Buscar
-
How to Protect Your Kids from Heatstroke
Summer is around the corner, bringing heightened risks of heatstroke, especially for children who cannot regulate their body temperature as efficiently as adults. Infants are particularly vulnerable and may not express discomfort, so never leave a child unattended in a vehicle. Top Tips for Preventing Heatstroke Reduce the number of deaths from heatstroke by remembering to ACT. Avoid heatstroke-related injury and death by never leaving a child alone in a car, not even for a minute. And make sure to keep your car locked when you’re not inside so kids don’t get in on their own. Create reminders. Keep a stuffed animal or other memento in your child’s car seat when it’s empty, and move it to the front seat as a visual reminder when your child is in the back seat. Or place and secure your phone, briefcase or purse in the backseat when traveling with your child. Take action. If you see a child alone in a car, call 911. Emergency personnel want you to call. They are trained to respond to these situations Keeping Your Baby Cool in the Back Seat In hot weather, it is crucial to keep your baby cool and hydrated by using a car seat cover or towel over them to reflect the sun's rays. Dress your baby in lightweight clothing that covers their arms and legs. Keep an eye on your baby's skin color. Move them to a cooler place if they look too red or flushed. Keep the temperature at a comfortable temperature for you, not for your child. Keep the windows cracked open for ventilation and ensure nothing is blocking the airflow from entering or exiting the vehicle. Dress your infant appropriately for their environment, including appropriate head and neck coverings, to keep them cool and protected from sunburns. Ensure you have enough fluids to last an hour before getting out of the car or use bottled water if possible. Never leave your child unattended in a car. Steps to Follow if You Suspect Heatstroke Call 911 immediately. Cool the victim – Get the person to a shady area, remove restrictive clothing and cover skin with sheets soaked in ice-water, and place ice packs in the arm pits and groin. Have the victim drink cool fluids, preferably an electrolyte-containing sports drink. Monitor body temperature with a thermometer but stop cooling efforts after temperature has dropped to 102 Fahrenheit. Baby Safe Classes These classes help prepare parents for emergencies that may occur in baby’s first year. Safe Kids Worldwide Did you know heatstroke is the leading cause of non-crash related fatalities in children? “On average, every 10 days a child dies from heatstroke in a vehicle. In more than half of these deaths, the caregiver forgot the child was in the car.”
-
Why Childhood Immunizations Are So Important
Immunizations save thousands of lives each year by preventing serious illnesses, hospitalizations, and deaths. They also protect those who can't be vaccinated, like young children and the elderly, through herd immunity. Dr. Vanessa Slots highlights the crucial role of vaccines. Immunizations Your Child Needs (and when) Birth to 6 Months Hepatitis B: Shortly after birth, first vaccine dose Diphtheria, Tetanus, and Pertussis (DTaP), Polio, Haemophilus Influenza (HiB), Pneumonia, Hepatitis B and Rotavirus: Ages 2, 4 and 6 months, boosters and vaccines One Year to 18 Months MMR and Varicella (chickenpox) vaccine: Age 1, first vaccine dose Hepatitis A, HiB and Pneumonia: Age 1, booster DTaP: 15 months, fourth vaccine dose Hepatitis, second dose: 18 months Flu Vaccine: 6 months and older, annually* *In the year after receiving their first dose, an infant will need a booster one month later. Four Years Old MMRV, DTaP and Polio, final dose: Four years of age Pre-Teen and Beyond Tdap and Meningitis: Before starting middle school, children receive these vaccines. They are also old enough to start the HPV vaccine, an essential vaccine for all young adults to protect against cancer, genital warts and cervical dysplasia.
Read More About Why Childhood Immunizations Are So Important
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
Departamento destacado: Special Procedures
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
What You Need to Know About RSV
Respiratory syncytial virus, also known as RSV, is a common respiratory virus that impacts the lungs and breathing pathways. The virus can be dangerous for infants and young children and is also concerning for older adults. While most older kids and adults only experience cold-like systems and recover in a week or two, an estimated 58,000-80,000 children younger than 5 years old are hospitalized due to RSV each year, and in 2022 healthcare organizations across the country are experiencing higher infection rates than in years past. "We are experiencing a strong RSV season and do not expect it to go away anytime soon," said Dr. Kris Wilson, Division Chief of Renown Children's Primary Care. "Infants who are infected with RSV almost always show symptoms of runny noses and cough. Call your healthcare provider immediately if your child is having difficulty breathing, is not drinking enough fluids, or is experiencing any worsening of these symptoms.” Symptoms of RSV: Runny nose Decrease in appetite/inability to drink Dry diapers, an indication of dehydration Cough, which may progress to wheezing or difficulty breathing Irritability (most common in very young infants) Decreased activity (most common in very young infants) Decreased appetite (most common in very young infants) Apnea, pauses in breathing for more than 10 seconds (most common in very young infants) What to do if you think your child has RSV: Call your pediatrician! If you suspect your child might have RSV, consulting their healthcare provider is the best first line of defense. From here they will help you build an appropriate treatment plan for child. Keep in mind that many pediatrician offices offer 24/7 call lines. If your child is experiencing retracted breathing (when the area between the ribs and in the neck sinks in when a person attempts to inhale), dehydration (not drinking and decrease in wet diapers) or apnea (pauses in breathing for more than 10 seconds) please call 911 or go to the closest emergency room.
-
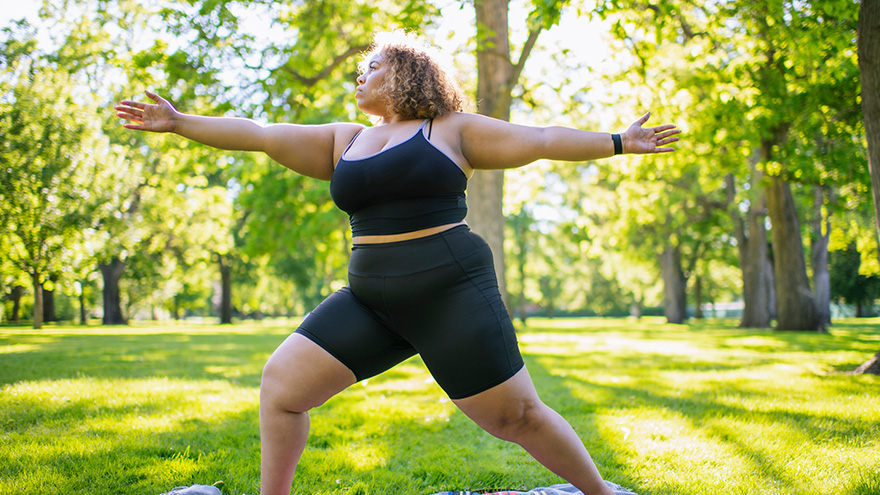
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
6 Healthcare Action Items for the LGBTQIA+ Community
© Niyazz via Canva.com Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
How to Treat a Sprain or Strain
Injuries happen to everyone. They are caused by participating in sports, recreational activities like hiking, and even by accidentally stepping off a curb wrong. If you experience a sprain or strain, the first few days are often the most painful. Renown Sports Medicine physicians Luis Palacio, MD and Brandon Hockenberry, MD walked us through what to do after an injury. Listen to Your Body See a medical professional right away if: You know or suspect that a bone is broken You are having difficulties putting full weight on a joint of the leg Pain or swelling is severe There is a sign of an infection, such as redness and warmth in the joint The First 24-72 Hours Joint sprains tend to swell more than muscle strains. You can use ice as needed for comfort and to relieve any pain, but do not use ice for more than 15-20 minutes at a time. Ice and NSAIDs (such as ibuprofen) can help prevent excessive swelling and mask the pain, but they do not speed recovery. Some research shows that overuse of ice actually delays recovery. During the first 24-72 hours, your injury will go through an inflammation phase. Inflammation is your body’s natural way to dispose of dead tissue cells, build new healthy structures, and hopefully heal even stronger than before.
-
Importance of Safe Sleep
In today's fast-paced society, it is understandable for parents to want to take shortcuts in caring for their little ones. A s a result, It is tempting to leave a sleeping infant in a car seat or swing after a long day of errands or when you need a moment to catch your breath. But, as convenient as these devices may be, they pose a serious risk to your child's safety. Why Car Seats and Swings Pose Risks for Infant Sleep Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The American Academy of Pediatrics (AAP) states that “infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical.” If a parent must use a car seat or other sitting device, they should only do so for a short period of time and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The American Academy of Pediatrics (AAP) warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. This is because infants can easily slump over or become entangled in the straps, blocking their airway, and causing suffocation. Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The AAP states: Infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical. If a parent must use a car seat or other sitting device, they should only do so for a short period and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The AAP warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. In addition, infants can easily slump over or become entangled in the straps, blocking their airways and causing suffocation.
-
What to Expect at a Well Child Checkup
A well-child checkup is a great opportunity to monitor your child’s growth and development, and it's also a chance to establish a trusting relationship with your child’s pediatrician and have your questions answered. What to Expect at Each Checkup At every checkup, a comprehensive physical examination will be conducted to assess your child's growth parameters, including height, weight and head circumference. A developmental assessment will evaluate the progress of your infant or young child in achieving age-appropriate milestones, encompassing language skills, motor development, problem-solving abilities and psycho-social skills. In addition, your pediatrician will address common concerns such as feeding, sleep patterns, oral health and general infant care. Unless there are specific needs or concerns for your baby, routine laboratory tests are typically unnecessary. Your pediatrician will provide guidance on immunization schedules, post-vaccination expectations and when to seek medical attention. Furthermore, during each visit, you will receive age-specific guidance to help you anticipate your child's expected growth and development, along with essential safety precautions and illness prevention measures. Your pediatrician will discuss various topics, such as placing your baby to sleep on their back, utilizing rear-facing infant car seats until around age two, maintaining home water thermostats below 120 degrees Fahrenheit, ensuring dangerous objects and poisonous substances are out of sight and reach, emphasizing dental health and promoting the use of bike helmets, among other things. Preparing for Your Visit It is recommended that, as a parent, you write down any questions beforehand, so you don’t forget them in the moment. Most importantly, feel comfortable asking your pediatrician about anything that might seem unusual, as you are the parent, and you know best! Before leaving the pediatrician’s office, be sure that you fully understand any instructions given to you and ask for clarification if needed. From your child’s birth through young adulthood, you will be visiting your pediatrician regularly. The American Academy of Pediatrics provides what a regular schedule might look like. Well-Child Checkup Schedule Two to three days after birth and at one month Two months Four months Six months Nine months One year 15 months 18 months 24 months 30 months Three years, and yearly after
-
10 Essential Questions to Ask at Your Child's Pediatrician Visit
Taking a few minutes to prepare for your child's pediatrician visit helps ensure that all your child's medical needs are met. Knowing the right questions to ask your provider can help you get the most out of your visit and ensure you and your child feel comfortable and informed. It is essential to base your questions on your child's specific health needs, but the ten options below are a great place to start. How is my child's overall health and development progressing? Is my child meeting their developmental milestones, and are there any areas where they may need extra support? What vaccinations does my child need, and are they up to date on all required immunizations? Are there any nutritional recommendations or concerns for my child's age and stage of development? What are some strategies for promoting healthy habits and physical activity for my child? Are there any warning signs I should look out for regarding my child's health or behavior? What can I do to help prevent common childhood illnesses like colds, flu strains or ear infections? What should I do if my child gets sick, and when should I seek medical attention? Are there any changes to my child's medication or dosage that I should be aware of? Is there anything else I should know or be aware of regarding my child's health or development?
Read More About 10 Essential Questions to Ask at Your Child's Pediatrician Visit
-
Department Spotlight Clinical Research
May 20 is National Clinical Trials Day. Celebrate with us by recognizing the Clinical Research team at Renown Health! The root of every medication, treatment and procedure in healthcare can be traced back to research. From the beginning of the history of medicine, research has always played a crucial role in improving the lives of patients around the world, leaving a permanent mark on how we expand our medical capabilities to this day. Renown Health’s Clinical Research team, in partnership with the University of Nevada, Reno School of Medicine (UNR Med), are leading that effort in our very own community. As our in-house leaders of clinical trials, this team is dedicated to advancing the science of medicine to help further our bottom line of making a genuine difference in the health and well-being of the patients they serve. Trial by (Medical) Jury Every day looks different for the Clinical Research team, especially when it comes to interacting with patients, providers and “sponsors,” which are the organizations providing the treatment for the study. One fact always remains true: communication and collaboration are key, especially among the team who act as the face of this process. Meet Lisa English (pictured above on the far right in a blue shirt), a Lead Clinical Research Coordinator at Renown who serves as the study "project manager." One aspect of Lisa’s day-to-day is seeing patients through their clinical trials from start to finish. It all begins with the setup. “Before we can launch a study, there is a lot of back-and-forth dialogue between everyone involved to ensure the best fit,” said Lisa. “Sponsors will come to us with novel treatments, such as medications or devices, and the inclusion criteria that patients need to meet in order to qualify for the study. We then immediately jump into working with the providers, looking closely at the science and comparing the treatments to what is on the market already.” From there, Lisa coordinates conversations between the providers, sponsors and study teams to gauge everyone’s capacity based on the length of the study, ensuring everyone involved has the time to dedicate to the process. Next, the providers identify patients that meet the criteria for the study, and together, the team decides where the patient visits will happen and discusses any potential barriers that may affect patient retention. The budget is clearly defined at this stage, set up to make sure no patient is ever billed for medical costs incurred as a result of the study. Often, research participants are seen within the specialty clinics throughout the health system, while other times the Clinical Research Coordinators see patients at the recently centralized Clinical Research Office at Renown Regional Medical Center. This location provides an essential public-facing space for the community to learn more about clinical trials and demonstrates the breadth of resources available at Renown to sponsors to strengthen external partnerships and research funding opportunities. Once the study officially begins, team members like Lisa will set patients up for a “screening/qualifying visit.” During this appointment, she makes sure patients get scheduled for their lab work, imaging scans and anything else the provider may need to make an executive decision on whether or not the patient is a good candidate for the study. “I build it all in Epic,” said Lisa. “The study information, directions, requirements and next steps are all loaded in Epic for easy tracking. We are also required to input any notes in the sponsor’s electronic data capture website. All the information I track is inputted without protected health information (PHI), so every patient is completely anonymous.” After the patient officially qualifies, the study goes full steam ahead. Team members like Lisa and the providers receive continual updates from sponsors on the status of the study. “Throughout the entire process, I make sure patients get scheduled for everything that meets the requirements for the study,” said Lisa. “I meet with patients one-on-one to discuss their needs and concerns and ask questions about the study, organize their appointments and charts and deal with any issues or pivots that may arise. It’s very important that every patient fully understands what is going to happen with their care.” The Clinical Research department strives to serve as a care partner to patients, providers and clinics they work with. The majority of our Clinical Research Coordinators are trained phlebotomists and medical assistants, performing their own assessments such as lab draws and electrocardiograms (ECGs) to streamline the research visit process and reduce resource constraints on the clinics and health system. Lisa typically sees a couple of patients per week, depending on the study and where patients are in the cycle. Depending on the complexity of the trial, patients may see the research team only one time or several times over many years. Typically, clinical trial patients are seen in clinic every 2-4 weeks. There are many tasks required before, during and after a research visit to ensure everything runs smoothly, so Clinical Research Coordinators dedicate an average of 5-11 hours of work per patient, per visit. Regardless of patient load, each employee in the Clinical Research department – as well as participating teams across Renown and UNR Med – always step in to help each other out. According to Lisa, the environment is immensely supportive. “We have a program here at Renown to train employees who have never done clinical trials,” said Lisa. “We love seeing people get more engaged with the important work we do, and every department has been great at collaborating with us. Everyone brings a different perspective.” At the end of the study, Lisa gathers all the information and collects notes into a zip drive or paper binder for archiving. The sponsor lets the Clinical Research team, providers and patients know whether they are on the trial drug or on the placebo. The teams use the data gathered during the study to publish a report or present at conferences, promoting the critical research done to better the lives of patients in our community, and potentially, the world. “I appreciate the time everyone gives us to make sure our research is successful,” said Lisa. “It feels great to work together to make a difference, improve healthcare quality and save lives.” Behind-the-Scenes, Yet on the Frontlines The impact of research studies transcends hospital walls, and this can all be attributed to the dedication of our Clinical Research department. The constant collaboration between this team, lab science, medical assistants and providers, cardiology technologists, sonographers, finance teams and our partners at UNR Med is crucial to safeguarding the success of the studies. Devoted to keeping research close to home, Renown and UNR Med teamed up to form the Clinical Research Office (CRO) in 2021. With the strength of northern Nevada's largest not-for-profit health system and Nevada’s first medical school, this team is dedicated to giving our community access to the latest care innovations. “At UNR Med, we are working with students, residents and academic faculty; on the Renown side, we are working with clinicians and community participants,” said Amber Emerson, Manager for Community Outreach and Research Engagement for UNR Med. “Everything we do is data-driven,” added Kristen Gurnea, Manager of Clinical Research for Renown. “Our main goal is to optimize our impact and provide a community benefit for our patients. The scope of our roles in the Clinical Research office is very diverse.” To help meet the growing need locally for healthcare and cutting-edge treatment solutions, the CRO has continued to grow, expanding its research capabilities and helping bring new medications, medical devices and more to patients across northern Nevada and northeastern California. “Once upon a time, our team had only six members; today we have grown to a team of 25,” added Diana Torres, Research Resource Analyst for Renown. “We used to be considered one department, including Medical Education, and we have since branched off into our own cost center. We branched off even further and created a separate Genetics department that runs the Healthy Nevada Project. Throughout this process, the Clinical Research department was always the main point of the umbrella.” “We participate in hospital-wide outreach and marketing, and we feel this has really helped us get the word out about our department,” added Raul Arellano, Research Resource Analyst for Renown. “In fact, we doubled our clinical trial portfolio from last year.” The CRO currently operates over 100 clinical trials locally in cardiology, endocrinology, infectious disease, neurology, pediatric and adult oncology, pediatric sub-specialties and pulmonology. Behind the curtains of in-person research, the CRO is home to several experts who help turn our research studies into a reality, from budgeting and billing to barrier-breaking and building relationships. “I help with barriers patients and Clinical Research Coordinators are facing, building connections and relationships inside and outside of our health system,” said Kristen Gurnea. “I enjoy handling all the supporting pieces that are required for studies to happen.” “My role changes every day,” added Jenna Berger, Administrative Assistant for the CRO at Renown. “Some days, I’ll be helping coordinate patient stipends and going through document management to ensure we have all necessary signatures. Other days, I will be planning events – like Clinical Trials Week – for our department and creating marketing materials and fliers.” “Our day-to-day involves going over anything related to research financials,” added Diana Torres. “We handle sponsor billings, process efficiency and collecting revenue for research contracts, and we collaborate closely with our Finance department and Revenue Integrity in order to accomplish this. It’s important for us to make sure all billing on both the sponsor and patient side is taken care of, especially because patients should never receive a bill for medical services they receive for the trial. A year and a half ago, we started doing budget negotiations for research contracts,” said Diana Torres. “We are proud to help clinical teams with any training they may need on these negotiations as well as billing reviews and allocations.” Seeing patients progress during a study and transform before their eyes inspires the CRO team to continue doing what they do every day. “I’ve been here for many years, first working on the floor as an oncology nurse and transitioning to oncology research in 2005,” said Anna Winchell, Cancer Protocol Nurse for Renown. “I love getting to know the patients and seeing them progress into a healthy lifestyle.” Medical students and residents at UNR Med also play a significant role in the research process, advancing medicine by exploring causes and novel treatments for a wide range of conditions, including HIV, muscular dystrophy, gastrointestinal disorders, infectious diseases and more. Medical research at UNR Med is headed by committed research coordinators, community outreach managers, grants managers, pharmacists and physicians. “I oversee scientific review and help the physicians that come to us for those resources,” said Amil Trujillo-King, Medical Research Coordinator at UNR Med. “I guide medical students in their research protocols and help with different projects to improve research activities for both students and medical residents.” It takes a village to make clinical research happen. Because of that, the ACRO cannot thank the following teams enough for moving mountains for the future of medicine: Renown Health and UNR Med leadership for demonstrating the integrated health system’s commitment to expanding access to clinical research in our community within both the Renown / UNR Med affiliation and Renown active strategic plans. Renown Pharmacy especially Research Clinical Pharmacist Tim Morton, who supports all clinical trial medication dispensing and patient education across all clinical trials at Renown. Accounts Payable for having a huge impact on patient and employee reimbursement. Renown Medical Group for their participating providers, especially in oncology, cardiology, pulmonology, pediatrics, endocrinology and neurology, who are involved in research year after year. Marketing and Communications for helping with printed materials and raising awareness for clinical research at Renown and UNR Med. An Affiliation to Last Through the Ages A collective, shared vision of exploring community health – that is the impetus behind the affiliation between Renown and UNR Med. By leveraging resources across both institutions, the CRO has maximized their impact, giving the people of northern Nevada greater access to new interventions and treatments and promoting an impassioned culture with patients, providers, residents and medical students. “Community-based research always sat well with me,” said Amber Emerson. “As Renown and UNR Med, we have this unique opportunity to shape clinical research here in northern Nevada. We always make sure we present research in a meaningful way that speaks to the work we produce and demonstrates the opportunities we offer. After all, participating in clinical research doesn’t mean our patients are ‘guinea pigs’ – quite the opposite! They are partners in their health care, and we support them through providing access to novel treatments.” “Research is my passion, and my career has spanned broadly from grants administration to study coordination,” added Valerie Smith, Clinical Research Center Administrative Manager at UNR Med. “I am excited to be at the forefront of research frontiers in northern Nevada.” Through robust engagement and collaboration with healthcare providers, department administrators, internal research team members and leadership, the strength of this affiliation is unmeasurable. The CRO’s ultimate goal is to have clinical trials be the standard of care for every condition that Renown and UNR Med treats. Clinical research participation is all about patient autonomy, shared decision-making between patients and their providers and advancing medicine to save lives. From their beginnings as a small group of passionate researchers to their present reality as a leader in the research space in northern Nevada, their efforts do not go unnoticed. “The success of our department is inspiring,” said Amil Trujillo-King. “Renown and UNR Med supports the wellbeing of all employees and contributes directly to the growth of the department.” “When I first joined Renown in Patient Access, I didn’t realize that we had a research department; with a strong healthcare background in my family, I knew I wanted to grow in my career, and our expanding Clinical Research office was that next step,” said Raul Arellano. “With our affiliation with UNR Med, it’s especially inspiring to be able to apply what I learned as a Patient Access Representative to help further outcomes for our patients through managing our finances.” Through their unwavering commitment to research excellence and patient-centered care, the CRO will continue to pave the way for groundbreaking medical discoveries and improved outcomes for patients for years to come. “Fundamentally, we’re working to build a culture of research in our community because we believe it is the right thing to do. Our community deserves to have access to clinical trials and novel care close to home with a dedicated team to support them every step of the way,” closes Kristen Gurnea.