Buscar
-
Strategies for Lasting Weight Loss
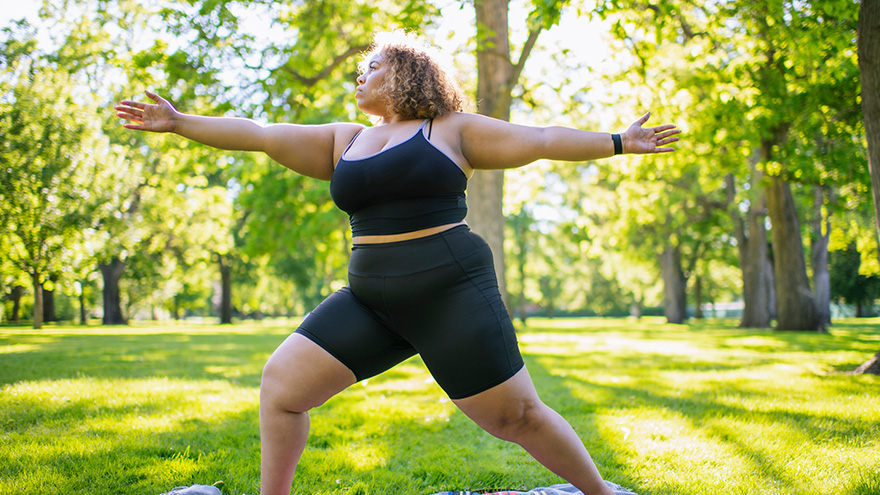
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Sepsis: Causes & Symptoms
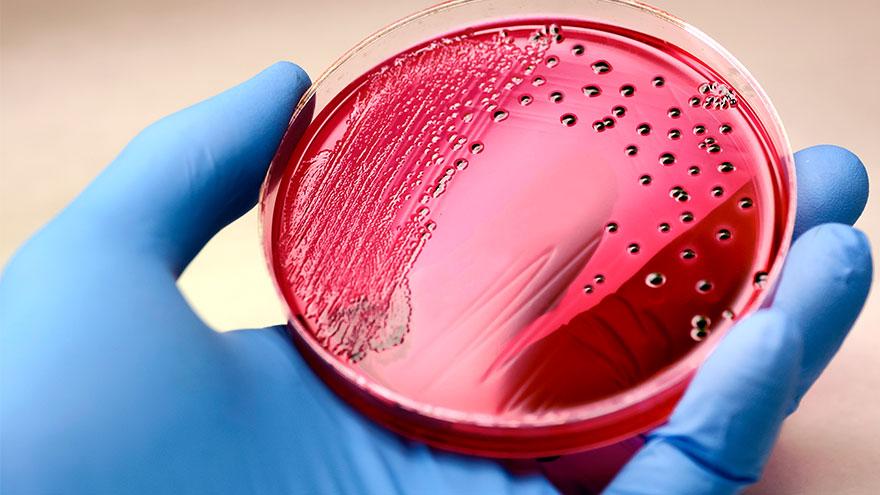
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Your Top 5 Questions about TAVR Answered
Your heart is the muscle in charge of pumping blood to your entire body. This vital organ is made up of chambers, valves and blood vessels. Your heart valves work similarly to a one-way door: they open and close, controlling blood flow in the correct direction through the heart chambers. For patients who have been diagnosed with a heart-related condition like aortic valve stenosis (narrowing), it is important to know treatment options. Most might think open-heart surgery is the only way to treat a heart valve, but many hospitals, including Renown, also offer a minimally invasive procedure called a Transcatheter Aortic Valve Replacement (TAVR). Dr. Abhilash Akinapelli of Renown Institute for Heart & Vascular Health shares his answers to the top five TAVR questions: 1. What causes aortic valve stenosis? Aortic valve stenosis can be caused by a variety of factors. The main reasons being wear and tear of the valve due to aging; genetically abnormal heart valve (bicuspid aortic valve); long-standing high blood pressure; and other reasons like radiation exposure. 2. Am I a candidate for TAVR? Renown’s heart care teams are made up of your primary care provider, cardiologist and cardio thoracic surgeon. They will evaluate if patients are a good candidate for the TAVR procedure by performing a variety of screenings and tests. Some of these include: Echocardiogram Electrocardiogram (ECG or EKG) Chest X-ray Exercise tests or stress tests Cardiac computerized tomography (CT) scan Cardiac catheterization 3. What are the advantages of the TAVR procedure? The Transcatheter Aortic Valve Replacement (TAVR) procedure is much less invasive than open heart surgery, otherwise known as a Surgical Aortic Valve Replacement (SAVR). Patients can typically return to their normal lifestyles within a week after leaving the hospital. During the TAVR procedure, a stent valve mounted on a balloon is advanced to the heart through the blood vessels in the groin without any incision. Once in position, the balloon will be inflated to firmly expand the new valve inside the diseased old valve, pushing it away to the sides. Once the new valve is in place, it begins working immediately and the deflated balloon is removed. The surgical procedure is approximately one hour long. Patients can get up and walk after four hours and will be discharged the following day if no complications arise. Compared to a SAVR, recovery time is much shorter and less risky for patients above the age of 75. A big advantage for anyone who fits under the criteria for a TAVR. 4. Is the procedure painful? The TAVR procedure is not surgery, but you will still be asleep during the procedure. Since no incision is made, it is essentially a painless procedure. Patients may experience slight discomfort such as aches and pains at the entry site of the catheter. 5. Can I have an MRI and X-rays done after having a TAVR valve? Yes, patients can have MRI scans and X-rays after TAVR. For further questions and information about the TAVR procedure, please consult with your Renown heart care team at 775-982-2452 or through MyChart.
-
Departamento destacado: Surgical Preadmission
Heading into surgery of any kind can bring along feelings of intimidation. With a best-in-class surgery team at Renown Health, patients rest assured that they are in the most capable hands for their entire procedure from start to finish – and while the physical preparation is vital, mental and emotional preparation is equally as important to ensure each patient has a smooth and comfortable experience. The Surgical Preadmission department (a.k.a. “preadmit”) at Renown Regional Medical Center and Renown South Meadows Medical Center is a dynamic and compassionate group of nurses, case managers, chart managers and more who are dedicated to guiding each patient through the surgical process. With extensive knowledge and expertise under their belt, the teams are equipped to make a genuine difference in the health and well-being of all patients, for all surgeries, at all times of the year. Surgery Starting Ground The Surgical Preadmission teams are crucial aspects in the successful outcome of every surgical procedure. Comprised of skilled healthcare professionals, this department is dedicated to providing comprehensive support and care before heading into the pre-operating room. “Our job is to prepare every patient for surgery, make sure all their pre-surgery testing is done, ensure they understand their fasting and medication instructions, have had their questions answered, have a ride home and know what to expect during surgery and after so their recovery can go smoothly and without complications,” said Debra Bennett, RN, Supervisor of Surgical Preadmission at Renown Regional. “Each patient is unique, so each experience is different.” Our preadmit nurses are the masters of communication, directing thorough assessments – including medications, tests and clearances – and addressing any questions or concerns patients may have, never missing the opportunity to inform them of exactly what they will expect in surgery. “I do a complete history on every patient while giving them detailed pre-operating instructions and helping them answer any questions to the best of my ability,” said Nancy Hilts, Surgical Preadmission RN at Renown Regional. “I am proud to be able to help allay their fears and concerns using my 30 years of pre-op experience. I offer an avenue for them to feel comfortable opening up to me.” “We always tell patients that they have great surgeons and a fantastic team that will be watching over them and taking care of them every step of the way,” added Jon Capallupo, Surgical Preadmission RN at Renown South Meadows. “We also give them plenty of educational handouts and video content, in addition to verbal instruction, to ensure they are as prepared as possible.” The nurses then pass the reigns onto the chart managers, who prepare the charts for surgery and ensure all documentation is up-to-date before sending them to the pre-operative team. The expert surgical case managers also step in to prepare a thorough discharge plan, along with reviewing pre-operation orders for status, consent, codes and more. The team does several of these initial visits virtually, and they are looking forward to soon phasing all preadmit case manager preliminary visits into a virtual model. From assisting the pre-op and post-anesthesia care unit (PACU) teams with discharge planning concerns to helping on the outpatient side with anything from oxygen equipment and catheters to transportation issues and those experiencing homelessness, our pre-admit case managers are always up to the challenge. "We are true patient advocates, alleviating concerns and fears along the way,” said Mary Carl, RN, Case Manager at Renown Regional. “Just to name a few things we do on a daily basis, we see our total joint and non-weight bearing patients during their preadmission appointment, so they are aware of the medical equipment they need and if it is covered by insurance; provide education for Aspira catheters and gastrostomy tubes; advocate to ensure tube feeding and dressing changes are set up for hospice and home health patients; and escalate concerns of patient safety to ensure a safe discharge.” In the midst of it all, there is never a dull moment in the preadmit teams. At Renown Regional alone, the preadmit professionals see more than 1,600 patients a month – and each one has a hyper-personalized experience with their very own preadmit team. “Many times, we are the first impression a patient has on our organization; after all, we touch more than 97 percent of patients that are scheduled for surgery, cardiac catheterization lab procedures or interventional radiology,” said Amy Schler, Surgical Preadmission RN at Renown Regional. “We also collaborate with many other departments in the hospital as well, from surgeons and anesthesiologists to case managers and nurse navigators. Our work in preadmit impacts the entire surgical process.” Holding a diverse array of experiences, our preadmit department plays an integral role in our commitment to providing the highest quality of care to every patient. Knowledge is Power Heading into surgery feeling fearful and worried is normal for any patient. However, how would you feel knowing that each individual member on your preadmit team has, on average, 23-25 years of experience in the field? This is the reality for our Surgical Preadmission department – and they put that vast knowledge to great use to bring a sense of calm to patients. “Our team members have worked in various departments within our organization, and they bring a wealth of knowledge that we share with each other, and most importantly, with our patients,” said Amy Schler, RN. “If you have hundreds of years of nursing experience, you can speak not only as a nurse but also as a patient. It allows you to give a more personal perspective on what patients can expect in their recovery. Being able to assess their emotions and provide feedback to our pre-op and PACU teams help the patient have a better experience.” “Many of our nurses have close to 40 years of experience each, and they have an extremely large knowledge base since we see patients from newborn to geriatric and from easy procedures to complex surgeries,” added Debra Bennett, RN. “Another great aspect of our team is the varied nursing backgrounds we all hold – surgery, pre- and post-op, labor and delivery, pediatric intensive care, cardiology, gastroenterology, urology, cardiac cath lab, home health and everything in between. Communication between departments is so important!” All members in this department, regardless of which clinical area they came from, surgical or non-surgical, can easily translate their skills into the work they do in preadmit – and they only continue to grow. “As a surgical preadmission nurse, I have used my years of experience as a nurse in surgical services,” said Terri Delatorre, Surgical Preadmission RN at Renown Regional. “I started as a floor nurse with orthopedics for 12 years, and then I worked with the PACU for 11 years. This has helped me give great understanding and care to our surgical patients.” “Because we have staff with such a vast knowledge base, we can rely on our years of working within our organization to help alleviate fears that the patient may have,” added Amy Schler, RN. We can prepare them for what to expect in pre-op and PACU and educate them on what to expect post-op, including any barriers they may face. For example, mastectomy patients may not realize they will not be able to raise their arms for 7-10 days post-op, and total knee patients have to navigate stairs and housing access. Helping patients think about barriers at home that they may not have thought about helps them prepare prior to surgery, enhances their healing and provides a better surgical experience.” The preadmit team works closely with our best-in-class surgeons and anesthesiologists, continuing to grow their expertise along the way while learning alongside our talented providers. For instance, when it comes to our Renown South Meadows preadmit department, anesthesiologist Nariman Rahimzadeh, MD provides excellent guidance for the entire team on state-of-the-art anesthesiology practices. “I am very proud of the work we do with Dr. Rahimzadeh,” said Lisa Closson, Surgical Preadmission RN at Renown South Meadows. “Together, we ensure patients are safe for both surgery and anesthesia.” Despite the challenges that come their way – whether it be changes to process and workflow to navigating support for patients after they leave the surgery floor – the preadmit team cleverly uses their collective wealth of knowledge to bring hope and comfort to all patients. “Our nurses are such warm, caring and compassionate humans that do their best to ease any fears and anxieties patients may have,” said Debra Bennett, RN. The Pride of Preadmission The pride of our preadmit team lies in their ability to make a positive impact on all patients they serve. To them, their work is not just a job – it's a calling. And they do it all while working together to elevate their team and performance. “Our team is most proud of the quality of care we provide to our patients and our abilities to troubleshoot difficult situations to ensure they have a great surgical experience here at Renown,” said Mary Carl, RN. The entire department supports each other by working collaboratively and relying on each other’s expertise to provide the best possible care for patients. They understand that their success as a team depends on their abilities to support and help each other. “Our team is awesome here at South Meadows,” said Jon Capallupo, RN. “We can turn to each other for support, and we all work very well with each other. I am glad to be a part of this team.” “I am proud of how well all of us in preadmit works with each other every day,” added Lisa Closson, RN. “We try to make patients feel comfortable from the moment they arrive to the time they leave the department.” The pride that our preadmit team expends goes beyond their departmental limits – these team members are also trusted teachers. They work closely with cancer nurse navigators to teach weekly classes for patients who have been newly diagnosed with breast cancer, coupled with lymphedema prevention and education classes. The team also encourages participation in Renown’s free smoking cessation programs to help their patients learn the risks and benefits of quitting smoking. When not serving patients or teaching classes, you can find many of these team members taking charge of multidisciplinary committees within our health system, including breast leadership, gastroenterology leadership, shared governance, infection control and recruitment and retention. On top of it all, this team certainly knows how to celebrate, with several of their members being a part of their own department-wide Celebration Committee, where they gather for retirement parties, baby showers and team get-togethers. Always active and never passing up a challenge, our preadmit department are shining examples of Renown’s Culture Commitments, especially Caring and Collaboration, and the pride in the vital work they do every day is limitless. “I am so happy my position in preadmit opened up for me at a time when I was really feeling challenged in my career,” said Nancy Hilts, RN. “The team that we have here is amazing. I am so grateful and thankful every day for the opportunity. It is an amazing place to work!”
-
Excellence in Heart Care Changes a Patient's Life
Being diagnosed with a chronic heart condition like atrial fibrillation (A-fib) can shift the course of your entire life. Embracing heart medications and lifestyle changes become your norm, and thanks to advancements in medicine and medical technology, managing the condition can bring you to a new sense of normalcy. But what if a different option was possible – one that would make medications and activity limits a thing of the past? This became the reality for Renown Health patient Richard Preyer after receiving a hybrid catheter ablation. Thanks to the vigilant surgical care of Shining Sun, MD, a cardiologist at the Renown Institute for Heart & Vascular Health, and his compassionate team, Richard has a new lease on life. Minimally Invasive with Maximal Results An A-fib patient since 2010 who had been living with an unfinished ablation, the 59-year-old Carson City resident turned to the internet to look for alternate solutions. He had heard that the Renown Institute for Heart & Vascular Health was a top-tier location for cardiovascular care. “I changed health insurance plans through Nevada Health Link to ensure I could see a Renown cardiologist,” said Richard. Choosing a cardiologist was an even easier decision for Richard. Dr. Sun’s introductory Find a Doctor video on Renown’s YouTube channel, where he displayed his expertise and determination, was more than enough for Richard to choose him as his cardiac care leader. At his first visit, Dr. Sun reviewed Richard’s records, and noted his prior unfinished ablation. The nine-hour procedure had been performed several years ago. With the enhanced technologies at Dr. Sun's disposal, Richard was excited at the thought of his life potentially being changed for good – with a minimally-invasive solution. Dr. Sun collaborated closely with Richard’s previous and current care teams – including a surgeon who performed a maze operation on him right before his surgery at Renown, to ensure his hybrid ablation was tailored uniquely to him. “Dr. Sun is clearly a very powerful cardiologist with many connections, and the coordination between his team and my other doctors was great,” said Richard. After working on the exterior of the heart in the first phase of the surgery and the interior of the heart during the second phase, Richard’s hybrid ablation was successful, completing the unfinished portion of his previous ablation. “Fixing A-fib can take one to three ablations, and sometimes it never holds,” said Richard. “That is one of the largest reasons why I am so thankful for this procedure and how it ended up.” Life After A-fib Now comes the long, arduous healing process, right? Not for Richard. With only eight incisions (four on each side of his chest), he was able to remove his bandages after two days, and he healed completely in one week. “I was even back to taking three-mile walks within a week of my operation,” said Richard. No more blood thinners. No more activity limits. And most importantly for Richard, no more heart-stabilizing medications that came with side effects he didn’t enjoy. He attributes his enhanced life to Dr. Sun and his team. “I highly recommend Dr. Sun and everyone that works with him,” he said. “Everyone in the group, from the nurses and anesthesiologists going above-and-beyond to the schedulers who helped me navigate the appointment process, made me have a lot of confidence. Their calm demeanors made so much difference.” Today, Richard now enjoys elongated walks in the northern Nevada outdoors, exotic vacations with his wife and, as he describes, “feeling like I’m in my 40’s again.” Learn more about the region's leader in cardiac health, heart and vascular care here.
Read More About Excellence in Heart Care Changes a Patient's Life
-
Lung Cancer Screening and Early Detection
Lung cancer is the leading cause of cancer deaths in both men and women in the U.S. The good news is the five-year survival rate increases dramatically if lung cancer is treated before spreading to other parts of the body. Julie Locken, MD, of Renown Health Imaging, explains more. What are the signs and symptoms of lung cancer? As you might expect, most lung cancer symptoms appear in the chest and can affect your breathing. Watch for signs such as: Persistent cough Constant chest pain Shortness of breath Wheezing Bloody or rust-colored phlegm Hoarseness Swelling of the neck Pain or weakness in the shoulder, arm or hand Recurring pneumonia, bronchitis or other lung infections Loss of appetite and loss of weight can also be signs of lung cancer That said, there are usually no symptoms in the early stages of lung cancer, which means getting screened can truly be a lifesaver. If you have a history of smoking, you should get screened as a precaution. What are the risk factors of lung cancer? Around 80% of lung cancer cases stem from a history of smoking tobacco. But there are other known causes, such as secondhand smoke, radon, asbestos and diesel exhaust. It’s important to do what you can to eliminate exposure to all of these to reduce your lung cancer risk. People with an immediate relative – a parent, sibling or child – diagnosed with lung cancer and people between 50 and 80 years old are also at higher risk and may need to consider screening. People who are at the highest risk are those with a history of smoking tobacco, particularly smokers who averaged one pack of cigarettes per day for 20 years or more, as well as former heavy smokers who quit in the last 15 years.
-
Monkeypox: A Renown Expert Weighs In
Renown Health is closely following the national outbreak of the monkeypox virus and urging healthcare providers to be alert for patients with illnesses associated with a rash. In working with the Washoe County Health District (WCHD), Renown is closely monitoring the spread of monkeypox in the community and looking to prevent and reduce the spread of monkeypox. To help to ease worries, we consulted with Paul De Leon, Infection Preventionist at Renown Health. What Exactly is Monkeypox? Monkeypox is a rare viral illness caused by the monkeypox virus — the same family of viruses that causes Smallpox. Although symptoms are similar to Smallpox, monkeypox symptoms are milder and rarely fatal. However, it's important to mention that this virus can be more severe for these susceptible groups: Immunocompromised Pregnant women A fetus or newborn baby Women who are breastfeeding Young children Those with severe skin diseases such as eczema How is Monkeypox Transmitted? The monkeypox virus is not easily transmitted but occurs through sustained person to person close contact with an infected individual. Monkeypox can also be transmitted through direct contact with infectious rash, scabs, or body fluids. Monkeypox can also be spread through prolonged intimate physical contact, such as kissing, cuddling or sex. Lastly, monkeypox can be spread through contaminated linens or bedding. Transmission through respiratory secretions is uncommon but has been reported after prolonged face-to-face contact with symptomatic individuals. In addition, pregnant women can spread the virus to their fetuses through the placenta. Monkeypox Testing If you think you have monkeypox, contact your primary care physician or other medical providers to obtain testing. Notify the provider ahead of time before entering the physical office. Signs & Symptoms This current outbreak of West African monkeypox does not have the typical presentation of classic monkeypox. Symptoms usually appear one to three weeks after infection and include: Pimple-like rash or blisters on the face, inside the mouth, and on other areas of the body, like the hands, feet, chest, genitals, or anus. The rash will go through serval stages, including scabs, before healing and may be painful or itchy. Other symptoms of monkeypox can include: Fever Headache Muscle aches and backache Swollen lymph nodes Chills Exhaustion Respiratory symptoms such as sore throat, nasal congestion, or cough Symptoms of monkeypox may occur before or after a rash with some individuals only report experience a rash. Individuals with monkeypox are infectious once symptoms begin and remain infectious until lesions form scabs, scabs fall off, and a fresh layer of skin forms. The illness typically lasts 2-4 weeks.
-
Dos años que no olvidaremos: la COVID-19 en Renown Health
On March 19, 2020, Renown Regional admitted the first patient in need of care while sick with COVID-19. Our providers navigated two years of a pandemic and overcame many challenges while providing the best care for our patients and the community. Anicia Beckwith’s series “The Art of Healing” captured Renown Health during this time. Let's take a look back on the last two years. February 2020: Standing Up the Hospital Incident Command System (HICS) On February 25, 2020, leaders at Renown Health stood up Renown’s Hospital Incident Command System (HICS), a standardized system used to organize response personnel and resources and manage response operations during emergencies and crises. March 2020: Temporary Deployable Medical Structure Placed Outside Renown Regional Emergency Department On March 12, 2020, Renown set up a deployable medical facility to serve as a respiratory illness screening center for emergency room patients at Renown Regional. A similar tent was also set up outside the emergency room at South Meadows Medical Center. This proactive measure helped our teams care for community members with respiratory illness symptoms while protecting patients and staff in the emergency department and other areas of the hospital. Check out photos of the tent here. Read the Reno Gazette Journal Article about the tent here. April 2020: Alternate Care Site at Mill Street Parking Structure at Renown Regional Renown’s HICS team decided to create an Alternate Care Site (ACS) in the Renown Regional Medical Center Mill Street parking structure. The ACS served additional hospitalized patients and allowed caregivers to remain on campus and still have access to existing hospital infrastructure such as lab, pharmacy, imaging, food services and other critical services. After just 10 days of construction, the ACS was completed on April 3, 2020 with space to hold up to 1,400 patients. Check out photos of the ACS under construction here. On Nov. 12, 2020, Renown opened the ACS to serve additional hospitalized patients diagnosed with COVID-19 who were clinically stable or improving. Healthcare workers at Renown cared for hundreds of patients at this site. In early Jan. 2021, the remaining patients returned home. Check out the video of Connie, a patient who received care in the ACS. April and July 2020: The LOVE Sculpture Placed at Renown Regional On April 16, 2020, during a time of darkness and uncertainty, Artown loaned Renown the LOVE sculpture, a one-ton aluminum piece of art created by artist Laura Kimpton and fabricated by Jeff Schomberg. The structure, which originally debuted at Burning Man, was lit up Renown Regional's main entrance on Mill St. Watch a video about the LOVE sculpture’s debut at Renown Regional. On July 13, 2020, thanks to the support of former board chair and community supporter Blake Smith and the Keyser Foundation, the LOVE sculpture is now a permanent fixture at Renown Health. Throughout the pandemic, it has served as a source of inspiration, hope and positivity for our community and care providers. Check out a video of the LOVE is Here to Stay celebration. June 2020: Renown Offers In-House COVID Testing In June 2020, the Renown laboratory team sprang into action to help meet the growing demand for COVID-19 testing amongst Washoe County residents and businesses. Renown invested in expanded staffing and in-house testing capabilities that ensured our teams could swab and process up to 1,000 COVID-19 tests for patients each day. All with results returning within hours. November 2020: Renown Introduces “Hospital At Home” Remote Monitoring In November 2020, six patients at Renown Regional Medical Center and Renown South Meadows Medical Center diagnosed with COVID-19 were outfitted with a remote Hospital at Home monitoring system. Renown clinicians plan to continue using this system to monitor upwards of 1,000 hospitalized patients and lower acuity patients from their homes. December 2020: Renown Administers COVID-19 Vaccines to Health Care Employees On Dec. 17, 2020, Renown began to vaccinate its healthcare workers. Among those receiving the first vaccines was Luis Martinez, a technician on Renown’s Clinical Decision Unit who cared for patients recovering from COVID-19 in the Alternate Care Site field hospital. Read the Reno Gazette Journal article about the COVID-19 vaccine rollout at Renown. January 2021: Renown Administers COVID-19 Vaccines to Community After several weeks of successful employee and volunteer drive-thru vaccination events, Renown supported the Washoe County Health District and the state in vaccinating Washoe County community members. Click here for a playlist of videos featuring Renown Health employees and patients talking about the importance of the COVID-19 vaccine. February 2021: Local Widow Inspires Renown to Change Visitor Supporter Policy Darlene Randolph’s husband Dave spent 17 days hospitalized at Renown Regional Medical Center before losing his battle with COVID-19 on December 13, 2020. Darlene wrote a passionate letter to Renown Health asking for the visitor policy that allowed patients with COVID-19 to receive visitors. In February 2021, Renown hospitals were among the first in the country to lift visitor restrictions for patients with COVID-19 to encourage families to be at the patient's bedside. Read Darlene’s full story here. May 2021: Renown Celebrates Volunteers, Partners and Community Who Aided in Vaccine Efforts In May 2021, Renown administered the last dose of COVID-19 vaccines to community members in Renown’s drive-thru clinic. Between January and May 2021, over 80,000 doses were administered at the drive-thru. View drone footage of this effort here. Click here to see pictures of vaccine volunteers and employees. November 2021: Renown Offers Vaccine for Children Ages 5+ In November 2021, Renown vaccinated children in the Reno-Sparks community with the 2-dose series in a limited round of weekend clinics. The vaccine clinics featured therapy dogs, local mascots and donuts donated by Doughboy’s Donuts. Click here to see pictures of the children’s vaccine clinics and watch a video about the clinics here.
Read More About Two Years We Won't Forget: COVID-19 at Renown Health
-
Avoid Counterfeits and Find the Right Protective Mask with This Helpful Guide
To better protect our patients, visitors and employees, cloth masks are no longer allowed at Renown facilities. Surgical masks, KN95 and N95 masks are allowed at Renown facilities. Appropriate face masks will be provided for visitors and patients who need one. With recent surges in the infectious COVID-19 omicron variant, many have sought to upgrade their face masks. But, let’s face it, shopping for face masks with adequate protection can be a challenge, especially considering the countless variations and the rise of counterfeit masks. Follow our straightforward guide below which includes some common red flags to help you discern between a high-quality face mask that provides proper protection and those that may be counterfeit. Types of Masks Qualities of a Real N95 Respirator Mask According to the National Institute for Occupational Safety and Health (NIOSH), N95 approved masks form a tight seal around your face and include a disposable respirator that removes particles including bacteria, viruses and dust as you breathe. N95 masks that are NIOSH approved undergo strict quality assurance and performance requirements to ensure mask respirators filter out up to 95% of hazardous particles. As a rule of thumb, N95 masks will not have ear loops, commonly used in cloth or surgical face masks. N95 respirators will contain two elastic bands or head straps that fasten behind the head, one securing the crown of the head and the other resting at the base of the neck, providing a snug fit and seal. Some other common signs that an N95 might be counterfeit include lack of all proper labeling, misspellings of NIOSH, decorative fabric and claiming to be approved for children. Currently, masks in adult sizes are the only masks to undergo NIOSH’s quality assurance and testing process. Respirators approved by NIOSH will include a testing certification (TC) approval number and will contain specific labeling on the facepiece of your mask. Find a full list of Center for Disease Control (CDC) and NIOSH requirements here. Identifying Real KN95 Respirator Masks Often preferred due to comfortability, the KN95 respirators were initially designed to meet Chinese standards for medical masks. Firstly, if a KN95 mask claims to be approved by the CDC, it is counterfeit as the CDC and NIOSH do not support any respiratory protective devices according to international standards. However, when KN95 masks are fitted and worn appropriately they do provide more protection than disposable masks. Legitimate KN95 masks will display a manufacturer number, GB2626-2019, ensuring accordance with current Chinese respirator standards for all masks made after July 1, 2021. Unlike N95 masks, it is important to note that KN95 masks are available in children's sizes. You might run into KN95 masks claiming to be “FDA (Food and Drug Administration) approved” or “FDA-registered,” but be aware that this does not mean much and is a misleading statement. What this indicates is that a mask maker has submitted paperwork to the FDA, but the product has not been thoroughly tested for proper filtration and protection. Surgical Masks Medical procedure masks often referred to as surgical or disposable masks vary in their protection according to a variety of factors including fit and filtration. The CDC defines medical procedure masks as “variably shaped, including flat pleated, cone-shaped, or duck-bill. Medical procedure masks are loose and are not expected to provide a reliable level of protection against airborne or aerosolized particles as N95 respirators regulated by the National Institute of for Occupational Safety and Health.” However, these types of masks provide more protection than cloth masks and are certainly better than wearing no mask at all. Often popular due to their level of comfort and cost-effectiveness, surgical masks can be knotted in the ear loop areas to provide a tighter seal and can be layered for additional filtration. Depending upon your budget and level of comfortability and protection, one variation of mask may suit you over another. Please remember to do your part in limiting the spread of COVID-19 and wear a surgical mask, KN95 or N95 mask when visiting Renown facilities.
Read More About Avoid Counterfeits and Find the Right Protective Mask with This Helpful Guide
-
Vacunas de refuerzo contra la COVID-19, lo que debe saber
Getting the COVID-19 booster is the best way to protect yourself from severe illness or death due to COVID-19, and both the CDC and the FDA have approved booster shots for people ages 18 and older. So, with the holidays right around the corner and infection rates on the rise both in Nevada and nationally, the best thing you can do to prevent the continued spread of this deadly virus is to get boosted today. The Basics: Who: It is recommended that everyone 18 years or older get a COVID-19 booster shot. When: At least 6 months after completing your primary COVID-19 vaccination series. What: Any of the COVID-19 vaccines authorized in the United States. The CDC allows for mix and match dosing for booster shots. How: To make an appointment for your COVID-19 vaccine booster, please visit vaccines.gov today. Appointment Reminders: Don’t forget to bring your CDC vaccination record card to your appointment. Refresh yourself on the potential side effects and remember that these are normal signs your body is building up protection. Commonly Asked Questions: Q: Does anything change if I received the Johnson & Johnson as my first COVID-19 vaccine? A: If you received the Johnson & Johnson COVID-19 vaccine, you are elidable for a booster two months after completing your primary vaccine. Q: Is the formula the same for the boosters as it was for the primary vaccine? A: COVID-19 booster shots are the same formulation as the current COVID-19 vaccines. However, in the case of the Moderna COVID-19 vaccine booster shot, it is half the dose of the vaccine people get for their primary series. Q: Am I still considered “fully vaccinated” if I don’t receive a COVID-19 booster shot. A: Yes, everyone is still considered fully vaccinated two weeks after their second dose in a two-shot series, such as the Pfizer-BioNTech or Moderna vaccines, or two weeks after a single-dose vaccine, such as the J&J/Janssen vaccine. All information courtesy of the Center for Disease Control and Prevention. All information courtesy of the Center for Disease Control and Prevention
Read More About COVID-19 Booster Shots, What You Need to Know
-
Viuda de Reno inspira una nueva política de visitantes para Renown
Renown Health is one of the country’s first health systems to lift visitor restrictions for patients with COVID-19 and encourage the family to be at the patient’s bedside. Read Darlene and Dave’s story to understand why we’re updating our visitor policy. Dave and Darlene Randolph found joy in exploring antique shops and garage sales to find damaged or discarded vintage pieces. Dave would spend many hours scraping, cleaning, sanding, and refinishing items, transforming them into functional, beautiful pieces of furniture. Every piece in their home rekindles a memory and has a story to tell. On Thanksgiving, when Dave was too ill to gather around their antique dining room table, Darlene called the ambulance. Ailing with COVID-19 for two weeks, Dave had not been improving. When the EMTs reached her home and asked Darlene what underlying conditions he had, she said, “all of them.” David was seriously ill. Hospitalized for COVID-19, their communications options were limited. The only way Darlene could communicate with Dave was on a video call or by telephone. Dave spent 17 days hospitalized at Renown Regional Medical Center in Reno. Darlene spent 17 days waiting by the phone for more information on his condition. Darlene said he had “up days and down days,” but thought he might be home, sitting at their antique dinner table for Christmas. Sadly, Dr. David Randolph lost his battle with COVID-19 on December 13, 2020, and died as he slept in a hospital bed. When Darlene wrote his obituary for the newspaper, she gave thanks to the “tremendous nurses and doctors at Renown Regional Medical Center, for providing his care during a time when the family could not be with him.” Taking Action to Inspire Change Darlene wished she could have been there. Over their 45-year marriage, she had always been there. Darlene said, “I had always been at his bedside, as his advocate, to help communicate and straighten things out.” As a registered dietician, she worked in hospitals, knew the protocol, and knew that Renown had a restricted visitor policy to stop the virus’s spread- to other patients, staff, and their family members. Still, she wished she could have spent more time with him. On Christmas Eve, she sat down and wrote to Renown leadership. “As the wife of a COVID patient who recently passed away in your hospital, I want to express my thanks to you and your staff for the care he received in the last days of his life. I am aware that the nurses and staff are working under dangerous conditions and risking their health and lives by caring for multiple COVID patients. The staff is gracious, concerned, and doing everything they can.” She continued, “I know procedures are changing every hour to try to stay ahead of this dangerous virus, and I am sharing my experiences, hoping they will be helpful when establishing policies that impact families.” Darlene explained that despite receiving assurances that Dave’s nurse or a doctor would call daily, sometimes they would forget. She explains in her letter, “how important it is, in these times when the family cannot visit, and has only infrequent communication and is anxiously waiting at home for information about their loved one, how much it means to get a call from someone caring for him at the hospital. If there is a way you can help assure nurses have time to make calls or assist patients in making calls because it is an important part of patient care.” A Person-Centered Visitor Policy After receiving her letter, Renown leadership called Mrs. David Randolph to thank her, offer his sympathies and ask if Renown could help in any way. Darlene asked if he might reconsider allowing families to visit hospital patients during treatment for COVID-19. As the COVID-19 situation has evolved, the policy has as well. Renown hospitals and medical practices now encourage limited visitors for all patients, including those diagnosed with COVID-19. Renown also has extra safety measures to protect the health of patients, visitors and healthcare employees. Darlene is very pleased that her letter inspired this shift in visitor policies for patients with COVID-19. She says, “I have always tried to think of ways I could help other families. Especially those senior couples where one has been hospitalized and the other is home. My wish is to help others.” Renown Health Visitor Policy Renown Health patients may identify two healthy adult “patient supporters” to accompany them on their hospital stay. For more details, visit our Patient Supporter Guidelines page.
Read More About Reno Widow Inspires New Visitor Policy for Renown