Buscar
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
Departamento destacado: Special Procedures
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
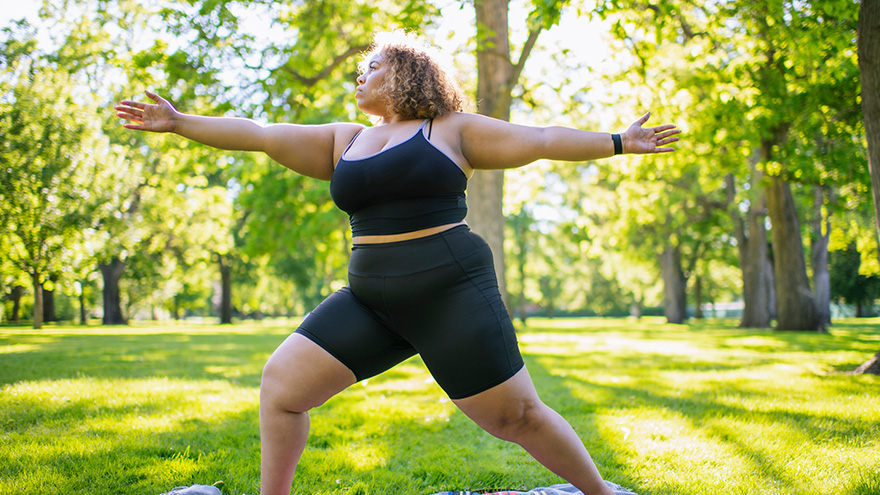
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
How to Treat a Sprain or Strain
Injuries happen to everyone. They are caused by participating in sports, recreational activities like hiking, and even by accidentally stepping off a curb wrong. If you experience a sprain or strain, the first few days are often the most painful. Renown Sports Medicine physicians Luis Palacio, MD and Brandon Hockenberry, MD walked us through what to do after an injury. Listen to Your Body See a medical professional right away if: You know or suspect that a bone is broken You are having difficulties putting full weight on a joint of the leg Pain or swelling is severe There is a sign of an infection, such as redness and warmth in the joint The First 24-72 Hours Joint sprains tend to swell more than muscle strains. You can use ice as needed for comfort and to relieve any pain, but do not use ice for more than 15-20 minutes at a time. Ice and NSAIDs (such as ibuprofen) can help prevent excessive swelling and mask the pain, but they do not speed recovery. Some research shows that overuse of ice actually delays recovery. During the first 24-72 hours, your injury will go through an inflammation phase. Inflammation is your body’s natural way to dispose of dead tissue cells, build new healthy structures, and hopefully heal even stronger than before.
-
How to Manage and Prevent Tendonitis
Tendonitis occurs when a tendon in your body is inflamed or irritated. This painful condition can impact your day-to-day activities, but can be managed and prevented. Luis Palacio, MD, shared some insights into how to manage tendonitis. Overuse and Repetitive Motion Tendons are complex tissues in our body that connect muscles to bones, allowing us to move. Unfortunately, sometimes these tendons become inflamed, worn down or injured, a condition called tendonitis. Symptoms of tendonitis include pain or dull ache, tenderness and mild swelling at the site. While tendonitis can be caused by a sudden injury, it is more commonly seen in frequent motions, including: Repetitive motions in exercise, work or other physical activities. Awkward positions in a movement, including poor posture. Forced movements that strain your body. Sudden increase in frequency of movement or level of difficulty, including little to no recover time between new activity. Shoes without proper support or hard surfaces, such as concrete floors. Evaluation is Key If you suspect that you have tendonitis and it does not resolve on its own after a few days, you should get it evaluated by a primary care or sports medicine doctor. They can make recommendations to aid your recovery and refer you to the right sub-specialist if needed. With some intentional actions, you can help reduce the risk of tendonitis with the following suggestions: Add variety: Mixing up the type of exercise you do will help prevent repetitive motions that can result in overuse. Stretch and condition: Make sure the keep up with proper stretching and muscle strengthening to support your physical activities. Do it right: Make sure that the way you are completing exercise or work-related physical activities is correct. Seek out a professional for lessons or guidance if you are unsure.
-
Departamento destacado: Infection Prevention
Hygiene in healthcare is an essential backbone to providing the safest, most optimal care to every patient. From everyday handwashing techniques and getting all necessary vaccinations to surveilling our health system before the onset of outbreaks, at Renown Health, creating and maintaining a low-infection environment is a group effort. From ensuring fundamental infection prevention practices are carried out to identifying process improvement opportunities, Renown’s Infection Prevention (IP) department is here to help care teams be successful in their role. This effort is led by members who are devoted in sharing evidence-based best practices to our patients, employees, healthcare organization partners and community. Making “Zero” A Reality Reducing healthcare-associated infections is possible when core infection prevention practices are incorporated into the daily care of our patients. These team members are dedicated to Renown’s commitment to creating a culture of Excellence, caring for our healthcare environment, and our care teams. “Often times, when asked what we do in our work it can be a challenge to answer because unpredictability is built into almost every day; and in that, we as a team must divide and conquer,” said Susanne James, Manager of Infection Prevention. Every day, each team member is assigned a day to perform required surveillance activities. Whether they are reviewing patients’ infections and isolation and evaluating lab orders for possible infectious processes or reporting communicable diseases to the local health authorities and the CDC, every Infection Preventionist participates in improvement projects and address issues as they arise. The Infection Prevention team plans, organizes, manages and evaluates the Infection Prevention Program and ensures IP policies reflect current best practice. They work closely with all departments at Renown in order to achieve high levels of standards that are implemented to reduce transmission of infection. “As a team, we perform ‘Infection Prevention Environment of Care Rounding’ on all units and departments to ensure our environment complies with regulatory requirements,” said Erika Clark, Operations Analyst at Renown Health. "We work together with Facilities and Site Practice Leaders to ensure a safe environment.” The pandemic challenged all Renown teams to find creative solutions for issues no one ever imagined. Our Infection Prevention department worked tirelessly alongside Renown's Hospital Incident Command Structure (HICS) and care teams in creating several lines of defense against COVID-19, including: Launching Renown's Alternate Care Site to meet the need for critical patients. Bringing on the new lab tests and specimen collection criteria. Managing demand for personal protective equipment (PPE). Bringing vaccines to staff and then to the community. Managing ill employees and our visitors. Keeping all locations informed on pandemic status and changes (which were occurring at breakneck speed). These initiatives enabled Renown's care teams to focus on providing the safest care possible to patients saving countless lives. This solidified the fact that together, the team can accomplish anything. “Infection Prevention is proud to be a valued and respected member of the care team,” said Susanne James. “We appreciate being a trusted resource and take this responsibility seriously as this enables us to provide staff the best possible tools to be successful.” Fight the Good Fight Against the Spread of Disease Educating patients and providers plays a huge part on the Infection Prevention stage. This team provides educational materials on a range of topics, some of the most important are, proper hand hygiene and the use of PPE. All these materials can be found throughout our health system and serve as an important reminder – infection prevention starts with all of us. “We partner with every aspect of the health system – environmental services, nutrition services, lab services, facilities, pharmacy, physical therapy and occupational therapy, respiratory care, patient access, security, nurses, providers and quality...just to name a few!” said Susanne James. Our Infection Prevention team also partners with Washoe County Health District and other public health agencies to report – and in turn, stop the spread of – diseases and exposures. These close partnerships poise our team to do what we do best: Fight the Good Fight. “I greatly appreciate everyone in the IP department for sharing their expertise as I learned a new position,” said Erika Clark. “I love working with my team and how closely we work with other departments to ensure excellence in all we do.” Our health system is ever-changing. But according to the experts in our Infection Prevention department, the three main ways to prevent illness and disease that remain the same time and time again are to: Clean your hands. Hand hygiene is the most effective way of preventing the spread of infections. The CDC recommends washing your hands with warm soap and water for 15-20 seconds or using an alcohol-based hand sanitizer. Clean your hands often and assist our patients to do the same. Learn expert hand-washing advice here. Get vaccinated. Immunizations are one of the top methods you can embrace the fight against preventable diseases, such as COVID-19, flu, measles, tetanus and more. Discover how you can get vaccinated with Renown. Keep germs from spreading. Practice good hygiene by covering your cough or sneeze or wearing a mask and sanitizing frequently touched spaces. Stay home if you feel ill to prevent the spread of illness and infection. Be sure to bring up any illness concerns with your primary care provider. “Every aspect of our health system has an infection prevention component, and we work daily to ensure our staff, patients and visitors are providing and receiving care free from potential harm or infections,” said Susanne James. “We are often the first call staff make when they have questions, concerns or just need someone to help improve process or outcomes.” Reveling with Renown Proudly defining themselves as a “small but mighty” team, the six-person Infection Prevention department moves mountains to ensure the safety of anyone who walks through Renown’s doors. The tight-knit nature of this team can be felt from miles away, and to them, being “small but mighty” is not a hindrance, as they have the support of the IP Champions and the entire health system. “I originally came to Renown in 2018 as a nurse traveler, the facility and people I worked with immediately made an impact on me,” said Brian Stroud, Infection Preventionist at Renown Health. “My wife and I chose Renown and Reno due to the positive impact the people had on us. Everyone is welcoming, helpful and caring. Now, I am a full-time employee, and the team has made my transition into infection prevention trouble-free." Renown’s mission of providing a genuine difference for the health and wellbeing of the community is heightened and echoed by the Infection Prevention team. “I chose Renown because of the reputation Renown has earned in the community because of the excellent care and level of services provided,” said Shannon Oriola, Infection Preventionist at Renown Health. “I absolutely love this team and my Renown family!” “What brought me to Renown was the opportunity to acquire diverse skills which then motivated me to pursue my master’s degree,” added Paul DeLeon, Infection Preventionist at Renown Health. “What keeps me here is the people – Renown attracts hard working, ethical and caring people.” "My wife and I loved coming out to the Nevada mountains on vacations," added Russ Laarman, Infection Preventionist at Renown Health. "After being in Michigan for 47 years, we took the plunge and made NV our home. The experience has been great! I work with a great team that is very knowledgeable and works hard to ensure positive outcomes for our patients and colleagues at Renown.” Their pride shines through with their own individual accolades, both inside and outside of work. This past year: Shannon Oriola received a scholarship from the Association for Professionals in Infection Control and Epidemiology (APIC) for “improving outcomes through knowledge and practice,” which provided her with a $1,000 scholarship to attend the annual APIC conference in Indianapolis. Paul DeLeon earned his Certification in Infection Control and Prevention from APIC. Erika Clark completed Renown’s High Potential program, a six-month program that gives employees hands-on learning experience with several competencies, including emotional intelligence, effective communication, building successful relationships and organizational knowledge. Brian Stroud and his wife Charla became official Nevada residents. Russ Laarman scaled Mount Whitney. ...And the list keeps growing! Charged with the goal of keeping disease spread at bay, our Infection Prevention team remains vigilant and dedicated to their mission. Their commitment to Renown and to keeping our health system clean and healthy proves the age-old saying true: not all heroes wear capes. “I’m so very proud of the work Infection Prevention does every day, working with the vast teams throughout the health system to improve lives,” said Susanne James. “We would like to thank all of you for protecting the health and safety of your colleagues, our patients and the community.”
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
Generic Drugs – What You Need to Know About Them
Without a doubt, taking medications can not only be expensive, but also confusing. In the United States, generic prescriptions are widely used, with 9 out of 10 people choosing them over a name brand. Pharmacists are a great resource to help us understand the benefits and side effects of any medication. We asked Adam Porath, PharmD, Vice President of Pharmacy at Renown Health, to answer some common questions about generic drugs. What is a generic drug? A generic drug has the same active ingredients of brand-name drugs. Brand-name drugs have a patent (special license) protecting them from competition to help the drug company recover research and development costs. When the patent expires other manufacturers are able to seek approval for a generic drug. However, the color, shape and inactive elements may be different. Per the U.S. Food & Drug Administration (FDA), a generic medicine works in the same way and provides the same clinical benefit as its brand-name version. Why do they cost less? Generic drug makers do not have the expense of costly development, research, animal and human clinical trials, marketing and advertising. This savings is passed on to the public. Also after a patent expires, several companies will compete on a generic version of a drug, further driving down prices.
Read More About Generic Drugs – What You Need to Know About Them
-
Alzheimer’s Disease – How to Spot the Signs
Alzheimer’s disease is not normal forgetfulness as we age. Instead, it is a specific form of mental decline. And according to the Alzheimer’s Association it accounts for nearly 80 percent all dementia cases. Natasa Dragicevic, MD, PhD., behavioral neurologist and Alzheimer’s disease specialist with Renown Institute for Neurosciences, weighs in on diagnosing it and the importance of early medical action. How to Diagnose Alzheimer’s Disease In general, the signs of Alzheimer’s disease occur slowly, getting worse over time. For example, forgetfulness is a daily search – for shoes, keys and other misplaced items. Not only is memory affected, but also speech patterns and behavior. There is no single test for Alzheimer’s disease. “Specifically, a neurologist should be the one to diagnose Alzheimer’s disease given differences in presentation,” clarifies Dr. Dragicevic. “And ideally a behavioral neurologist (Alzheimer’s sub-specialist) will be managing the treatment,” she adds. Brain Imaging Diagnosing Alzheimer’s disease involves multiple approaches and medical providers. In short, medical history is reviewed along with a physical exam, lab tests and other diagnostic testing. “A medical workup includes a variety of tests. These include MRI and other brain imaging, as well as neurological and psychological testing. Furthermore, a lumbar puncture is performed to look for markers of the disease,” she states. What Causes Alzheimer’s disease? Although no one knows the cause, researchers think many factors play a role. Uncontrollable risk factors include your genetics and having a family member with the disease. However, the controllable risk factors include: reducing the risk of head injury and keeping your heart healthy. It’s important to realize that high blood pressure, high cholesterol, stroke and diabetes play a role in brain health. Blood loss to the brain causes vascular dementia, leading to long-term blood vessel damage. Symptoms of Alzheimer’s disease Generally speaking, the signs of this disease differ in each person. Yet noticeable behaviors include: • Losing the way to familiar places • Forgetting to pay bills • Trouble finding the right words when talking • Repeating questions • General confusion • Social withdrawal Alzheimer’s Disease – Benefits of Early Diagnosis Equally important, spotting Alzheimer’s disease early allows more time to benefit from medications and possible clinical trials. Likewise, nutrition and exercise changes can be made, increasing blood flow to the body, and perhaps delaying symptoms. Early diagnosis also allows for personal health decisions and quality-of-life conversations to take place. According to the Alzheimer’s Association, these benefits include: 1. Medical advantage 2. Emotional and social comfort 3. Time to plan ahead 4. Cost savings A Brain Supporting Lifestyle “At the present time, treatment is limited,” explains Dr. Dragicevic. “Usually Alzheimer’s is a progressive ongoing disease – any management at this time is purely symptomatic.” However, she states the following lifestyle changes can help support brain health: • New hobbies such as painting, pottery, music classes or learning a new language • Crosswords, puzzles and playing games, such as Scrabble • Brain challenging mobile apps, such as Luminosity • 30-45 minutes of mild to moderate physical activity per day, such as walking • Eating a Mediterranean diet (primarily plant based foods)
-
¿Es la cirugía bariátrica adecuada para usted?
You’ve likely heard about bariatric surgery — and perhaps even have friends who’ve done it. But is it a potential solution for you? Here, Dawn Remme, RN, Metabolic Bariatric Surgery Program Manager, provides insight. You may have been struggling with excess weight for years. You’ve tried high-protein diets, low-carb diets and more. Most patients considering weight loss surgery have tried numerous dieting methods. The truth is, some patients who suffer with obesity are successful dieters. Unfortunately though, excess weigh often returns. This impacts their health and the quality of their life. It can be a disheartening battle. Weight loss surgery is a big decision. In making this decision, keep in mind that surgery is only one step toward your goal of achieving better health. It is neither magic, nor is it the “easy way out.” Weight loss surgery can offer you a TOOL to help you become more successful in controlling the disease of morbid obesity. By combining this tool with a lifelong commitment to important lifestyle changes, medical follow-up and nutritional modifications, you have the potential to become a healthier you. Bariatric Surgery By the Numbers Exploring the facts about obesity, how it impacts your health, and how surgery can resolve or significantly improve your chronic medical conditions is the first step to making a decision. Obesity is medically defined as “excess body fat” and is measured by a mathematical ratio known as the Body Mass Index (BMI). To calculate your BMI, we consider your height, weight, age, gender and body build. Here are the standards: “Normal” BMI: less than 25 Overweight: 25 – 29.9 Obese: BMI of 30 – 39.9 Morbid obesity: BMI of 40 or more Morbid obesity (BMI over 40) is a lifelong, progressive disease, and the prevalence of morbidly obese Americans (100 or more pounds over a healthy weight) is increasing rapidly. According to the CDC, the disease of obesity affects 78 million Americans. Further estimates indicate about 24 million have morbid obesity. Serious medical problems known as co-morbidities often occur when someone is morbidly obese. Studies tell us conditions such as type 2 diabetes, high cholesterol, sleep apnea, high blood pressure and degenerative arthritis increase in severity as the BMI is increasing in patients. When may weight loss surgery be an option? When someone has a BMI greater then 40. If a person’s BMI is 35 – 39.9 and they have significant health problems such as type 2 diabetes, high blood pressure, high cholesterol, sleep apnea, or other diagnosed health conditions related to obesity. Gastric Sleeve, Gastric Bypass Explained To resolve or significantly reduce these health conditions, bariatric surgery can be done when diet and exercise haven’t worked. Weight loss surgery makes changes to your digestive system to help you lose weight. The gastric sleeve limits how much you can eat, whereas gastric bypass limits how much you can eat and reduces the absorption of certain nutrients. Other Benefits of Surgery You can greatly increase life expectancy by resolving or significantly improving conditions like diabetes, high cholesterol, high blood pressure, sleep apnea, and obesity itself. Infertility can also be positively affected. A significant weight loss and relief from serious health conditions and diseases will greatly improve your quality of life. Studies tell us that type 2 diabetes is resolved or significantly improved in 84 percent of patients following bariatric surgery. Cholesterol levels dropped in 95 percent of patients. And hypertension and sleep apnea showed improvement in 68 and 80 percent of patients, respectively, following bariatric surgery. Bariatric Surgery at Renown In making the decision to move forward to better health, it is important to remember: Obesity is a disease, and the desire to have a healthier, longer, more fulfilling life is possible. If you are interested in learning more, please visit the Bariatric Surgery Program page to view more information about Renown Regional Medical Center’s MBSAQIP accredited bariatric program, as well as information about upcoming educational seminars. Or call 775-982-RSVP (7787) to reserve your seat. Learn More
-
Use Caution: Mixing Over-the-Counter Medications Can Be Harmful
When you’re too sick to go to work but not sick enough for a doctor’s visit, over-the-counter medicines are a welcome relief to help alleviate that fever, runny nose or allergies. But because those medicines aren’t signed off on or managed by your doctor and pharmacist, you must be especially mindful of what you put into your body. Whenever you pop a pill, you want to ensure you’re taking the correct dosage, waiting the right amount of time before taking another dose and not mixing certain medicines. Too Much Tylenol/Acetaminophen Tylenol — or acetaminophen — is a popular pain reliever for many, but too much can be bad for your liver. “Our bodies have a finite ability to metabolize Tylenol,” says Andy Wright, clinical pharmacist at Renown Rehabilitation Hospital. “When too much builds up in the liver, it becomes toxic. In patients with medical conditions like cirrhosis of the liver or hepatitis, this could be disastrous.” Remember, acetaminophen is in more than just Tylenol and generic pain relievers. You may also see acetaminophen in flu, cold and cough medicines, like Nyquil, and some prescription medications including Norco and Percocet. Keep a list of the medications you take, and limit daily acetaminophen use to 3,000 mg per day. When you’re scanning medicine bottle contents, remember acetaminophen is also referred to as APAP, AC, acetam or paracetamol. Mixing Painkillers When you’re dealing with pain and not getting any relief, taking a different medication may seem like the easy solution. Maybe you take some Aleve — a form of naproxen — for a headache, but it isn’t working, so you switch to Motrin, an over-the-counter form of ibuprofen. Not a smart idea. Ibuprofen and naproxen along with aspirin are known as nonsteroidal anti-inflammatory drugs (NSAIDS). Because these medicines work in similar ways, they should never be combined or used in larger doses or more frequently than directed. Otherwise your risk of side effects can increase, which range from mild nausea to severe gastrointestinal bleeding. It’s also important to consider your family history when taking NSAIDs because, “recent studies have shown NSAIDs may have greater cardiovascular risks for people taking blood thinners or those with hypertension,” explains Andy. “A good example is ibuprofen: It has a relatively low gastrointestinal bleed risk while it has a moderate to high cardiovascular risk. The opposite is true for naproxen.” Rather than experimenting with multiple medicines, figure out which drug works best for you. You may find muscle soreness improves with aspirin, whereas when a headache hits, naproxen is best. Keep in mind that these medications aren’t always best for everyone in the family. “Aspirin in children and teens is not recommended unless under the supervision of a doctor,” Andy says. And pregnant and lactating women should generally avoid NSAIDS due to risk of birth defects and bleeding. “In both of these cases, acetaminophen or Tylenol are preferred but only if approved by an OB/GYN.” Fighting Allergies Over-the-counter antihistamines like Claritin, Zyrtec and Allegra have made fighting itchy eyes and runny noses a little easier. But these daily medicines — when taken inappropriately or in the wrong combinations — can also have an adverse effect. Similar to acetaminophen, you need to watch for antihistamines in other products. Sleep aids — like Tylenol PM and Unisom — commonly use an antihistamine known as diphenhydramine, which may increase your risk of overdose. “Combining antihistamines, or overdosing, can cause many adverse effects including dry mouth, blurred vision — even arrhythmias,” Andy says. “Only take these medications on their own.” If you’re still struggling with symptoms, you can talk to your doctor about adding an over-the-counter nasal steroid. Andy confirms the importance of closely following the directions listed on antihistamine (and all medicine) bottles. He has seen extended release nasal decongestants cause significant arrhythmias requiring medical care after a patient took the medicine with warm fluids. “The decongestant in question is designed to slowly release, but it can dissolve suddenly in the presence of warm liquids like coffee,” Andy explains. “This can cause the pill to deliver 12 to 24 hours of medication all at once.” Taking an Antidiarrheal with Calcium Calcium supplements and antidiarrheal medicines are another harmful combination. Calcium firms up your stool, but if taken with an antidiarrheal, can cause severe constipation. If you need to take an antidiarrheal, take a break from your calcium for a few days until you’re back to normal. Another consideration when taking calcium supplements or calcium-based antacids is gas. “I’ve had several patients report cases of excessive gas using Tums or calcium carbonate-based supplements.” Andy suggests instead “trying Maalox or Mylanta for indigestion and Citracal as a supplement.” Talk with Your Doctor or Pharmacist About Your Medications If over-the-counter drugs aren’t providing the relief you need, it’s time to see your doctor. And remember, for your safety it is important to keep your doctor and pharmacist up-to-date with any medications — prescribed or over-the-counter — that you are taking.
Read More About Use Caution: Mixing Over-the-Counter Medications Can Be Harmful