Buscar
-
Why Am I So Tired? 9 Reasons for Your Chronic Exhaustion
Do you find yourself struggling to stay awake during the day or having no energy? You’re not alone. Whether you’re a full-time employee, a student or retiree, that “I’m tired” feeling comes in all shapes and sizes. What’s even more frustrating is not knowing the source of your exhaustion. Dr. Brandon Flores, a sleep medicine physician with Renown Medical Group, breaks down nine key reasons why you may be feeling so fatigued. You did not get enough sleep, or your quality of sleep is poor. This may seem obvious, but in today’s “rise and grind” culture, sleep can be considered a luxury rather than what it really is: a necessity. Ensuring you get adequate hours of sleep between 6-9 hours and quality sleep is essential. You may not be breathing well during sleep. Interruptions to your breathing, such as snoring, can decrease airflow at night causing your sleep to be less restorative. This is often due to Obstructive Sleep Apnea (OSA). OSA can lead to daytime fatigue and sleepiness and can also impact other chronic health conditions, such as hypertension, diabetes, acid reflux, migraines and heart rhythm. You are not getting enough regular exercise, or you are exercising too much. Incorporating at least 30 minutes a day of physical activity can help keep you energized throughout the day. It has also been shown to increase deep slow wave sleep, which is often associated with feeling rested. On the other hand, getting too much exercise can tire you out more easily and heighten stress levels. You drink too much caffeine. This one may seem counterintuitive – caffeine is supposed to keep you awake, right? Well, overdoing it with your favorite coffee or soda could affect your sleep quality. Pay attention to your caffeine limits and have a cut-off time, as most caffeine should not be consumed past noon. You have a food allergy or intolerance. If you find yourself feeling especially tired after eating a lot of a certain food, you could have an allergy or intolerance to it – and vice versa. Consider speaking with your primary care provider (PCP) about a food allergy test or being referred to an allergist. You’re drinking too many alcoholic beverages. Alcohol is a depressant, which as the word implies, can make you feel especially tired during the day. It can also affect your breathing at night and disrupt your sleep cycle. Cutting back on alcoholic drinks may be beneficial to your overall health. You are anemic. This is the leading cause of fatigue in women but can affect people of all genders. It can be associated with low iron. Eating foods high in iron, including leafy greens and many different meats, can help your iron levels. A blood test ordered by your PCP can help you understand if you are iron deficient. You are experiencing depression or anxiety. Emotional exhaustion can be just as taxing as physical exhaustion. Prolonged feelings of sadness, hopelessness, nervousness or panic can be signs and symptoms of depression or anxiety. Speak with your provider about the many resources available to help you. You have an underactive thyroid. Feeling fatigued can also be a symptom of hypothyroidism, which affects your metabolism and energy levels. Medication can help get your thyroid back to normal. Your PCP can order a blood test to determine your thyroid levels. If you experience severe exhaustion that lasts six months or longer, worsens after physical or mental exertion and does not get better after resting, it could be a sign of myalgic encephalomyelitis, otherwise known as chronic fatigue syndrome (CFS). This is a diagnosis of exclusion, and other causes must be ruled out. While there are no tests that detect CFS, your provider can order blood and urine tests to rule out other causes of your fatigue and help develop a care plan.
Read More About Why Am I So Tired? 9 Reasons for Your Chronic Exhaustion
-
Departamento destacado: Special Procedures
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
COPD Explained: Protecting Your Lungs and Managing Symptoms
COPD (chronic obstructive pulmonary disease) is a progressive lung condition often mistaken for typical aging signs, like shortness of breath and coughing. While smoking and pollution can contribute to its development, lifestyle changes and medications can help manage its progression. Diagnosis typically involves lung function tests, chest X-rays, or CT scans, with treatments available through a pulmonologist or primary care provider. Renown’s Pulmonary Rehabilitation Program offers insights into living with COPD. What is COPD? According to the COPD Foundation, it is an umbrella term used to describe progressive lung diseases including: Emphysema: Damage to the small air sacs in the lungs (alveoli). Chronic Bronchitis: Irritation and swelling of bronchial tubes, causing shortness of breath and coughing for long periods of time. Asthma (non-reversible): When asthma medications cannot reduce swelling in the airways. COPD Risk Factors Smoking is the most significant COPD risk factor, and the American Lung Association (ALA) says it accounts for nearly 90 percent of cases. If you are a smoker, it is essential to seek help and quit. Other COPD risk factors include: Air pollution Genetics Second-hand smoke Chemical, fumes or dust in the workplace How Can You Protect Yourself? Stop smoking Renown Health provides support offering 4-week Smoking Cessation Virtual Classes, free of charge! Sign up today. Use natural cleaning products Many household chemicals, especially those containing bleach, can irritate the lungs – a condition called, chemical pneumonitis. Stay away from all types of smoke This includes smoke from fireplaces. Likewise, plan to stay indoors when it is smoky outside, or air quality is poor. Get active Of course, it’s never too late to start an exercise program. When exercising your heart pumps, circulating your blood and sending oxygen to every part of your body. Notably it strengthens your lungs, making it easier to breath. Talk to your doctor to see if you are healthy enough to begin exercising. Eat a healthy diet Surprisingly what you eat can affect your breathing. The American Lung Association encourages those with COPD to watch their sodium intake, eat smaller, more frequent meals (instead of three large ones), limit high fat foods and drink plenty of water. Avoid scented products Perfumes, aerosol sprays and plug-in air fresheners can trigger flare-ups. Get a flu shot Did you know chronic lung conditions, as well as, heart disease, cancer and diabetes, can be made even worse by the flu? Now is the time to get your flu shot for the season if you haven’t already. Renown’s Pulmonary Rehab staff is certified through the American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR). Recently, Renown Regional Medical Center successfully completed a disease specific COPD certification survey by The Joint Commission. For two accreditation cycles in a row, the COPD Program has had zero findings during the rigorous survey.
Read More About COPD Explained: Protecting Your Lungs and Managing Symptoms
-
Celebrating World Lung Day in Northern Nevada
In the United States, electronic cigarettes are the most popular form of tobacco product used among high school students. Approximately 21% of Washoe County area high schoolers report current use of e-cigarettes, higher than the national average of 14% reported in the most recent national data. While often viewed as a safer alternative to traditional cigarette use, e-cigarette use, commonly referred to as vaping, exposes users to nicotine and harmful chemicals that stunt brain development, results in lung damage and harms overall health. In partnership with Reno area school principals and nurses, the Renown Health – UNR Med Clinical Research Office was able to provide this year’s World Lung Day Anti-Vaping Program to Galena High School, Robert McQueen High School and Sage Ridge School, reaching hundreds of high school students.
Read More About Celebrating World Lung Day in Northern Nevada
-
Guide to Injury Healing: Heat or Ice?
Heat and ice are two of the most common treatments used to relieve pain and reduce swelling in injuries. However, each one is better suited for certain types of injuries Dr. Luis Palacio, MD explores the differences between the two. When it comes to treating aches and pains, the debate between heat and ice has been ongoing for quite some time. Both have their benefits making it crucial to understand which option is better suited for your specific needs. Determining which method is better depends on various factors such as the type of injury or pain you are experiencing. For instance, if you have recently sprained your ankle or pulled a muscle during exercise, applying ice within the first 48 hours can help minimize swelling and alleviate discomfort. It's worth noting that some individuals find alternating between heat and ice therapy beneficial as well. This approach combines the benefits of both methods by using heat to increase blood flow followed by ice to reduce inflammation. Cold Therapy Cold therapy can help to reduce inflammation after an injury, heat can have the opposite effect. Therefore, heat therapy should be reserved for those who have chronic pain issues and are not dealing with an acute injury. Cold therapy is often recommended immediately after an injury or during the initial stages of inflammation. Cold therapy such as ice packs are especially effective in treating: Sprains Strains Any injury that involves swelling Heat Therapy Heat therapy is known for its ability to relax muscles, increase blood flow and soothe pain. It is often used for chronic conditions or injuries that are not inflamed. Applying heat can help alleviate stiffness, promote healing and provide a comforting sensation. This increased circulation can bring more nutrients and oxygen to the area, helping it to heal faster. Heat therapy such as heating packs are especially effective in treating: Stiffness with associated pain Injuries that are not inflamed Muscle pain
-
Why Your Teen Athlete Should See a Sports Medicine Doctor
Seeking specialized care for your teen from a sports medicine doctor is essential. Like a coach fine-tunes a player's skills, our experts fine-tune your teen's health, ensuring they stay at the top of their game. Luis Palacio, MD, a sports medicine physician with Renown Health, shares information to help young athletes safely push their boundaries and achieve their personal best. The Role of Sports Medicine Sports medicine is a specialized branch of healthcare that focuses on preventing, diagnosing and treating injuries related to physical activity and sports. Renown's Sports Medicine team consists of skilled professionals passionate about keeping young athletes performing at their peak while minimizing the risk of injury. With a comprehensive approach to care, our sports medicine doctors provide tailored guidance and solutions to help your teen reach their full potential. Injury Prevention and Education Prevention is the key to maintaining a long and successful athletic journey. Our sports medicine doctors collaborate with young athletes to educate them about proper warm-up techniques, body mechanics, and techniques to prevent overuse injuries. From understanding the importance of rest days to practicing correct form, our experts empower teen athletes with the knowledge they need to stay in the game.
Read More About Why Your Teen Athlete Should See a Sports Medicine Doctor
-
6 Healthcare Action Items for the LGBTQIA+ Community
Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
Head Injuries, Sprains and Broken Bones
Participating in sports and physical activities is enjoyable and beneficial for our health. However, the risk of injuries comes with the fun and excitement of sports. Sports-related injuries, including sprains, traumatic brain injuries and broken bones, are more common than we realize and can land you in the emergency room. Dr. Scott Shepherd, Emergency Medicine Physician, provides a wealth of information. Traumatic Brain Injuries: The Invisible Threat Traumatic brain injuries come in many forms. From “mild” brain injuries, concussions, to major brain injuries and bleeds. Sometimes it is very difficult to tell the difference between a major injury and a minor injury because many of the symptoms are the same. Concussions Concussions are a type of “mild” traumatic brain injury resulting from a blow to the head or a violent shaking of the body that causes a transient alteration in mental function. They are particularly prevalent in contact sports such as football, soccer and boxing. A concussion can affect memory, judgment, reflexes, speech, balance and muscle coordination. Typically, concussions are not life threatening and usually short lived. However, multiple concussions can lead to permanent disabilities. So, remember there is nothing “mild” about injuring your brain. Contusions The more serious brain injuries from brain contusions (actual bleeding in the brain material) and bleeding that presses on the brain are life threatening. These injuries are caused by the same blow to the head as a concussion and the symptoms are the same from memory deficits, loss of coordination to coma. Because of this, anyone who has a blow to the head and is not acting normal should be evaluated by a medical professional. Anyone suspected of having a severe head injury should seek immediate medical attention and follow a strict protocol for rest and a gradual return to play. It is important to note a person may not lose consciousness if they suffer a concussion; however, major consequences can occur if not properly managed. If you suspect you have an emergency that needs immediate medical attention, please call 911 or visit an emergency room near you. While it is impossible to prevent traumatic brain injuries altogether, the severity of the injury can be mitigated through proper helmet usage and knowing your skill level when participating in high-risk activities. The guidelines for picking a helmet for summer activities such as mountain biking, dirt biking and riding off highway vehicles are similar to those of picking a helmet for winter sports. Learn more about choosing the right helmet. Any blow to your head, neck or upper body can result in a major head injury Signs to watch for include the following: Headache Dizziness Blurred vision Difficulty with thinking, attention or memory Sensitivity to noise or light Ringing in the ears Changes in hearing Double vision Changes in behavior Balance issues Nausea/vomiting Sprains: The Annoying Twist One of the most common sports injuries is a sprain, which occurs when ligaments that connect bones are stretched or torn. Sprains typically occur in joints, such as the ankle, knee or wrist, and are often caused by sudden twists or impacts. Symptoms may include: Pain Swelling Bruising Limited range of motion Rest, ice, compression and elevation (RICE) are the initial recommended treatment, followed by physical therapy to regain strength and mobility.
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Concussion Risks and Prevention
It’s important to be aware of the risk of a concussion, which can have serious health implications. Susan Park, MD, discusses the effects of concussions and how they can be prevented. According to Susan Park, MD, a Renown Medical Group doctor who specializes in sports and family medicine, concussions are a serious issue — especially among children whose developing brains “are more susceptible to brain injury and long-term effects from concussions.” All parents, coaches and athletes, she points out, should be aware of the risks of concussions and take precautions to avoid them. What is a concussion and how does it occur? Dr. Park describes a concussion as a traumatic brain injury resulting from direct or indirect impact to the head or body, during which the brain shakes back and forth in the skull. This may cause some bruising of the brain. In severe cases, traumatic head injuries can cause bleeding, which if not treated quickly, can be fatal. What are the health implications of a concussion? Symptoms of drowsiness and confusion can be a sign of a concussion after a head injury. Some short-term effects may include headaches, dizziness and difficulty concentrating. Long-term concerns can further include mood disorders, sleep disturbance and problems with cognitive function-concentration, which may affect school performance. What sports carry the highest risk of suffering a concussion? Dr. Park notes participation in any impact sport can result in a head injury. But among school-age kids, she treats more concussions from football and soccer than any other sport. However, during the winter months, skiing and snowboarding injuries can be a common cause of concussions Any blow to your head, neck or upper body can result in a concussion with symptoms including, but not limited to, feeling dazed or confused, dizziness, nausea/vomiting or a headache. Initial treatment of concussions varies depending on severity. Rest, avoiding vigorous activity and a reduced school workload help young athletes recover after a concussion. Dr. Park notes that sometimes further imaging and an ER visit will be required. Otherwise, rest from activities is the main treatment, along with not returning to sports activities until further clearance from a healthcare provider.
-
When Is It Time to See a Physiatrist
Physiatry (fi-zahy-uh-tree), also referred to as physical medicine and rehabilitation, encompasses the diagnosis, prevention and treatment of disabilities or injuries related to the brain, nerves, bones and muscles. The goal of this specialty is to maximize physical functioning, greatly decrease or eliminate pain, foster independence and improve quality of life for those suffering with a disability, chronic pain and physical impairments. Who Is It for? Physiatry can help patients with functional deficits and secondary medical conditions as a result of the following: Amputation Brain Injury Osteoarthritis Spasticity and Movement Disorders Spinal Cord Injury Spine Pain Sports-Related Injuries Stroke Some of these medical conditions can often cause chronic pain or impede physical functioning, ultimately affecting a person’s overall well-being and making it difficult for them to sustain a desired quality of life.
-
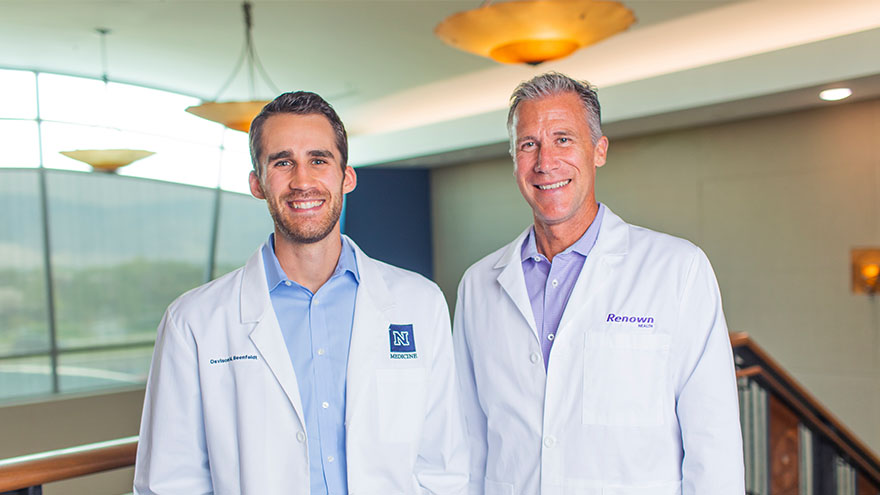
A Family's Legacy
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school