Buscar
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
Departamento destacado: Special Procedures
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
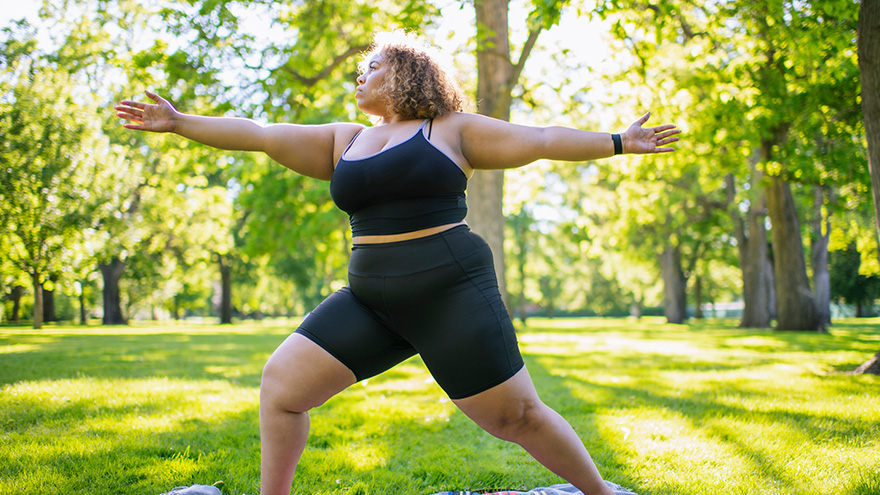
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
How to Treat a Sprain or Strain
Injuries happen to everyone. They are caused by participating in sports, recreational activities like hiking, and even by accidentally stepping off a curb wrong. If you experience a sprain or strain, the first few days are often the most painful. Renown Sports Medicine physicians Luis Palacio, MD and Brandon Hockenberry, MD walked us through what to do after an injury. Listen to Your Body See a medical professional right away if: You know or suspect that a bone is broken You are having difficulties putting full weight on a joint of the leg Pain or swelling is severe There is a sign of an infection, such as redness and warmth in the joint The First 24-72 Hours Joint sprains tend to swell more than muscle strains. You can use ice as needed for comfort and to relieve any pain, but do not use ice for more than 15-20 minutes at a time. Ice and NSAIDs (such as ibuprofen) can help prevent excessive swelling and mask the pain, but they do not speed recovery. Some research shows that overuse of ice actually delays recovery. During the first 24-72 hours, your injury will go through an inflammation phase. Inflammation is your body’s natural way to dispose of dead tissue cells, build new healthy structures, and hopefully heal even stronger than before.
-
How to Manage and Prevent Tendonitis
Tendonitis occurs when a tendon in your body is inflamed or irritated. This painful condition can impact your day-to-day activities, but can be managed and prevented. Luis Palacio, MD, shared some insights into how to manage tendonitis. Overuse and Repetitive Motion Tendons are complex tissues in our body that connect muscles to bones, allowing us to move. Unfortunately, sometimes these tendons become inflamed, worn down or injured, a condition called tendonitis. Symptoms of tendonitis include pain or dull ache, tenderness and mild swelling at the site. While tendonitis can be caused by a sudden injury, it is more commonly seen in frequent motions, including: Repetitive motions in exercise, work or other physical activities. Awkward positions in a movement, including poor posture. Forced movements that strain your body. Sudden increase in frequency of movement or level of difficulty, including little to no recover time between new activity. Shoes without proper support or hard surfaces, such as concrete floors. Evaluation is Key If you suspect that you have tendonitis and it does not resolve on its own after a few days, you should get it evaluated by a primary care or sports medicine doctor. They can make recommendations to aid your recovery and refer you to the right sub-specialist if needed. With some intentional actions, you can help reduce the risk of tendonitis with the following suggestions: Add variety: Mixing up the type of exercise you do will help prevent repetitive motions that can result in overuse. Stretch and condition: Make sure the keep up with proper stretching and muscle strengthening to support your physical activities. Do it right: Make sure that the way you are completing exercise or work-related physical activities is correct. Seek out a professional for lessons or guidance if you are unsure.
-
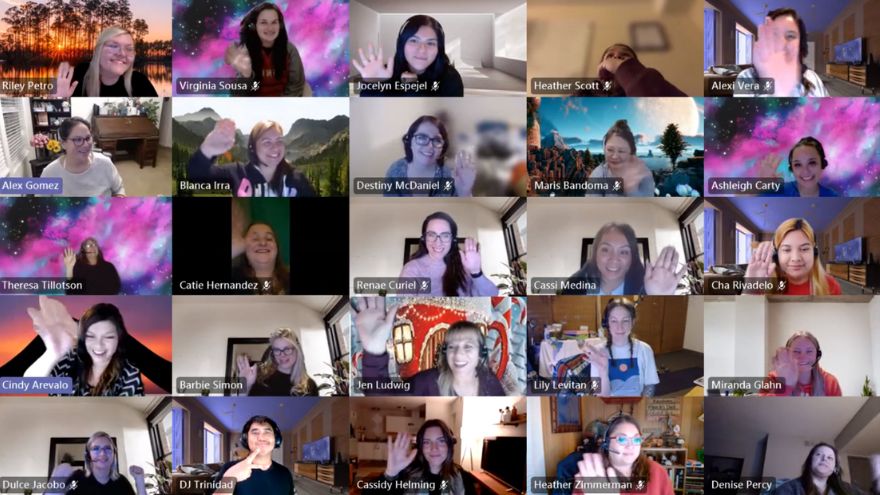
Departamento destacado: Customer Engagement Center
Do it for the patient. That’s the motto that each employee in the Customer Engagement Center (CEC) lives by every single day. This team spins all the existing stereotypical thoughts about call centers on their side by empowering and partnering with patients to achieve their best health. Being transferred around several times just isn’t in this team’s DNA – being a one-stop-shop for patient scheduling, referrals, insurance matters and more is how they proudly operate. Through elevating the customer engagement experience, the CEC closes care gaps to ensure patients get the right care at the right time. From employees who work from our home base in Reno, all the way to the southeastern corner of Florida, this primarily remote team stays firmly connected and collaborative to make patient care possible for all Renown Health patients and Hometown Health and Senior Care Plus members. The “Make It Happen” Department Back-to-back phone calls about a wide variety of patient needs? They make it happen. Referrals that need to go directly to the provider? They make it happen. Complex insurance questions that need to be resolved? They make it happen. The CEC is the keeper of all things customer service and all things patient satisfaction, leveraging technology to improve engagement and accessibility – and they wear that badge with pride. “Patient care is our first priority,” said Cindy Arevalo, Supervisor of Customer Engagement. “Even though we aren’t face-to-face with them, we are always there to help them over the phone with whatever their needs are.” The CEC has a lot of different sub-departments under its umbrella: scheduling, referrals, insurance, patient outreach, personal assistants, MyChart customer service and more. Each team handles calls for a different section of our health system, including the hospitals, imaging, primary care and specialty care. While their individual teams may be different, one aspect of their jobs remains the same: they care. Deeply. “We advocate for the patient, especially when they can’t advocate for themselves,” said Amanda Ishii, Referral Specialist. “We are the first people that patients speak to, and we all have empathy to listen to them, help them solve their problems and take as much time as they need to care for their needs,” added Susana Arroyo Garcia, Supervisor of Customer Engagement. Customer loyalty is key to the CEC. Every CEC team member builds strong relationships with patients and members. Whether they manage patient outreach or manage back-to-back inbound calls, each employee feels a special connection to the helpful work they do to solve a variety of patient concerns. “As Senior Care Plus Personal Assistants, for instance, we help guide our members through complex situations, and we eliminate the process of transferring them to different departments, becoming a ‘one-stop-shop' for them,” said Stephanie Perez Campbell, Senior Care Plus (SCP) Health Coordinator. “While every day is different, we are constantly learning new things and helping members navigate through the health system." With the 4.5 million calls the CEC handles per year, the nature of their jobs is undoubtedly fast paced. However, this does not intimidate the CEC team members; instead, it inspires them to continue reaching new milestones, helping thousands of patients and members every year by handling all the scheduling and referral work on the backend so that they can receive the care needed. “I never find myself sitting around asking, ‘what should I do next,’” said Gina Briles, Supervisor of Customer Engagement. “We always support each other to stay on top of it all in order to take care of our patients.” By wearing a lot of hats and managing many different work queues all while staying engaged with each patient, the CEC is full of natural problem-solvers, helping our healthcare network run smoothly. “The Engagement Center is the front door for the community; serving as the voice of the customer, we ensure patients do not fall through the cracks of the complex healthcare system and are able to easily access the right care at the right time through an exceptional experience,” said Candace Dietrich, Director of Customer Engagement. Consistently Connected With thousands of referrals to process and millions of calls to field, the ways the CEC stays connected to patients and members as well as each other can be related closely to magic. No concern goes unnoticed, and no problem is too complicated. “The sheer volume of patients we engage with is incredible,” said Rene Jacinto, Manager of Customer Engagement. “We processed nearly 200,000 referrals and authorizations last year.” “We expect a steady increase of calls year-over-year. My team processed 1,259 referrals in one day alone recently,” added Arielle Gomes, Referral Specialist. A superpower that every CEC team member holds is the ability to listen. According to this department, active listening is key when problem-solving with every patient and member, as that skill helps them anticipate patient needs and resolve their issues quickly and efficiently. “I’ll always listen,” said Alex Gomez, Customer Engagement Representative. “I want them to know that they are in good hands, especially when they are feeling scared or frustrated.” Team members like Alex help carefully guide customers through the Hometown Health and Senior Care Plus enrollment process, increasing membership and engaging patients to find the perfect plan for them. One of the largest challenges the CEC faces is the departures and arrivals of providers. The ebbs and flows of all hospital systems include provider departures and shifting provider availabilities. Despite this challenge, the CEC staff work hard to ensure communication with all patients regarding provider changes is consistent and that all patients are scheduled in a slot that works for both their schedule and the provider’s schedule. “It’s important for us to be flexible, because things can change at a moment’s notice,” said Gina Briles. “This is more than just a job – we are here for our patients. What we are doing impacts everyone.” Throughout all times of transition, the CEC builds robust relationships with both patients and providers within our organization and community, a skill that this team emphasizes as “fundamentally important.” For example, SCP Personal Assistants like Stephanie Perez Campbell will coordinate care with community resources and offices, giving members one less call to make and one less hurdle to cross in order to get the care they need. On top of it all, even though this team has the ability to work from all 50 states (and many of them work outside of Nevada!), every employee feels connected to their colleagues and their work. “This is the best group of people I’ve ever worked with,” said Riley Petro, Manager of Customer Engagement – Imaging. “I am super lucky for this job and am so thankful for these people.” Proud and Powerful The proof is in the pudding – or rather, the proof is in the numbers. Within the 4.5 million calls they successfully field every year, approximately 1.6 million of those calls route through the private branch exchange (PBX) team – the team that oversees the main operator lines – under the guidance of Jess Nater, Supervisor of Customer Engagement. The CEC is also on track to handle nearly 300,000 referrals this year alone. Additionally, the Hometown Health CEC team was recognized nationally this year with a five-star rating from Medicare. “We all have the initiative to grow, and because of this, we are always learning something new,” said Cindy Arevalo. “Our leaders also support our growth, especially if we want to skill-build or advance in our careers.” The CEC is frequently the first stop on the career ladder for many employees as they start their journey in healthcare, and CEC leadership is committed to the growth and development of their teams to reach their career goals at Renown. The secret formula for all this success can be in part attributed to the pride each CEC employee has for their team, their work and Renown. “We have a very supportive team,” said Holly Coffey, Supervisor of Customer Engagement. “I’ve seen our leaders support their teams tremendously.” “We rely on each other,” added Ashleigh Carty, Customer Engagement Representative. "I love the relationships we create with one another.” Employees in the CEC come from many walks of life, choosing to work at Renown and Hometown Health for a variety of different reasons, many related to the positive power our health system holds. Team members in this department hold a myriad of different career backgrounds, including pharmacy technicians, medical assistants, population health professionals, community health workers and more. Some team members, like Nikki Clifford, Customer Engagement Representative Lead, heard wonderful things about Renown from her mother, who also works for Renown. According to Nikki, “seeing how happy my mom has been in her career made me want to join too. I’ve loved it here ever since.” Katie Lunau, Supervisor of Customer Engagement, also grew up in a family involved in healthcare, and she wanted to follow in their footsteps. Choosing Renown as the place to follow her family path was a simple one, because “Renown stood out as the company that was actively involved in the community helping others.” For other team members, like Susana Arroyo Garcia, Ashleigh Carty and Stephanie Perez Campbell, Renown and Hometown Health’s impact on the local healthcare landscape was their primary driver for choosing a career here and in the CEC specifically. “Renown is very well-known in the area,” said Stephanie Perez Campbell. “I went to school in Reno for public health, so Renown came up all the time in my schooling. I knew Renown had a lot of different opportunities available for career growth, and with the friendly environment I always experienced here, it was an easy decision.” “Once I went through the interview process and joined the team, I immediately realized that there are outstanding managers, support systems and communication skills here. People genuinely care,” added Ashleigh Carty. Ashleigh is exactly right. As emphasized by every team member, employees in the CEC care. Their heightened levels of care and empathy set the bar high for all at Renown and Hometown Health, and their impact will be felt for years to come.
Read More About Department Spotlight: Customer Engagement Center
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
Keeping Kids Safe on Halloween
Halloween is around the corner. So while you're prepping pumpkins for carving, putting together creative costumes and coordinating trick-or-treating plans, safety is one more detail to remember. Masks, haunted houses, witches, ghosts and ghouls — it all spells Halloween, and what could be more frighteningly fun, right? For children, however, Halloween can indeed be frightening and not so fun. According to Dr. Kristina Deeter, Physician-in-Chief of Renown Children’s Hospital and Chair of Pediatrics for the University of Nevada, Reno School of Medicine, it is common for younger children to express Halloween fears — being afraid of monsters, the dark or really anything out of the norm. “It's normal for children to struggle with separating reality from fantasy,” she explains. For children who fall into this category, the month of October can be traumatizing. Halloween may not come until the end of the month. Still, in the weeks building up to the spookiest night of the year, little ones are bombarded on all sides with decorations — mummies, skeletons, coffins, vampires, you name it. For a child with a blossoming imagination who, as Dr. Deeter said, is still learning to differentiate real from pretend, this can cause additional fears and anxieties. In commemoration of Halloween Safety Month, Dr. Deeter shares safety tips for the spooky holiday from the American Academy of Pediatrics: Dressing Up & Heading Out Plan costumes that are bright and reflective. Ensure shoes fit well and that costumes are short enough to prevent tripping, tangling or coming into contact with flames. Consider adding reflective tape or striping to costumes and trick-or-treat bags and baskets for greater visibility. Masks can limit or block eyesight. Instead, consider non-toxic makeup and hats, which should fit properly to prevent them from sliding over the eyes. Test makeup ahead of time on a small patch of skin to test for allergies before full application. When shopping for costumes, wigs and accessories, look for and purchase those with a label clearly indicating they are flame resistant. If a sword, cane or stick is a part of your child's costume, make sure it is not sharp or long. A child may be easily hurt by these accessories if he stumbles or trips. Do not use decorative contact lenses without an eye examination and a prescription from an eye care professional. While the packaging on decorative lenses will often make claims such as "one size fits all," or "no need to see an eye specialist," obtaining decorative contact lenses without a prescription is both dangerous and illegal. This can cause pain, inflammation, serious eye disorders and infections, which may lead to permanent vision loss. Review with children how to call 9-1-1 (or their local emergency number) if they ever have an emergency or become lost. Carving Pumpkins Leave the carving to the grownups. Have children draw the pumpkin design with markers, but keep knives away. Consider using a flashlight or glow stick instead of a candle to light your pumpkin. If you do use a candle, a votive candle is safest. Candlelit pumpkins should be placed on a sturdy table, away from curtains and other flammable objects, and not on a porch or any path where visitors may pass close by. They should never be left unattended. Prepping Your Home Keep your entryway safe for trick-or-treaters by removing all items from the porch or front yard that a child could trip over, like garden hoses, toys, bikes and lawn decorations. To ensure visibility, check outdoor lights and replace burned-out bulbs. Sweep leaves (or snow) from sidewalks and steps. If there are dogs in the home, take steps to ensure they don't jump on trick-or-treaters. Hunting for Treats Young children should always be accompanied by a parent or responsible adult. Give each child and adult a flashlight (with fresh batteries). If older children are heading out to trick-or-treat alone, plan and review a route you can agree on, as well as a specific time they are supposed to return home. Only visit homes with a lit porch light. Never enter a home or a car for a treat. Notify law enforcement authorities of any suspicious or unlawful activity immediately. Since pedestrian injuries are the most common injuries to children on Halloween, remind youngsters to take crosswalk safety precautions. For more key tips regarding Halloween safety for your young trick-or-treaters, visit our partners at Safe Kids Worldwide for a variety of spooky safety resources.
-
Meet Gabby, Renown Regional ER Nurse and Miss Rodeo Nevada
Renown Health is proud to embrace the Reno-Sparks culture that makes our community stand out, which is why we sponsor the Reno Rodeo, an early summer staple with roots in the community as deep as our own. One of our many ties with the Reno Rodeo includes Renown Regional’s own emergency room nurse and Miss Rodeo Nevada 2022, Gabby Szachara. A Reno native, Gabby developed a love for the Reno Rodeo at a very young age. “I loved watching the girls on the Reno Rodeo Flag Team when I was little and knew I wanted to be part of the Reno Rodeo someday,” said Gabby. “As I got older, I started to make connections and build relationships with some people in the rodeo scene, and they generously lent me their horses so I could participate in the Reno Rodeo Flag Team.” Gabby was on the flag team for three years before being crowned Miss Rodeo Nevada 2022 last year. Before joining the Reno Rodeo Flag Team, Gabby was a student at the University of Nevada, Reno, and a member of the women’s volleyball team. In December 2017, she graduated with a bachelor’s degree in public health. At first, Gabby was interested in a career in sports medicine – it made sense with her background in athletics. But, after working in the medical field as a certified nurse assistant and an emergency medical technician, she grew passionate about patient care and decided she wanted to become a nurse. “I’ve always loved teamwork and helping others,” said Gabby. “It’s important to me to be there for others, especially when it might be their worst day.” In December 2021, Gabby graduated from Truckee Meadows Community College with a nursing degree and joined Renown Health this February. “I love Renown for various reasons. Everyone here is so nice and welcoming, and there is a great team dynamic,” said Gabby. “And I love that Renown’s main color is purple because that is my favorite!” When Gabby isn’t in her scrubs and caring for patients, she is in western wear and carrying out her duties as Miss Rodeo Nevada. “I do a lot of traveling across the country to attend other rodeos,” said Gabby. “I enjoy meeting so many wonderful people and experiencing the culture of different states.” Gabby’s main goals as Miss Rodeo Nevada are to promote the western way of life, agriculture, rodeo and community benefit. In addition, she visits local schools to talk with kids about how they can get involved in these areas and inspires them to turn their dreams into reality. Gabby has a special place in her heart for the Reno Rodeo. “Reno is my home, and the Reno Rodeo is the heart and soul of summer in northern Nevada. Everyone comes together and dusts off their boots to have fun and also contribute money to important causes in our community,” said Gabby. “I love the comradery, the friendly and healthy competition and the great people.” If you’re going to the Reno Rodeo this weekend, watch for Gabby and her horse, “Torque.” And if you see Gabby in the halls at Renown Regional, give her a high-five for all her hard work as a nurse and Miss Rodeo Nevada!
Read More About Meet Gabby, Renown Regional ER Nurse and Miss Rodeo Nevada
-
La historia de Paola: incorporar la esperanza y la determinación en el cuidado del paciente
You may recognize her from billboards around town or the cover of Renown's latest annual report, but what you might not know is the story behind the now-familiar face. Paola Espinoza-Patino is the oncology unit's associate nurse manager at Renown Regional, and she grounds her work in hope and determination daily. Meet Paola:
Read More About Paola’s Story: Bringing Hope and Determination to Patient Care
-
Alzheimer’s Disease – How to Spot the Signs
Alzheimer’s disease is not normal forgetfulness as we age. Instead, it is a specific form of mental decline. And according to the Alzheimer’s Association it accounts for nearly 80 percent all dementia cases. Natasa Dragicevic, MD, PhD., behavioral neurologist and Alzheimer’s disease specialist with Renown Institute for Neurosciences, weighs in on diagnosing it and the importance of early medical action. How to Diagnose Alzheimer’s Disease In general, the signs of Alzheimer’s disease occur slowly, getting worse over time. For example, forgetfulness is a daily search – for shoes, keys and other misplaced items. Not only is memory affected, but also speech patterns and behavior. There is no single test for Alzheimer’s disease. “Specifically, a neurologist should be the one to diagnose Alzheimer’s disease given differences in presentation,” clarifies Dr. Dragicevic. “And ideally a behavioral neurologist (Alzheimer’s sub-specialist) will be managing the treatment,” she adds. Brain Imaging Diagnosing Alzheimer’s disease involves multiple approaches and medical providers. In short, medical history is reviewed along with a physical exam, lab tests and other diagnostic testing. “A medical workup includes a variety of tests. These include MRI and other brain imaging, as well as neurological and psychological testing. Furthermore, a lumbar puncture is performed to look for markers of the disease,” she states. What Causes Alzheimer’s disease? Although no one knows the cause, researchers think many factors play a role. Uncontrollable risk factors include your genetics and having a family member with the disease. However, the controllable risk factors include: reducing the risk of head injury and keeping your heart healthy. It’s important to realize that high blood pressure, high cholesterol, stroke and diabetes play a role in brain health. Blood loss to the brain causes vascular dementia, leading to long-term blood vessel damage. Symptoms of Alzheimer’s disease Generally speaking, the signs of this disease differ in each person. Yet noticeable behaviors include: • Losing the way to familiar places • Forgetting to pay bills • Trouble finding the right words when talking • Repeating questions • General confusion • Social withdrawal Alzheimer’s Disease – Benefits of Early Diagnosis Equally important, spotting Alzheimer’s disease early allows more time to benefit from medications and possible clinical trials. Likewise, nutrition and exercise changes can be made, increasing blood flow to the body, and perhaps delaying symptoms. Early diagnosis also allows for personal health decisions and quality-of-life conversations to take place. According to the Alzheimer’s Association, these benefits include: 1. Medical advantage 2. Emotional and social comfort 3. Time to plan ahead 4. Cost savings A Brain Supporting Lifestyle “At the present time, treatment is limited,” explains Dr. Dragicevic. “Usually Alzheimer’s is a progressive ongoing disease – any management at this time is purely symptomatic.” However, she states the following lifestyle changes can help support brain health: • New hobbies such as painting, pottery, music classes or learning a new language • Crosswords, puzzles and playing games, such as Scrabble • Brain challenging mobile apps, such as Luminosity • 30-45 minutes of mild to moderate physical activity per day, such as walking • Eating a Mediterranean diet (primarily plant based foods)
-
¿Es la cirugía bariátrica adecuada para usted?
You’ve likely heard about bariatric surgery — and perhaps even have friends who’ve done it. But is it a potential solution for you? Here, Dawn Remme, RN, Metabolic Bariatric Surgery Program Manager, provides insight. You may have been struggling with excess weight for years. You’ve tried high-protein diets, low-carb diets and more. Most patients considering weight loss surgery have tried numerous dieting methods. The truth is, some patients who suffer with obesity are successful dieters. Unfortunately though, excess weigh often returns. This impacts their health and the quality of their life. It can be a disheartening battle. Weight loss surgery is a big decision. In making this decision, keep in mind that surgery is only one step toward your goal of achieving better health. It is neither magic, nor is it the “easy way out.” Weight loss surgery can offer you a TOOL to help you become more successful in controlling the disease of morbid obesity. By combining this tool with a lifelong commitment to important lifestyle changes, medical follow-up and nutritional modifications, you have the potential to become a healthier you. Bariatric Surgery By the Numbers Exploring the facts about obesity, how it impacts your health, and how surgery can resolve or significantly improve your chronic medical conditions is the first step to making a decision. Obesity is medically defined as “excess body fat” and is measured by a mathematical ratio known as the Body Mass Index (BMI). To calculate your BMI, we consider your height, weight, age, gender and body build. Here are the standards: “Normal” BMI: less than 25 Overweight: 25 – 29.9 Obese: BMI of 30 – 39.9 Morbid obesity: BMI of 40 or more Morbid obesity (BMI over 40) is a lifelong, progressive disease, and the prevalence of morbidly obese Americans (100 or more pounds over a healthy weight) is increasing rapidly. According to the CDC, the disease of obesity affects 78 million Americans. Further estimates indicate about 24 million have morbid obesity. Serious medical problems known as co-morbidities often occur when someone is morbidly obese. Studies tell us conditions such as type 2 diabetes, high cholesterol, sleep apnea, high blood pressure and degenerative arthritis increase in severity as the BMI is increasing in patients. When may weight loss surgery be an option? When someone has a BMI greater then 40. If a person’s BMI is 35 – 39.9 and they have significant health problems such as type 2 diabetes, high blood pressure, high cholesterol, sleep apnea, or other diagnosed health conditions related to obesity. Gastric Sleeve, Gastric Bypass Explained To resolve or significantly reduce these health conditions, bariatric surgery can be done when diet and exercise haven’t worked. Weight loss surgery makes changes to your digestive system to help you lose weight. The gastric sleeve limits how much you can eat, whereas gastric bypass limits how much you can eat and reduces the absorption of certain nutrients. Other Benefits of Surgery You can greatly increase life expectancy by resolving or significantly improving conditions like diabetes, high cholesterol, high blood pressure, sleep apnea, and obesity itself. Infertility can also be positively affected. A significant weight loss and relief from serious health conditions and diseases will greatly improve your quality of life. Studies tell us that type 2 diabetes is resolved or significantly improved in 84 percent of patients following bariatric surgery. Cholesterol levels dropped in 95 percent of patients. And hypertension and sleep apnea showed improvement in 68 and 80 percent of patients, respectively, following bariatric surgery. Bariatric Surgery at Renown In making the decision to move forward to better health, it is important to remember: Obesity is a disease, and the desire to have a healthier, longer, more fulfilling life is possible. If you are interested in learning more, please visit the Bariatric Surgery Program page to view more information about Renown Regional Medical Center’s MBSAQIP accredited bariatric program, as well as information about upcoming educational seminars. Or call 775-982-RSVP (7787) to reserve your seat. Learn More