoms, meaning they may not even know they have an STD unless they get tested. Even if an STD shows no symptoms, the result of non-treatment can be serious. Bret Michael Bellard, MD, with Renown Medical Group, shares that it’s important for people to get tested for STDs because if left untreated, they can cause the following health problems: Loss of fertility Pregnancy complications Other health issues When to Visit Your Primary Care Provider Who should get tested and how often? “The recommendations are that everyone from ages 13 to 64 should get tested at least once for HIV. All sexually active adults should also be tested for other STDs once a year, and all pregnant women should be tested at the start of their pregnancy,” says Dr. Bellard. Some STDs, like syphilis, can be passed from mother to baby, so it's important for women to get tested as soon as they know they’re pregnant. Dr. Bellard recommends going to your primary care provider for testing. “They can also give advice on prevention and other health topics.” If you don’t have a primary care provider, this is a great reason to get established with one. Women with an established OB/GYN can have STD testing done simultaneously with their annual pelvic exam. The providers in Renown's network care for patients of all ages and specialize in family medicine, internal medicine, pediatrics and OB/GYN. Practice Safe Sex STDs are preventable. Practicing safe sex and getting tested routinely are your best defenses against all types of STDs. For many, the conversation about sexually transmitted diseases is awkward and many avoid it. To lower your risk of contracting an STD, don’t wait until you’re “in the moment” to have the conversation with your partner about the last time you were both last tested. If you haven’t gotten tested in-between new partners, use latex condoms every time you have sex until you are both confirmed negative of STDs. Condoms are not 100% effective at preventing disease or pregnancy. However, they are extremely effective if used properly. To establish Primary Care, visit renown.org/virtualvisits or call 775-982-5000
-
Women and Stroke Surprising Signs to Know
Stroke is unfortunately common, with 1 in 5 American women experiencing it each year. When it comes to a stroke the phrase “time is brain” speaks to the urgency of getting rapid care. In fact, a woman may lose nearly 2 million neurons per minute of oxygen loss to the brain. The Renown Health Comprehensive Stroke Center experts share the importance of timely treatment and how stroke symptoms can differ in women. Women and Stroke – Surprising Symptoms Each year stroke affects more women than men. Even more concerning, women are less likely to recover from a stroke. The following non-traditional, less common, warning signs can be common in women: Hiccups with chest pain Sudden disorientation, drowsiness, confusion or a general altered mental status Nausea or vomiting A sudden headache that feels like the ‘worst headache of your life’ Unusual chest pain (especially with hiccups) Body numbness or weakness, such as an arm or leg suddenly ‘falling asleep’ Fainting or loss of consciousness Stroke Diagnosis The first step is neuroimaging by CT scan. This allows for rapid identification of any bleed, and also assists in determining candidacy for the early clot busting medication. MRI brain imaging is much higher resolution, and can better determine the core stroke size, assisting in prognosis and recovery. Since strokes have several different origins, an inpatient workup is essential to determine the underlying cause. Whether the stroke is secondary to plaque in the large vessels, clots being thrown in the setting of atrial fibrillation (an abnormal heart rhythm), or small vessel disease from years of uncontrolled vascular risk factors (high blood pressure, smoking, high cholesterol, diabetes), determining the cause is essential to implementing a management plan to reduce risk for further strokes. Quick Treatment for Stroke is Key Early recognition of stroke symptoms and seeking prompt attention is paramount. There are interventions that can be instituted to minimize the stroke and increase likelihood of recovery, but only if a patient presents to the hospital early. A clot busting medication, called tPA, can be given to patients with stroke if given within 4-5 hours from time of onset. Renown Regional Health Center is designated as a Comprehensive Stroke Center, the highest level of stroke certification available. To earn the designation of comprehensive stroke center, a hospital has to meet stringent requirements, including biannual on-site evaluations. This includes care for ischemic stroke patients (lack of blood flow), hemorrhagic stroke patients (bleeds), and determining the underlying cause to guide secondary stroke management prevention. Stroke Symptoms Remember “B.E.F.A.S.T.” to recognize the symptoms of a stroke below: B – Balance Being off balance or dizzy, is common. E – Eyes An eyesight change such as blurring or double vision may occur. F – Face droop One side of the face, or lip, droops A – Arm weakness Does one arm drift down? S – Speech Talking may slur or sound strange. T – Time Time to call 911. Call an ambulance immediately if you or anyone else, experiences any of these symptoms.
-
How to Spot Depression in Men
Has a male in your life been affected by depression? It could be your father, husband, or son. Or maybe your brother, a friend – or even, your co-worker. They all have one thing in common, they’re men and they may not always be able recognize when they need help. Here’s how you can support the men in your life by understanding their unique signs of depression. Dr. Coard, Ed.D., Psychologist with Renown Behavioral Health, weighs in on the topic of depression and the warning signs. More than 6 million men are diagnosed with depression each year, and surprisingly, depression in men can differ from women. The signs of depression are not easily recognized and it’s common for men to be in denial about what they’re going through. They can demonstrate anger and aggression instead of sadness – making it difficult for loved ones, or even their providers, to recognize. Behavioral Signs of Depression in Men High levels of the hormone cortisol are released during stressful situations affecting the neurotransmitter, serotonin (a feel good hormone), contributing to depression. You can identify depression or suicidal tendencies by paying close attention to the following behavioral changes: Anger, irritability, or aggression Avoiding family or social situations Losing interest in family responsibilities, passions and hobbies Lack of sex drive Becoming controlling/abusive in relationships Risk-taking behavior such as; unsafe sex, overspending or gambling Not being able to concentrate or remember details Excessive drinking or drug use Having frequent thoughts about death Talking about suicide Attempting suicide Factors That Lead to Depression in Men Life Events Work stress or long-term unemployment can be huge contributing factors relating to depression. This type of life event can be overwhelming, making it impossible for a man to cope. Changes in Relationships The loss of a relationship can be a significant contributing factor to the emergence of depressive symptoms and past experienced physical, sexual, or emotionally abusive relationships. With this in mind, counseling can often help individual to overcome this type of trauma. Grief and Loss Overwhelming sadness due to the loss of a loved one can trigger depression. Although normal, each person goes through their own grieving period. For example, normal responses to death are insomnia, poor appetite and loss of interest in activities. Pay attention if grief seems prolonged or out of the ordinary. Health Problems In particular, depression coexists with medical conditions. As men age, this can be passed off as normal aging, but it could be more serious. In addition, illnesses such as thyroid disorders, Addison’s disease and liver disease can cause depressive symptoms. Diabetes, cancer, heart disease, or Parkinson’s disease can affect any age, thus triggering or worsening depression. Some older men also feel like they may be suffering from dementia because of difficulties with memory this may be a symptom of depression. A trip to the doctor may be in order to help alleviate concern and worry. Depression in Men and Suicide Frequently the emotional pain occurring with depression can distort a man’s ability to see a solution beyond suicide. Individuals with depression become very rigid and constricted in the way they solve problems. The statistics below speak for themselves, helping us understand the need to reach out to those who need our support. Male suicide rates are on rising – men die by suicide 3.53 times more often than women, accounting for 70% of all suicides. Sadly, every day 129 men commit suicide. White males accounted for 69.67% of suicide deaths in 2017. In 2017, firearms accounted for 50.57% of all suicide deaths. Middle aged Men who are middle aged have the highest suicide rates. 40% of those identifying as transgender have attempted suicide in their lifetime. Males who are guy or transgendered are at an increased risk for suicide attempts, especially before age 25. Veterans often suffer from post-traumatic stress disorder (PTSD) and depression, and are more likely to act on a suicide plan. How You Can Help Now that you can identify some of the warning signs of depression, here’s how you can help: Talk about your concern and communicate that you’re there to help him. Let him know depression is a medical condition and will usually get better with treatment. Suggest professional help from a Primary Care Provider, Psychologist or Therapist. Help set up appointments and offer to accompany him – let him make the decision, but make it clear you’re there for him, no matter what he decides. If you feel he is in a dire or life-threatening situation, contact 911. Call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to talk to a trained counselor. Call the Veteran’s Crisis Line at 1-800-273-TALK (1-800-273-8255) and press “1”
-
If You're a Soon-To-Be-Dad, We've Got Tips for You
“You’re gonna be a dad!” Whether you’ve been waiting years to hear those words or still think you’re too much of a kid to have a kid, the reality of impending fatherhood can be terrifying for any first-time, soon-to-be-dad. But not to worry, Best Medicine has some timely tips to help calm those bundle-of-joy fears and help you rock your new role as a brand-new, baby daddy. Winter is Where Babies Come From Fact: More babies are born in September than any other month, with spill over (and spit-up) into October. Subtract ten months for the typical 40-week, bun-in-the-oven baking time and early winter stands out as the top baby-making part of the year. Is it the cozy nights before a fire as people avoid the snowman-friendly temperatures outside? Possibly. There could be any number of reasons, both seasonal and otherwise, for what will eventually arrive in the fall and immediately steal your heart — and untold hours of your sleep. Though moms carry most of the baby burden traditionally (and literally for three trimesters), that’s no excuse for the soon-to-be-dad not to step up to the plate and take a swing at being the best partner and father on the planet. Below is a list of tips and resources to help you do just that. So read on, daddy-o. Tip #1: Don’t Freak Out Ok, you’re probably going to freak out even if we tell you not to. But once you calm down, consider this: human beings have been having babies for millions of years, and many of those soon-to-be-dads had it much tougher than we do today. And guess what? The human race is still going strong. Those first moms and dads did a good job — and you will too, with a little help. Tip #2: Take a Class Knowledge is power. In this case, it's diaper-changing, swaddle-wrapping, 2 a.m.-feeding power. And for you and your partner, taking a parenting class or two should be a no-brainer. You'll both learn what to expect and prepare for as you support each other and bond with your baby even before he or she arrives. Tip #3: Learn From Other Dads If the thought of sitting in a room full of full-bellied women and their partners makes you uncomfortable, you may opt to stick with bros for your lesson plan. Dad-only classes and soon-to-be-dad support groups — taught and led by seasoned fathers with tales to tell and words of wisdom to share — are available online and in cities and communities around the country. Dad-focused sites also offer advice for new and still-learning proud papas. Here are a few options to check out: Boot Camp for New Dads City Dads Group Wilderdad.com Fatherly.com Fathers.com Tip #4: Babies are Required Reading Haven't read a good book lately? Well, if you're expecting a baby, now is the time to flip through a few pages that could make your life a whole lot easier in a few months. There's no such thing as being too-well-read when it comes to your fast-approaching, adorable little poop machine. The least you can do is read a book or two, or seven. We're Pregnant! The First Time Dad's Pregnancy Handbook From Dude to Dad: The Diaper Dude Guide to Pregnancy We're Pregnant! The First Time Dad's Pregnancy Handbook What to Expect When Your Wife Is Expanding Be Prepared: A Practical Handbook for New Dads The New Dad's Survival Guide: Man-to-Man Advice for First-Time Fathers What to Expect When You're Expecting Tip #5: Be a Prepared Soon-To-Be-Dad Tips 1 through 4 are meant to help alleviate some of your jittery, new-dad anxiety. And we hope they do just that. But if you really want to hold that "Best Dad Ever" coffee mug starting on day one, there are also some practical things you can do to prepare. Check these items off your list now to make life with baby more baby-, mommy- and daddy-friendly from the get-go. Buy a baby/child car seat. Three out of four car seats are installed incorrectly. Protect your children by ensuring they are riding in a properly secured and age-appropriate car seat. Renown Children’s Hospital Car Seat Station is staffed by certified technicians who provide child vehicle safety restraint education, inspection and installation. Set up the baby's nursery early, including furniture Stock up on diapers and baby supplies Cook and freeze 2 weeks of food for nights when no one wants to cook Research family healthcare Agree upon a shared diaper-changing/feeding schedule Ask about paternity leave from work Get bills and finances up-to-date or pre-pay to avoid late charges Give the home a thorough cleaning before the baby arrives
Read More About If You're a Soon-To-Be-Dad, We've Got Tips for You
-
Una guerrera que sobrevivió a un ataque cerebrovascular: la historia de Kimi
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”