Buscar
-
Departamento destacado: Surgery & Procedure Scheduling
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
A Therapist's Tips to Prevent and Manage Osteoporosis
Want to know more about osteoporosis and osteopenia? We'll dive into these conditions and give you some handy tips on preventing future problems and taking care of your bones. What is Osteopenia? Osteopenia (low bone density) is the initial stage of bone mineral density loss, which can eventually progress to osteoporosis if steps are not taken to prevent it. What is Osteoporosis? Osteoporosis is a condition that weakens our bones. While it literally means “porous bone," it doesn’t mean that our bones are doomed to succumb to the changes that can happen to us silently over time. Our bones are living tissues that are constantly breaking down and remodeling themselves. Osteoporosis and osteopenia are typically diagnosed by testing bone mineral density using scans that your primary care provider can easily order. This is important testing because it dictates your risk of breaking a bone in common areas like your hip, wrist or spine. It also helps set the stage for talking with your healthcare team to develop a treatment plan. Most people will reach their peak bone mass in their mid to late twenties. There are several factors that increase our risk of osteoporosis or osteopenia as we age, such as menopause, genetics and other lifestyle factors. However, there are several things you can do to mitigate this breakdown and assist your body in the constant remodeling it does to our bones. 3 Controllable Factors to Build Strong Bones 1. Talk to your primary care provider They can go over a plan and prescribe things such as vitamin D, calcium and medications that can help if you are at risk or have osteoporosis or osteopenia. 2. Maintain a healthy diet Talk to a dietician if you need further help as they can be an invaluable resource to develop a plan. Eat foods rich in calcium, vitamin D and vitamin C. These assist with the rebuilding of bone. Examples include but aren’t limited to leafy greens, legumes, salmon and healthy dairy products. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per week. Alcohol interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. 3. Exercise Talk to your primary care provider to get a referral to physical therapy if you need help with exercise. Our bones adapt to the stresses we put them through. Therefore, exercise should be tailored to putting the right stress on our bones. There is good quality research that most exercise is safe when dealing with less bone mineral density. The exercises should be progressively challenging and increase the load for resistance and weight training at least two to three days a week. Examples include squats, step-ups, chest presses and rows. Exercises higher in velocity will lead to more power and bone adaptation. Examples include quicker push-ups, marching and quicker walks. Exercises that are weight-bearing will lead bones to adapt to the stress placed on them. Movements such as mini stomps, step-ups, jumping, jogging and so forth may be used depending on how your body tolerates these things to really stimulate bone adaptation. There are aspects of aging and bone health we can’t control, but we can take steps to minimize the chances of bone loss and osteoporosis. Talk to your healthcare team to determine your risk and don’t forget to show your bones a little TLC – you’re going to need them.
Read More About A Therapist's Tips to Prevent and Manage Osteoporosis
-
How to Protect Your Kids from Heatstroke
Summer is around the corner, bringing heightened risks of heatstroke, especially for children who cannot regulate their body temperature as efficiently as adults. Infants are particularly vulnerable and may not express discomfort, so never leave a child unattended in a vehicle. Top Tips for Preventing Heatstroke Reduce the number of deaths from heatstroke by remembering to ACT. Avoid heatstroke-related injury and death by never leaving a child alone in a car, not even for a minute. And make sure to keep your car locked when you’re not inside so kids don’t get in on their own. Create reminders. Keep a stuffed animal or other memento in your child’s car seat when it’s empty, and move it to the front seat as a visual reminder when your child is in the back seat. Or place and secure your phone, briefcase or purse in the backseat when traveling with your child. Take action. If you see a child alone in a car, call 911. Emergency personnel want you to call. They are trained to respond to these situations Keeping Your Baby Cool in the Back Seat In hot weather, it is crucial to keep your baby cool and hydrated by using a car seat cover or towel over them to reflect the sun's rays. Dress your baby in lightweight clothing that covers their arms and legs. Keep an eye on your baby's skin color. Move them to a cooler place if they look too red or flushed. Keep the temperature at a comfortable temperature for you, not for your child. Keep the windows cracked open for ventilation and ensure nothing is blocking the airflow from entering or exiting the vehicle. Dress your infant appropriately for their environment, including appropriate head and neck coverings, to keep them cool and protected from sunburns. Ensure you have enough fluids to last an hour before getting out of the car or use bottled water if possible. Never leave your child unattended in a car. Steps to Follow if You Suspect Heatstroke Call 911 immediately. Cool the victim – Get the person to a shady area, remove restrictive clothing and cover skin with sheets soaked in ice-water, and place ice packs in the arm pits and groin. Have the victim drink cool fluids, preferably an electrolyte-containing sports drink. Monitor body temperature with a thermometer but stop cooling efforts after temperature has dropped to 102 Fahrenheit. Baby Safe Classes These classes help prepare parents for emergencies that may occur in baby’s first year. Safe Kids Worldwide Did you know heatstroke is the leading cause of non-crash related fatalities in children? “On average, every 10 days a child dies from heatstroke in a vehicle. In more than half of these deaths, the caregiver forgot the child was in the car.”
-
Why Childhood Immunizations Are So Important
Immunizations save thousands of lives each year by preventing serious illnesses, hospitalizations, and deaths. They also protect those who can't be vaccinated, like young children and the elderly, through herd immunity. Dr. Vanessa Slots highlights the crucial role of vaccines. Immunizations Your Child Needs (and when) Birth to 6 Months Hepatitis B: Shortly after birth, first vaccine dose Diphtheria, Tetanus, and Pertussis (DTaP), Polio, Haemophilus Influenza (HiB), Pneumonia, Hepatitis B and Rotavirus: Ages 2, 4 and 6 months, boosters and vaccines One Year to 18 Months MMR and Varicella (chickenpox) vaccine: Age 1, first vaccine dose Hepatitis A, HiB and Pneumonia: Age 1, booster DTaP: 15 months, fourth vaccine dose Hepatitis, second dose: 18 months Flu Vaccine: 6 months and older, annually* *In the year after receiving their first dose, an infant will need a booster one month later. Four Years Old MMRV, DTaP and Polio, final dose: Four years of age Pre-Teen and Beyond Tdap and Meningitis: Before starting middle school, children receive these vaccines. They are also old enough to start the HPV vaccine, an essential vaccine for all young adults to protect against cancer, genital warts and cervical dysplasia.
Read More About Why Childhood Immunizations Are So Important
-
What You Need to Know About RSV
Respiratory syncytial virus, also known as RSV, is a common respiratory virus that impacts the lungs and breathing pathways. The virus can be dangerous for infants and young children and is also concerning for older adults. While most older kids and adults only experience cold-like systems and recover in a week or two, an estimated 58,000-80,000 children younger than 5 years old are hospitalized due to RSV each year, and in 2022 healthcare organizations across the country are experiencing higher infection rates than in years past. "We are experiencing a strong RSV season and do not expect it to go away anytime soon," said Dr. Kris Wilson, Division Chief of Renown Children's Primary Care. "Infants who are infected with RSV almost always show symptoms of runny noses and cough. Call your healthcare provider immediately if your child is having difficulty breathing, is not drinking enough fluids, or is experiencing any worsening of these symptoms.” Symptoms of RSV: Runny nose Decrease in appetite/inability to drink Dry diapers, an indication of dehydration Cough, which may progress to wheezing or difficulty breathing Irritability (most common in very young infants) Decreased activity (most common in very young infants) Decreased appetite (most common in very young infants) Apnea, pauses in breathing for more than 10 seconds (most common in very young infants) What to do if you think your child has RSV: Call your pediatrician! If you suspect your child might have RSV, consulting their healthcare provider is the best first line of defense. From here they will help you build an appropriate treatment plan for child. Keep in mind that many pediatrician offices offer 24/7 call lines. If your child is experiencing retracted breathing (when the area between the ribs and in the neck sinks in when a person attempts to inhale), dehydration (not drinking and decrease in wet diapers) or apnea (pauses in breathing for more than 10 seconds) please call 911 or go to the closest emergency room.
-
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Understanding and Managing Childhood Asthma
Dr. Shipra Singh, a Pediatric Pulmonologist, outlines the challenges of diagnosing asthma in children due to symptoms resembling other respiratory issues. It's particularly difficult to identify in infants and young children, who may not clearly exhibit breathing difficulties. Asthma, often confused with bronchitis, croup, or allergies, is a significant chronic illness causing school absenteeism, as per the CDC. Risk factors include prenatal smoking and family history of allergies or asthma. Infants and toddlers are more susceptible due to smaller airways and respiratory viruses, which can exacerbate conditions like colds and bronchitis. How can I tell if my child has asthma? Unfortunately small children are unable to describe their symptoms, making asthma difficult to diagnose. Your child may even be active, playing and smiling, although they are experiencing chest tightness or labored breathing. Observe your child and let the child’s doctor know if: Your child’s breathing behavior has changed (coughing, wheezing, rapid breathing) Your child’s breathing pattern changes (day vs. night, with rest or activity, inside vs. outside) You have a family history of asthma or allergies Your child’s breathing is triggered by any foods or allergies With your help, your child’s doctor can make the best diagnosis to determine if your child has asthma. A pediatric pulmonologist (lung specialist) or pediatric allergist may also have to be consulted for special testing. Tests may include lung function testing, allergy tests, blood tests and X-rays for an accurate diagnosis. What is the treatment for infants and toddlers? Young children can use many of the same medications as older children and adults, although the way they take them and the dosage will differ. A nebulizer (or breathing machine) creating a medicated mist for your child to breathe through a mask may be used. An inhaler with a small spacer tube connected to a mask is also common to help your child breath medication into their lungs. Either of these options are effective. Asthma in children is treated with both fast-acting and long-term medicines to open up airways quickly for easy breathing and also to lessen asthma symptoms over time. Communicate with your child’s medical providers to create a personalized asthma management plan for them. How can I manage my child’s asthma? Recognize your child’s breathing habits and be aware of worsening symptoms. Consult with your child’s doctor on a daily asthma action plan to recognize worsening symptoms and track medications. Here’s an example of an asthma action plan provided by the U.S. Department of Health and Human Services’ National Institutes of Health). Be consistent with the plan and talk to your doctor before changing it. Have an emergency plan in case of a serious asthma attack. Know where the closest ER is and know who can take care of your other children. Also know what the medical treatment coverage is under your insurance plan. Dr. Singh explains, "Discussing asthma with your child may be difficult. Some kids find the subject frightening or confusing. Others, especially the older kids, may resent the treatment and may not be interested in doing it. Talk to your doctor about advice to build an open and trusting relationship regarding your child's asthma care."
-
6 Healthcare Action Items for the LGBTQIA+ Community
© Niyazz via Canva.com Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
Sepsis: Causes & Symptoms
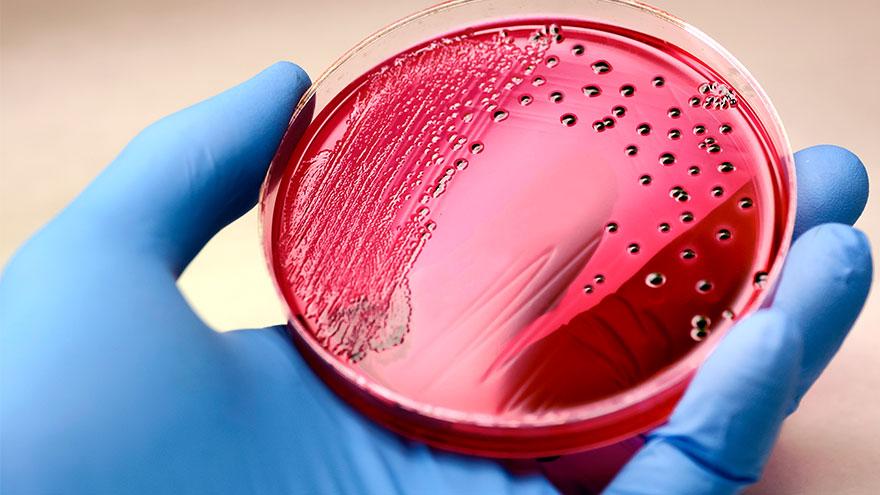
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Importance of Safe Sleep
In today's fast-paced society, it is understandable for parents to want to take shortcuts in caring for their little ones. A s a result, It is tempting to leave a sleeping infant in a car seat or swing after a long day of errands or when you need a moment to catch your breath. But, as convenient as these devices may be, they pose a serious risk to your child's safety. Why Car Seats and Swings Pose Risks for Infant Sleep Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The American Academy of Pediatrics (AAP) states that “infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical.” If a parent must use a car seat or other sitting device, they should only do so for a short period of time and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The American Academy of Pediatrics (AAP) warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. This is because infants can easily slump over or become entangled in the straps, blocking their airway, and causing suffocation. Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The AAP states: Infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical. If a parent must use a car seat or other sitting device, they should only do so for a short period and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The AAP warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. In addition, infants can easily slump over or become entangled in the straps, blocking their airways and causing suffocation.
-
What to Expect at a Well Child Checkup
A well-child checkup is a great opportunity to monitor your child’s growth and development, and it's also a chance to establish a trusting relationship with your child’s pediatrician and have your questions answered. What to Expect at Each Checkup At every checkup, a comprehensive physical examination will be conducted to assess your child's growth parameters, including height, weight and head circumference. A developmental assessment will evaluate the progress of your infant or young child in achieving age-appropriate milestones, encompassing language skills, motor development, problem-solving abilities and psycho-social skills. In addition, your pediatrician will address common concerns such as feeding, sleep patterns, oral health and general infant care. Unless there are specific needs or concerns for your baby, routine laboratory tests are typically unnecessary. Your pediatrician will provide guidance on immunization schedules, post-vaccination expectations and when to seek medical attention. Furthermore, during each visit, you will receive age-specific guidance to help you anticipate your child's expected growth and development, along with essential safety precautions and illness prevention measures. Your pediatrician will discuss various topics, such as placing your baby to sleep on their back, utilizing rear-facing infant car seats until around age two, maintaining home water thermostats below 120 degrees Fahrenheit, ensuring dangerous objects and poisonous substances are out of sight and reach, emphasizing dental health and promoting the use of bike helmets, among other things. Preparing for Your Visit It is recommended that, as a parent, you write down any questions beforehand, so you don’t forget them in the moment. Most importantly, feel comfortable asking your pediatrician about anything that might seem unusual, as you are the parent, and you know best! Before leaving the pediatrician’s office, be sure that you fully understand any instructions given to you and ask for clarification if needed. From your child’s birth through young adulthood, you will be visiting your pediatrician regularly. The American Academy of Pediatrics provides what a regular schedule might look like. Well-Child Checkup Schedule Two to three days after birth and at one month Two months Four months Six months Nine months One year 15 months 18 months 24 months 30 months Three years, and yearly after
-
10 Essential Questions to Ask at Your Child's Pediatrician Visit
Taking a few minutes to prepare for your child's pediatrician visit helps ensure that all your child's medical needs are met. Knowing the right questions to ask your provider can help you get the most out of your visit and ensure you and your child feel comfortable and informed. It is essential to base your questions on your child's specific health needs, but the ten options below are a great place to start. How is my child's overall health and development progressing? Is my child meeting their developmental milestones, and are there any areas where they may need extra support? What vaccinations does my child need, and are they up to date on all required immunizations? Are there any nutritional recommendations or concerns for my child's age and stage of development? What are some strategies for promoting healthy habits and physical activity for my child? Are there any warning signs I should look out for regarding my child's health or behavior? What can I do to help prevent common childhood illnesses like colds, flu strains or ear infections? What should I do if my child gets sick, and when should I seek medical attention? Are there any changes to my child's medication or dosage that I should be aware of? Is there anything else I should know or be aware of regarding my child's health or development?
Read More About 10 Essential Questions to Ask at Your Child's Pediatrician Visit