Buscar
-
Prevenir el cáncer de piel Consejos de una médica
Want to protect yourself from skin damage from the sun’s harmful rays? Dr. Angela Walker, dermatologist with Renown Medical Group, shares what you can do to prevent skin cancer. What can people do to prevent skin cancer while enjoying the outdoors? There are several steps you can take to protect your skin from the sun. “I caution all of my patients to avoid the sun during the hours of 10 a.m. until 2 p.m. when UV rays are strongest. I also encourage people to wear sleeves on cooler days. And don’t forget that we still need to wear sunscreen on cloudy days! UV rays can still cause sun damage on cloudy days. Preventing skin cancer also entails wearing sunscreen of at least SPF 30 everyday. Are hats also a good idea for skin protection? Yes, of course! Choose a wide-brim hat that shades the face as well as the back of the neck for extra protection against UV rays. When it comes to identifying skin cancer, what should people watch for? We use easy-to-remember letters when checking for spots on the skin; it’s called the ABCDEs: A - Asymmetry: One half of the mole or lesion doesn't match the other half. B - Border irregularity: The edges of the mole are irregular, blurred, or notched. C - Color variation: The mole has different shades of color or uneven color distribution. D - Diameter: The diameter of the mole is larger than the size of a pencil eraser (about 6 millimeters) or is increasing in size. E - Evolution: Any changes in the mole over time, such as size, shape, color, itching, bleeding, or crusting. These guidelines can help in identifying potentially suspicious skin lesions, but it's important to consult a dermatologist for proper evaluation and diagnosis. Early detection is crucial for successful treatment of skin cancer.
-
El Papel de los Ginecólogos Obstetras en la Atención de la Salud de la Mujer
Obstetrician-gynecologists (OBGYNs) see patients from menses (the monthly menstrual cycle that occurs as a part of the female reproductive system), pregnancy and childbirth through menopause and play a pivotal role in managing reproductive health and overall wellness. Dr. James Alexander with Renown Women's Health explains. "As experts in women's health, we are uniquely positioned to recognize subtle changes or symptoms that might indicate broader health issues. This comprehensive approach allows us to serve as a valuable first touchpoint for various health concerns." Preventive Screenings: A Proactive Approach One key aspect is an OBGYN's ability to recommend preventive screenings based on your symptoms, age, lifestyle and medical history. For instance, lipid screenings are critical for monitoring cholesterol levels, which can be a significant factor in women’s heart disease. An OBGYN keeps up with the current guidelines for routine screening as well as in women with risk factors such as high blood pressure, diabetes, or a family history of heart disease during your visit. By identifying risks and abnormal screening early, they can collaborate with you to implement lifestyle changes or treatments to reduce your risk of heart conditions. Schedule Your Screening Appointment Make an Appointment by Phone: 775-982-5000
Read More About The Expanded Role of OBGYNs in Women's Healthcare
-
Understanding the Reasons Behind Heavy Menstrual Cycles
While menstrual cycles can be an annoying inconvenience for many women, heavy bleeding (menorrhagia) is not normal and can disrupt your life. A few days of heavy flow at the start of your period is usually nothing to worry about. However, if you’re frequently experiencing very heavy periods, you should discuss it with your gynecologist or primary care provider. Dr. Megan Fish, an OB-GYN with Renown Women’s Health, discusses various reasons, evaluation and treatment methods when it comes to heavy menstrual cycles. What is classified as heavy menstrual bleeding? The American College of Obstetricians and Gynecologists considers heavy bleeding to be any of the following signs: Bleeding that lasts more than 7 days. Bleeding that soaks through one or more tampons or pads every hour for several hours in a row. Needing to wear more than one pad at a time to control menstrual flow. Needing to change pads or tampons during the night. Menstrual flow with blood clots that are as big as a quarter or larger. What are the most common reasons for heavier periods? A variety of reasons why someone might have heavy periods. Fortunately, most of these problems are treatable. Because each woman's period is unique, only a doctor can definitively determine the cause of your heavy periods. Some of the most common issues that cause heavy periods include: Hormone imbalances such as anovulation, thyroid disease and Polycystic Ovary Syndrome (PCOS). Structural abnormalities in your uterus such as polyps or fibroids. Precancer and cancer such as uterine, cervical, vaginal, ovarian or endometrial hyperplasia. Infections such as chlamydia, gonorrhea, endometritis or vaginitis. Other medical conditions such as liver disease, kidney disease or Pelvic Inflammatory Disease. Medications such as blood thinners and aspirin, hormone replacement therapy, Intrauterine devices (IUDs), birth control pills and injectables. Pregnancy-related problems such as a miscarriage or ectopic pregnancy.
Read More About Understanding the Reasons Behind Heavy Menstrual Cycles
-
Health Insurance Terms Explained: HMO, EPO and PPO Plans
When it comes to purchasing a health insurance plan, you’ve probably heard of the two plan types, HMO and PPO, but what exactly do these terms mean, and what is an EPO? Let’s learn more about these plan types and how you can choose the plan that meets your needs. What is an HMO Plan? HMO stands for “Health Maintenance Organization.” HMO plans contract with doctors and hospitals creating a network to provide health services for members in a specific area at lower rates, while also meeting quality standards. HMO plans typically require you to select a primary care physician (PCP) and obtain a referral from your PCP to see a specialist or to have certain tests done. If you choose to see a provider outside of the HMO’s network, the plan will not cover those services and you will be responsible for all charges. What is an EPO Plan? An EPO stands for “Exclusive Provider Organization.” This plan provides members with the opportunity to choose in-network providers within a broader network and to visit specialists without a referral from their primary care doctor. EPO plans offer a larger network than an HMO plan but typically do not have the out-of-network benefits of PPO plans. EPO plans do not require you to select a primary care physician (PCP) giving you a broader network of providers. EPO options are a great cost-saving option with more flexibility than a standard HMO plan. What is a PPO Plan? PPO stands for “Preferred Provider Organization.” PPO plans are often more flexible when it comes to choosing a doctor or a hospital. These plans still include a network of providers, but there are fewer restrictions on the providers you choose. PPO plans do not require you to select a primary care physician (PCP), giving you a broader network of providers. So, which plan should you choose? Each plan type has different benefits, so it depends on your health needs when choosing the right plan type. If you are looking for flexibility when choosing providers and locations, a PPO plan may better fit your needs. An EPO plan may be a better option if you want the flexibility of a larger network, but don’t necessarily need out-of-network benefits. If you regularly seek care in a certain geographic area and are looking for a health insurance plan at a lower price point, consider an HMO plan. To keep costs low, insurance carriers contract with providers and partner in plan members’ health to ensure quality care at the lowest cost. Whether you choose an HMO, EPO or PPO option, partnering with your health insurance carrier and your healthcare provider will help you receive the best care while controlling your out-of-pocket costs. Keep in mind that most insurance carriers offer emergency care coverage for all three plan options (HMO, PPO, EPO). Get the most out of your health insurance benefits! Established in 1988, Hometown Health is the insurance division of Renown Health and is northern Nevada’s largest and only locally-owned, not-for-profit insurance company providing wide-ranging medical coverage and great customer service to members.
Read More About Health Insurance Terms Explained: HMO, EPO and PPO Plans
-
Health Insurance Terms Explained: Deductible and Out-of-Pocket Maximum
Health insurance might be one of the most complicated purchases you will make throughout your life, so it is important to understand the terms and definitions insurance companies use. Keep these in mind as you are comparing health insurance plan options to choose the right plan for you and make the most of your health insurance benefits. One area of health insurance that can cause confusion is the difference between a plan's deductible and out-of-pocket maximum. They both represent points at which the insurance company starts paying for covered services, but what are they and how do they work? What is a deductible? A deductible is the dollar amount you pay to healthcare providers for covered services each year before insurance pays for services, other than preventive care. After you pay your deductible, you usually pay only a copayment (copay) or coinsurance for covered services. Your insurance company pays the rest. Generally, plans with lower monthly premiums have higher deductibles. Plans with higher monthly premiums usually have lower deductibles. What is the out-of-pocket maximum? An out-of-pocket maximum is the most you or your family will pay for covered services in a calendar year. It combines deductibles and cost-sharing costs (coinsurance and copays). The out-of-pocket maximum does not include costs you paid for insurance premiums, costs for not-covered services or services received out-of-network. Here's an example: You get into an accident and go to the emergency room. Your insurance policy has a $1,000 deductible and an out-of-pocket maximum of $4,500. You pay the $1,000 deductible to the hospital before your insurance company will pay for any of the covered services you need. If you received services at the hospital that exceed $1,000, the insurance company will pay the covered charges because you have met your deductible for the year. The $1,000 you paid goes toward your out-of-pocket maximum, leaving you with $3,500 left to pay on copays and coinsurance for the rest of the calendar year. If you need services at the emergency room or any other covered services in the future, you will still have to pay the copay or coinsurance amount included in your policy, which goes toward your out-of-pocket maximum. If you reach your out-of-pocket maximum, you will no longer pay copays or coinsurance and your insurance will pay for all of the covered services you require for the rest of the calendar year.
Read More About Health Insurance Terms Explained: Deductible and Out-of-Pocket Maximum
-
Copays vs. Coinsurance: Know the Difference
Health insurance is complicated, but you don't have to figure it out alone. Understanding terms and definitions is important when comparing health insurance plans. When you know more about health insurance, it can be much easier to make the right choice for you and your family. A common question when it comes to health insurance is, "Who pays for what?" Health insurance plans are very diverse and depending on your plan, you can have different types of cost-sharing: the cost of a medical visit or procedure an insured person shares with their insurance company. Two common examples of cost-sharing are copayments and coinsurance. You've likely heard both terms, but what are they and how are they different? Copayments Copayments (or copays) are typically a fixed dollar amount the insured person pays for their visit or procedure. They are a standard part of many health insurance plans and are usually collected for services like doctor visits or prescription drugs. For example: You go to the doctor because you are feeling sick. Your insurance policy states that you have a $20 copay for doctor office visits. You pay your $20 copay at the time of service and see the doctor. Coinsurance This is typically a percentage of the total cost of a visit or procedure. Like copays, coinsurance is a standard form of cost-sharing found in many insurance plans. For example: After a fall, you require crutches while you heal. Your coinsurance for durable medical equipment, like crutches, is 20% of the total cost. The crutches cost $50, so your insurance company will pay $40, or 80%, of the total cost. You will be billed $10 for your 20% coinsurance.
-
Understanding and Managing Childhood Asthma
Dr. Shipra Singh, a Pediatric Pulmonologist, outlines the challenges of diagnosing asthma in children due to symptoms resembling other respiratory issues. It's particularly difficult to identify in infants and young children, who may not clearly exhibit breathing difficulties. Asthma, often confused with bronchitis, croup, or allergies, is a significant chronic illness causing school absenteeism, as per the CDC. Risk factors include prenatal smoking and family history of allergies or asthma. Infants and toddlers are more susceptible due to smaller airways and respiratory viruses, which can exacerbate conditions like colds and bronchitis. How can I tell if my child has asthma? Unfortunately small children are unable to describe their symptoms, making asthma difficult to diagnose. Your child may even be active, playing and smiling, although they are experiencing chest tightness or labored breathing. Observe your child and let the child’s doctor know if: Your child’s breathing behavior has changed (coughing, wheezing, rapid breathing) Your child’s breathing pattern changes (day vs. night, with rest or activity, inside vs. outside) You have a family history of asthma or allergies Your child’s breathing is triggered by any foods or allergies With your help, your child’s doctor can make the best diagnosis to determine if your child has asthma. A pediatric pulmonologist (lung specialist) or pediatric allergist may also have to be consulted for special testing. Tests may include lung function testing, allergy tests, blood tests and X-rays for an accurate diagnosis. What is the treatment for infants and toddlers? Young children can use many of the same medications as older children and adults, although the way they take them and the dosage will differ. A nebulizer (or breathing machine) creating a medicated mist for your child to breathe through a mask may be used. An inhaler with a small spacer tube connected to a mask is also common to help your child breath medication into their lungs. Either of these options are effective. Asthma in children is treated with both fast-acting and long-term medicines to open up airways quickly for easy breathing and also to lessen asthma symptoms over time. Communicate with your child’s medical providers to create a personalized asthma management plan for them. How can I manage my child’s asthma? Recognize your child’s breathing habits and be aware of worsening symptoms. Consult with your child’s doctor on a daily asthma action plan to recognize worsening symptoms and track medications. Here’s an example of an asthma action plan provided by the U.S. Department of Health and Human Services’ National Institutes of Health). Be consistent with the plan and talk to your doctor before changing it. Have an emergency plan in case of a serious asthma attack. Know where the closest ER is and know who can take care of your other children. Also know what the medical treatment coverage is under your insurance plan. Dr. Singh explains, "Discussing asthma with your child may be difficult. Some kids find the subject frightening or confusing. Others, especially the older kids, may resent the treatment and may not be interested in doing it. Talk to your doctor about advice to build an open and trusting relationship regarding your child's asthma care."
-
3 Ways to Enroll in a Hometown Health Insurance Plan
Are you looking for health insurance coverage for the upcoming year? In that case, it's time to browse your options for an Individual or Family Plan. The Open Enrollment Period is from Nov. 1, 2023 until Dec 15, 2023. So, if you're looking for coverage by Jan 1, 2024, you must enroll by Dec 15, 2023. Get a Quote Online Suppose you don't qualify for a health insurance subsidy, no need to worry! You can still choose an individual and family health insurance plan from Hometown Health. Get a quote online by providing your location, the type of coverage you're looking for and your personal/family details. Once you've provided this information, you'll receive health plan options and pricing. And, if you find a plan you like, you can easily self-enroll online. Get Your Online Quote Today Enroll Through the Nevada Health Link Hometown Health offers Individual and Family health insurance plans on Nevada's Healthcare Marketplace, the Nevada Health Link. Through Nevada Health Link, eligible Nevada consumers can shop for, compare and purchase quality and affordable health insurance plans with ease. Nevada Health Link is the only health insurance resource that can provide eligible candidates with federal tax credits and subsidies to help cover the cost of your health insurance. Use Hometown Health's Insurance Subsidy Federal Poverty Level Calculator to see if you qualify for a tax credit or subsidy. Enroll via Nevada Health Link Work with a Health Insurance Broker Hometown Health is northern Nevada's local insurance provider and if you have questions about Individual and Family Plan insurance benefits, you’re in luck! Hometown Health partners with our local health insurance brokers who will work with you, typically at no cost, to help you understand health insurance plans and benefits and find the plan that is best for you. Need assistance finding a broker? Connect with our team by submitting the form below. They'll provide you with a list of our local broker partners. Find a Broker Near You
Read More About 3 Ways to Enroll in a Hometown Health Insurance Plan
-
Guide to Injury Healing: Heat or Ice?
Heat and ice are two of the most common treatments used to relieve pain and reduce swelling in injuries. However, each one is better suited for certain types of injuries Dr. Luis Palacio, MD explores the differences between the two. When it comes to treating aches and pains, the debate between heat and ice has been ongoing for quite some time. Both have their benefits making it crucial to understand which option is better suited for your specific needs. Determining which method is better depends on various factors such as the type of injury or pain you are experiencing. For instance, if you have recently sprained your ankle or pulled a muscle during exercise, applying ice within the first 48 hours can help minimize swelling and alleviate discomfort. It's worth noting that some individuals find alternating between heat and ice therapy beneficial as well. This approach combines the benefits of both methods by using heat to increase blood flow followed by ice to reduce inflammation. Cold Therapy Cold therapy can help to reduce inflammation after an injury, heat can have the opposite effect. Therefore, heat therapy should be reserved for those who have chronic pain issues and are not dealing with an acute injury. Cold therapy is often recommended immediately after an injury or during the initial stages of inflammation. Cold therapy such as ice packs are especially effective in treating: Sprains Strains Any injury that involves swelling Heat Therapy Heat therapy is known for its ability to relax muscles, increase blood flow and soothe pain. It is often used for chronic conditions or injuries that are not inflamed. Applying heat can help alleviate stiffness, promote healing and provide a comforting sensation. This increased circulation can bring more nutrients and oxygen to the area, helping it to heal faster. Heat therapy such as heating packs are especially effective in treating: Stiffness with associated pain Injuries that are not inflamed Muscle pain
-
Why Your Teen Athlete Should See a Sports Medicine Doctor
Seeking specialized care for your teen from a sports medicine doctor is essential. Like a coach fine-tunes a player's skills, our experts fine-tune your teen's health, ensuring they stay at the top of their game. Luis Palacio, MD, a sports medicine physician with Renown Health, shares information to help young athletes safely push their boundaries and achieve their personal best. The Role of Sports Medicine Sports medicine is a specialized branch of healthcare that focuses on preventing, diagnosing and treating injuries related to physical activity and sports. Renown's Sports Medicine team consists of skilled professionals passionate about keeping young athletes performing at their peak while minimizing the risk of injury. With a comprehensive approach to care, our sports medicine doctors provide tailored guidance and solutions to help your teen reach their full potential. Injury Prevention and Education Prevention is the key to maintaining a long and successful athletic journey. Our sports medicine doctors collaborate with young athletes to educate them about proper warm-up techniques, body mechanics, and techniques to prevent overuse injuries. From understanding the importance of rest days to practicing correct form, our experts empower teen athletes with the knowledge they need to stay in the game.
Read More About Why Your Teen Athlete Should See a Sports Medicine Doctor
-
6 Healthcare Action Items for the LGBTQIA+ Community
© Niyazz via Canva.com Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
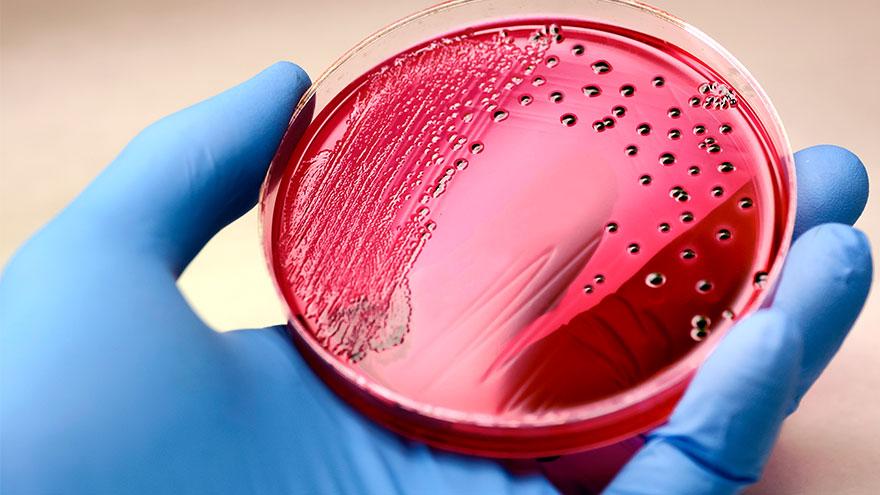
Sepsis: Causes & Symptoms
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.