Buscar
-
8 pruebas de evaluación de la salud importantes para hombres
Men are generally less likely to visit their doctor for exams, screenings, and consults compared to women. To address this, we've collaborated with Dr. Bonnie Ferrara of Renown Health, to compile a list of eight essential screenings that can help men maintain their health. 1. Blood Pressure Tests Ages 20+ Blood Pressure tests measure the pressure in your arteries as your heart pumps. Biennial (every two years) checks are recommended if you have normal blood pressure or more frequently if you have high blood pressure (hypertension) or low blood pressure (hypotension). The United States Preventative Services Taskforce cites normal blood pressure below 120 systolic (top number) and 80 diastolic (bottom number). 2. Cholesterol Screening Ages 20+ High levels of cholesterol increase your risk of stroke and heart disease. A simple blood test will help your healthcare provider determine your numbers and if you're at risk. If you have a family history of diabetes or heart disease, you may need yearly screenings. But, again, your doctor can provide the best course of action.
-
How to Spot Depression in Men
Is a man in your life struggling with depression? Many men find it difficult to acknowledge when they need help. Recognize their unique warning signs of depression with insights from psychologist Dr. Herbert Coard. Over 6 million men are diagnosed annually, often displaying symptoms like anger and aggression instead of sadness. Learn how to support them and understand these often-misinterpreted indicators. Behavioral Signs of Depression in Men High levels of the hormone cortisol are released during stressful situations affecting the neurotransmitter, serotonin (a feel-good hormone), contributing to depression. You can identify depression or suicidal tendencies by paying close attention to the following behavioral changes: Anger, irritability, or aggression Avoiding family or social situations Losing interest in family responsibilities, passions and hobbies Lack of sex drive Becoming controlling/abusive in relationships Risk-taking behavior such as; unsafe sex, overspending or gambling Not being able to concentrate or remember details Excessive drinking or drug use Having frequent thoughts about death Talking about suicide Attempting suicide Factors That Lead to Depression in Men Life Events Work stress or long-term unemployment can be huge contributing factors relating to depression. This type of life event can be overwhelming, making it impossible for a man to cope. Changes in Relationships The loss of a relationship can be a significant contributing factor to the emergence of depressive symptoms and past experienced physical, sexual, or emotionally abusive relationships. With this in mind, counseling can often help individual to overcome this type of trauma. Grief and Loss Overwhelming sadness due to the loss of a loved one can trigger depression. Although normal, each person goes through their own grieving period. For example, normal responses to death are insomnia, poor appetite and loss of interest in activities. Pay attention if grief seems prolonged or out of the ordinary. Health Problems In particular, depression coexists with medical conditions. As men age, this can be passed off as normal aging, but it could be more serious. In addition, illnesses such as thyroid disorders, Addison’s disease and liver disease can cause depressive symptoms. Diabetes, cancer, heart disease, or Parkinson’s disease can affect any age, thus triggering or worsening depression. Some older men also feel like they may be suffering from dementia because of difficulties with memory this may be a symptom of depression. A trip to the doctor may be in order to help alleviate concern and worry. Depression in Men and Suicide Frequently the emotional pain occurring with depression can distort a man’s ability to see a solution beyond suicide. Individuals with depression become very rigid and constricted in the way they solve problems. The statistics below speak for themselves, helping us understand the need to reach out to those who need our support. Male suicide rates are on rising – men die by suicide 3.53 times more often than women, accounting for 70% of all suicides. Sadly, every day 129 men commit suicide. White males accounted for 69.67% of suicide deaths in 2017. In 2017, firearms accounted for 50.57% of all suicide deaths. Middle aged Men who are middle aged have the highest suicide rates. 40% of those identifying as transgender have attempted suicide in their lifetime. Males who are guy or transgendered are at an increased risk for suicide attempts, especially before age 25. Veterans often suffer from post-traumatic stress disorder (PTSD) and depression, and are more likely to act on a suicide plan. How You Can Help Now that you can identify some of the warning signs of depression, here’s how you can help: Talk about your concern and communicate that you’re there to help him. Let him know depression is a medical condition and will usually get better with treatment. Suggest professional help from a Primary Care Provider, Psychologist or Therapist. Help set up appointments and offer to accompany him – let him make the decision, but make it clear you’re there for him, no matter what he decides. If you feel he is in a dire or life-threatening situation, contact 911. Call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to talk to a trained counselor. Call the Veteran’s Crisis Line at 1-800-273-TALK (1-800-273-8255) and press “1”
-
Departamento destacado: Special Procedures
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
Optimizing Mammogram Screenings: A Genetic Approach to a Personalized Screening Schedule
© Arthon Meekodong via Canva.com Breast cancer screening has long been a cornerstone of women's healthcare. With 1 in 8 women diagnosed with breast cancer in their lifetime1, the United States Preventive Services Task Force (USPSTF) has developed screening recommendations to help detect early-stage cancer. Notably in 2023, the USPSTF revised the recommended age for biennial mammogram screenings for women with average risk to start at age 40 instead of 502, estimated to result in 19% more lives being saved3 by starting screening earlier. While initiating screening at an earlier age offers advantages to a wide demographic, concerns about the potential of over-screening prompted research into the feasibility of identifying women with lower breast cancer risk who could safely delay mammograms. While guidelines address high-risk individuals, a notable gap exists in providing recommendations tailored to those at lower risk. To gain insight into a patient's risk level, physicians are able to utilize genetic testing to understand an individual's genetic makeup, providing precise insights into their predisposition to various health conditions, including breast cancer. Armed with this genetic information, healthcare providers could craft tailored screening strategies that align with an individual’s specific risk profile. This genetic risk-based approach underscores the value of genetics in individualizing the onset of screening to help avoid over-screening and its associated costs. Surprisingly, genetic information is not currently being widely utilized to identify women at risk of breast cancer or other diseases in clinical practice, despite its potential to make a significant positive impact for patients. A recent retrospective analysis of 25,591 women from the Healthy Nevada Project4 sheds light on the potential benefits of this genetic risk-based approach. The study classified 2,338 (9.1%) of these women as having a low genetic risk for breast cancer. What's remarkable is that these women exhibited a significantly lower and later onset of breast cancer compared to their average or high-risk counterparts. This finding suggests that it might be safe for low-risk women to delay mammogram screening by 5 to 10 years without compromising their health.
-
20 Years of Compassion and Dedication
When you meet Poeth Kilonzo, Director of Oncology Nursing at Renown Health, you are immediately greeted with a warm smile that puts your mind at ease. Within the William N. Pennington Cancer Institute, Poeth enjoys a strong reputation among her employees and patients as someone they can always rely on, no matter how rough the tides may flow. As an incredibly humble oncology professional, you may not realize that behind that smile is the power of a best-in-class nurse and leader holding a 20+ year career of diverse nursing experience and leadership excellence – dedicating the majority of her service to Renown Health. Join us as we dive into Poeth’s unique journey through Renown. Finding Her Passion Ever since she could remember, Poeth has been a “people person.” Above all else, she cared for people – and she cared a lot. What better place for her to be than healthcare? After moving to northern Nevada from Kenya, she began working in private patient care working with home health and dementia patients while taking classes at Truckee Meadows Community College (TMCC) in 2000. One day, a patient asked her a question that would change the course of her career journey: Did you ever think about becoming a nurse? Driven by not only the words of encouragement of her patients and supervisors in home health but also the rallying support from her family and friends, including her husband and high school friend, who both have decades of experience interacting with nurses in healthcare (with her husband spending many of those years at Renown), Poeth knew this was the path she was meant to take. “That was it; it was like a light switch had flipped,” said Poeth. “I switched to nursing overnight.” According to Poeth, TMCC’s nursing program offered her an incredibly supportive environment, which was especially important as she was a young mom at the time. Working in healthcare, going to nursing school and raising a family all at the same time is no easy task, but to Poeth, this was her calling. “Regardless of my path, I knew I wanted to be a nurse that was close to patients, sitting with them and holding their hand throughout their treatment,” said Poeth. During nursing school, Poeth completed clinicals at several hospitals in Reno – three of them were at Renown Health (known as Washoe Medical Center at the time). What immediately stood out to her was the passion of the pediatrics unit, especially in the neonatal intensive care unit (NICU). “While I knew that pediatrics wasn’t going to be my arena, some of the best times in my life were during my pediatrics clinical,” said Poeth. “It opened me up to how welcoming Renown is.” While doing her rotations, nursing leaders helped Poeth and her fellow classmates discover Renown’s Nurse Apprentice program, an apprenticeship designed exclusively for local northern Nevada nursing students. One of those leaders asked her, “have you considered doing a rotation in oncology?” And another light switch flipped. “Bingo. I am becoming an oncology nurse apprentice,” Poeth recalls. And that’s exactly what she did. After her four-month apprenticeship ended in February 2002, she walked into her interview with Joanna Gold, who would end up being her supervisor and one of her greatest mentors until she passed away in recent years. With her experience and enthusiastic spirit on her side, Poeth fervently expressed her passion and interest in working in oncology. And Joanna saw all of that and more. In June 2002, Poeth was presented with a two-year oncology RN contract, which she easily signed – however, she knew right then and there but she was not going anywhere. Renown was her home, and oncology ignited the fire within her. “The nurses in this unit are part of what kept me here,” Poeth remembers. “These nurses would really do anything for their patients. The commitment and love they all had for one another truly was like family. It inspired me to learn more and give even better care to my patients." To Poeth, it didn’t feel like she was coming to work just to do a job – she was following her dreams. “You don’t think about the work you do; you think about the service,” said Poeth. From there, Poeth spent three years on the floor as an oncology RN and became a night shift supervisor in 2005. She was thriving. But this part of her journey was only the beginning. When Opportunity Arises, Take It In March 2007, Poeth and her husband welcomed their third child – and for her, working a day shift position would serve her the best at her current stage of life. This revelation led her down to Renown South Meadows Medical Center, where she became a staff nurse in Medical Telemetry. It was in the telemetry unit where Poeth contributed to one of the largest digital transformations Renown would ever go through: transitioning from paper records to electronic records on EPIC. From there, Poeth was inspired to get back into leadership in 2012 as the Supervisor of Clinical Nursing overseeing nurses, clinical outcomes and payroll in the medical/telemetry unit and intensive care unit (ICU). The timing of her leadership role lined up perfectly with her decision to take her skills to the next level, achieving a bachelor’s degree from Nevada State College in 2016. The timing of her degree lined up perfectly with what was about to come; she embarked on her first leadership role at Renown This is where she would happily stay for 11 years, eventually becoming the Manager of Nursing in telemetry and the ICU, noting that Renown South Meadows felt like a second home to her. “I wore many hats at South Meadows,” Poeth recalls. “From piloting back coding and handling compliance work to being on the patient floor and heading up South Meadows’ first high school hospital volunteer program, I got very involved. We had seven years without having a single nurse traveler in our unit." It wasn’t long before Poeth was inspired to expand her education even further, and she graduated in January 2018 with a master’s degree in nursing clinical leadership from Western Governors University. Thanks to Renown’s educational assistance programs, our health system invested directly in Poeth’s education with tuition reimbursement and a $1,000 nursing scholarship. Soon after celebrating her achievement, Jennifer Allen Fleiner – who was the Director of Nursing at Renown South Meadows at the time – asked Poeth yet another question that would bring her to the precipice of another career detour: “Have you ever considered transferring from South Meadows to Renown Regional?” Moments later, Alicia Glassco, Director of Nursing for Renown Regional, asked her the same question, noting that the hospital’s neurosurgery unit needed the leadership of someone just like Poeth. “It took me a whole week to make a decision, because this was one of the toughest decisions I’ve ever made in my life,” said Poeth. “I truly loved South Meadows. After that week, my leader told me, ‘you know what, Poeth? You’ve reached your pinnacle. You need and deserve a new challenge. Learn from this new team and teach them something. I think you have a huge opportunity for growth.” So, Poeth decided to apply for the position and shadow the neurosurgery team, where unlike her unit, the majority of the team at the time were travelers. But this was a challenge Poeth was up to – so she was accepted into the role. “At the end of the day, these patients deserved consistent care,” Poeth emphasized. “I knew I had to take this position for the patients – they were the ones who sold me on this job. They are the reason why we are all here. It was important for me to be an advocate for them.” The big hills to climb didn’t slow down Poeth; in fact, the exact opposite happened. Within her first year in the neurosurgery unit, her team onboarded 18 new graduates and replaced travelers. “We were hiring like crazy,” said Poeth. “My standing agenda at all section meetings focused on hiring and our quality metrics. I started having a relationship with our doctors. Once we created a strong doctor/nurse collaboration, our nurses started staying with us longer.” Everything on the unit was going great. Then, COVID-19 hit. “Since we had private patient rooms, our unit became the first COVID unit at Renown Regional,” Poeth recalls. “My whole staff that I had built up had to be distributed elsewhere. I started caring for COVID patients. We relied on our Infection Prevention team a lot. And at the same time, I was worried about my family in Africa.” Despite the stressful nature that the pandemic brought upon health systems everywhere, according to Poeth, she knew she had to continue on. “The neurosurgery team ended up merging with orthopedic trauma, which was very difficult,” said Poeth. “We went from 28 beds to 58 beds. The key to success here was training. Nurses are very resilient, and through training, we were able to stabilize the unit.” Noticing the opportunity for virtual demonstrations that were previously offered only in-person, Poeth spearheaded online trainings for nursing, physical therapy, mobility, head injuries and more, allowing teams across Renown to upskill in safe spaces. These programs continued throughout the pandemic, and Poeth was proud to be a figurehead through it all, helping to stabilize the unit while creating strong relationships with the entire team, many of whom followed her from Renown South Meadows to Renown Regional. Then, she gets another visitor – her Chief Nursing Executive – in her office with yet another opportunity. Have You Considered... In September 2022, Chief Nursing Executive Melodie Osborn walked into Poeth’s office with those three words that Poeth has heard for decades: “Have you considered...” “Before Melodie could even finish, I thought, ‘I have considered A LOT in my career!’” said Poeth. Melodie told Poeth that the William N. Pennington Cancer Institute was looking for a Director of Oncology Nursing, noting that this could be yet another growth opportunity for her and a chance for her to go back to her roots. “I had just celebrated my twentieth year at Renown; I knew this was going to be a decision I really had to think about,” said Poeth. “Everyone believed in me. Alicia Glassco told me, ‘Poeth, you are ready for this. Go for it.’ Once I applied for the position and started getting my updated chemotherapy certifications, I thought, ‘they are right; I got this.’” At this point in her career, Poeth had been hyper-focused on inpatient care, and this role would be her first time caring for patients in the outpatient setting. After going through the interview process, however, Poeth knew that this was where she was meant to be yet again – and colleagues she hadn’t seen in years reaffirmed that commitment. “I felt the most excited about the job when I toured the facility,” Poeth recalls. “I’ll never forget what one of the infusion nurses told me on my tour. She told me, ‘I don’t know if you remember me, but I remember you; I came from Renown South Meadows, and you were so nice to me as I was precepting as a new nurse. Your kindness was unforgettable to me.’ The fact that people like her wanted me in the unit so badly inspired me to come back.” Soon enough, Poeth became the Director of Oncology Nursing, a position she still proudly holds to this day. Once she was hired, she immediately went into deep learning mode, mastering skills such as revenue integrity, credentialing and the insurance process. She attributes Supervisor of Infusion Kaitlin Hildebrand and Director of Radiation Oncology Services Susan Cox for helping her succeed. Shortly after assuming the position, Poeth noticed yet another opportunity for cross-training within the organization to combat short staffing – training nurses from the Float Pool to care for patients in Infusion Services. “Between May and July of this year, we trained six nurses from Float Pool to do infusion therapy services, which offered so much relief to my team; I am so thankful to Rendee Perry, the Manager of Nursing in our Float Pool unit, and her team for their support,” said Poeth. “My mission in outpatient oncology is to serve the staff and patient population and create those strong relationships." Poeth's efforts to circumvent nurse burnout go beyond cross-training – as a director, she is always there for her team members no matter what, leading with kindness every step of the way. “I never miss a 7:45 a.m. huddle unless I am in a ‘cannot miss’ commitment; I want my employees to always know that I am there for them and that they are cared for both on and off the job,” Poeth emphasizes. “I want them to feel like they are valued, their families are valued and their mental health is valued; after all, without my team, we cannot care for patients. It’s important for them to know that I am here to be a security blanket and that there is always something we can do to solve a problem." Today, Poeth enjoys a full team of core Renown staff members whom patients look forward to seeing – and the high patient satisfaction scores to prove it. “Our team is so established that patients feel comfort in knowing they are always going to know exactly who they are being treated by,” said Poeth. “We will always work to maintain that consistency.” Staying True to the Mission Renown’s mission of making a genuine difference in the health and well-being of our community resonates closely with Poeth. Before she arrives at the infusion unit every day, she asks herself: What can I do to make it easier for my team to deliver care? “It takes a village to deliver the care we do,” said Poeth. “Our nurses are priceless. You can’t place a monetary value on dealing with life and death every day. This is what inspires me. It’s all about helping each other out and keeping those relationships strong.” Maintaining those relationships on the floor, according to Poeth, requires one main ingredient: work-life balance. “I want my nurses to be able to balance sending their kids to kindergarten and giving their patients their first chemotherapy treatments,” Poeth emphasizes. “I genuinely care about their lives. It’s nice when you get to know your team’s children, grandkids, spouse and hobbies. I’m grateful that Renown has given us the autonomy to foster that flexible environment within our teams. It is so rewarding to have such a strong impact on these employees.” To Poeth, it’s all about doing and then duplicating. Luckily for her team and infusion patients in northern Nevada, a new infusion center at Renown South Meadows is planned to open in the coming years as part of our commitment to expanding care. Her team is excited to grow their expertise down to south Reno – Poeth's original home hospital. “I strongly believe that as nurses, we are meant to be where we are meant to be at the time,” said Poeth. “Be kind to yourself and remember your ‘why.’ Take advantage of the opportunity you have.” To all nurses (and future nurses) out there, Poeth wants you to know that you are welcomed and valued. You are saving lives every day, and to her, that is worth everything. “Always remain focused, even throughout all the challenges. Never forget why you got into nursing. And lastly, always stay true to your own mission,” closes Poeth.
-
Staying Heart-Healthy with Genetic Screening
February is American Heart Month. While cardiac care is crucial every time of year – especially as heart disease stays the number one killer in the United States – American Heart Month serves as a great reminder to stay on top of your heart health. We spoke with Malina Ruiz, a cardiology nurse practitioner at Renown Health, on three key ways to embrace heart-healthy living and how genetic screening can help inform you of certain genetic risks that can play a role on the cardiac life stage. 1. Invest in a heart-healthy diet. Eating a diet that is rich in fruits, vegetables, whole grains and healthy fats (including monounsaturated fats such as avocados and polyunsaturated fats such as sunflower oil) is a key defense in protecting your cardiac health, according to Malina. While you are filling your plate with these nutritious foods, remember to keep an eye on your saturated and trans-fat intake, and try limiting foods that are high in those fats. “No matter what age we are, maintaining a heart-healthy diet will always be important,” said Malina. Need help finding cardiac-friendly meals? The National Heart, Lung and Blood Institute makes it easy with heart-healthy recipes and tips from experts. 2. Do an exercise audit. “Keeping an active lifestyle during our younger years is one of the most important factors that affect heart health in future years,” said Malina. Maintaining a regular exercise regimen that allows you to raise your heart rate and break a sweat can help prevent future cardiac events. A good rule of thumb is to aim for 150 minutes a week of moderate-intensity exercise, which averages out to 30 minutes a day on 5 days out of the week. It’s never too late to start a regular exercise routine! Exercise doesn’t have to be something you dread – leverage American Heart Month to find activities that you enjoy. The American Heart Association can help you discover new ways to move your body. At the end of the day, as Malina emphasizes, “any movement is better than nothing!” 3. Don't skip those check-ups. Regular preventative visits with your primary care provider can help you identify possible risk factors for heart conditions before they start actively affecting your life. “Check-ups become even more important as we age, along with being aware of the signs and symptoms of heart disease, heart attack and stroke,” added Malina. There’s no time better than the present – call our expert scheduling team today at 775-982-5000 to request a preventative check-up with your primary care provider.
Read More About Staying Heart-Healthy with Genetic Screening
-
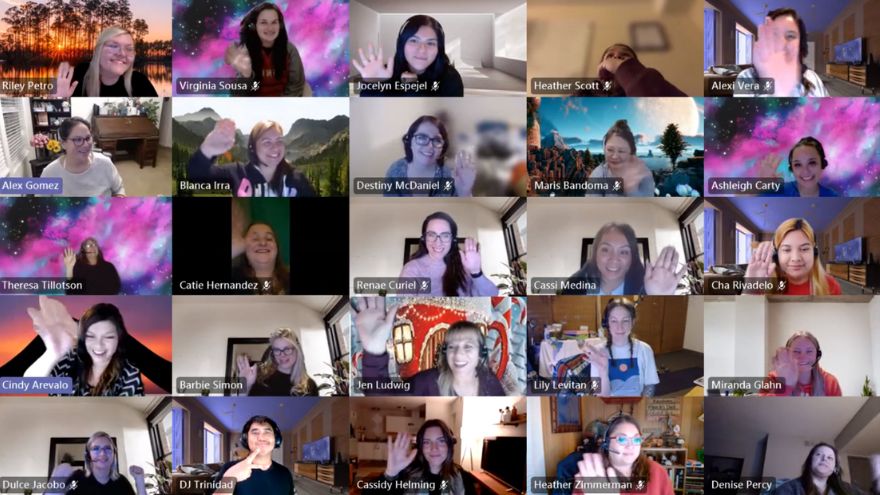
Departamento destacado: Customer Engagement Center
Do it for the patient. That’s the motto that each employee in the Customer Engagement Center (CEC) lives by every single day. This team spins all the existing stereotypical thoughts about call centers on their side by empowering and partnering with patients to achieve their best health. Being transferred around several times just isn’t in this team’s DNA – being a one-stop-shop for patient scheduling, referrals, insurance matters and more is how they proudly operate. Through elevating the customer engagement experience, the CEC closes care gaps to ensure patients get the right care at the right time. From employees who work from our home base in Reno, all the way to the southeastern corner of Florida, this primarily remote team stays firmly connected and collaborative to make patient care possible for all Renown Health patients and Hometown Health and Senior Care Plus members. The “Make It Happen” Department Back-to-back phone calls about a wide variety of patient needs? They make it happen. Referrals that need to go directly to the provider? They make it happen. Complex insurance questions that need to be resolved? They make it happen. The CEC is the keeper of all things customer service and all things patient satisfaction, leveraging technology to improve engagement and accessibility – and they wear that badge with pride. “Patient care is our first priority,” said Cindy Arevalo, Supervisor of Customer Engagement. “Even though we aren’t face-to-face with them, we are always there to help them over the phone with whatever their needs are.” The CEC has a lot of different sub-departments under its umbrella: scheduling, referrals, insurance, patient outreach, personal assistants, MyChart customer service and more. Each team handles calls for a different section of our health system, including the hospitals, imaging, primary care and specialty care. While their individual teams may be different, one aspect of their jobs remains the same: they care. Deeply. “We advocate for the patient, especially when they can’t advocate for themselves,” said Amanda Ishii, Referral Specialist. “We are the first people that patients speak to, and we all have empathy to listen to them, help them solve their problems and take as much time as they need to care for their needs,” added Susana Arroyo Garcia, Supervisor of Customer Engagement. Customer loyalty is key to the CEC. Every CEC team member builds strong relationships with patients and members. Whether they manage patient outreach or manage back-to-back inbound calls, each employee feels a special connection to the helpful work they do to solve a variety of patient concerns. “As Senior Care Plus Personal Assistants, for instance, we help guide our members through complex situations, and we eliminate the process of transferring them to different departments, becoming a ‘one-stop-shop' for them,” said Stephanie Perez Campbell, Senior Care Plus (SCP) Health Coordinator. “While every day is different, we are constantly learning new things and helping members navigate through the health system." With the 4.5 million calls the CEC handles per year, the nature of their jobs is undoubtedly fast paced. However, this does not intimidate the CEC team members; instead, it inspires them to continue reaching new milestones, helping thousands of patients and members every year by handling all the scheduling and referral work on the backend so that they can receive the care needed. “I never find myself sitting around asking, ‘what should I do next,’” said Gina Briles, Supervisor of Customer Engagement. “We always support each other to stay on top of it all in order to take care of our patients.” By wearing a lot of hats and managing many different work queues all while staying engaged with each patient, the CEC is full of natural problem-solvers, helping our healthcare network run smoothly. “The Engagement Center is the front door for the community; serving as the voice of the customer, we ensure patients do not fall through the cracks of the complex healthcare system and are able to easily access the right care at the right time through an exceptional experience,” said Candace Dietrich, Director of Customer Engagement. Consistently Connected With thousands of referrals to process and millions of calls to field, the ways the CEC stays connected to patients and members as well as each other can be related closely to magic. No concern goes unnoticed, and no problem is too complicated. “The sheer volume of patients we engage with is incredible,” said Rene Jacinto, Manager of Customer Engagement. “We processed nearly 200,000 referrals and authorizations last year.” “We expect a steady increase of calls year-over-year. My team processed 1,259 referrals in one day alone recently,” added Arielle Gomes, Referral Specialist. A superpower that every CEC team member holds is the ability to listen. According to this department, active listening is key when problem-solving with every patient and member, as that skill helps them anticipate patient needs and resolve their issues quickly and efficiently. “I’ll always listen,” said Alex Gomez, Customer Engagement Representative. “I want them to know that they are in good hands, especially when they are feeling scared or frustrated.” Team members like Alex help carefully guide customers through the Hometown Health and Senior Care Plus enrollment process, increasing membership and engaging patients to find the perfect plan for them. One of the largest challenges the CEC faces is the departures and arrivals of providers. The ebbs and flows of all hospital systems include provider departures and shifting provider availabilities. Despite this challenge, the CEC staff work hard to ensure communication with all patients regarding provider changes is consistent and that all patients are scheduled in a slot that works for both their schedule and the provider’s schedule. “It’s important for us to be flexible, because things can change at a moment’s notice,” said Gina Briles. “This is more than just a job – we are here for our patients. What we are doing impacts everyone.” Throughout all times of transition, the CEC builds robust relationships with both patients and providers within our organization and community, a skill that this team emphasizes as “fundamentally important.” For example, SCP Personal Assistants like Stephanie Perez Campbell will coordinate care with community resources and offices, giving members one less call to make and one less hurdle to cross in order to get the care they need. On top of it all, even though this team has the ability to work from all 50 states (and many of them work outside of Nevada!), every employee feels connected to their colleagues and their work. “This is the best group of people I’ve ever worked with,” said Riley Petro, Manager of Customer Engagement – Imaging. “I am super lucky for this job and am so thankful for these people.” Proud and Powerful The proof is in the pudding – or rather, the proof is in the numbers. Within the 4.5 million calls they successfully field every year, approximately 1.6 million of those calls route through the private branch exchange (PBX) team – the team that oversees the main operator lines – under the guidance of Jess Nater, Supervisor of Customer Engagement. The CEC is also on track to handle nearly 300,000 referrals this year alone. Additionally, the Hometown Health CEC team was recognized nationally this year with a five-star rating from Medicare. “We all have the initiative to grow, and because of this, we are always learning something new,” said Cindy Arevalo. “Our leaders also support our growth, especially if we want to skill-build or advance in our careers.” The CEC is frequently the first stop on the career ladder for many employees as they start their journey in healthcare, and CEC leadership is committed to the growth and development of their teams to reach their career goals at Renown. The secret formula for all this success can be in part attributed to the pride each CEC employee has for their team, their work and Renown. “We have a very supportive team,” said Holly Coffey, Supervisor of Customer Engagement. “I’ve seen our leaders support their teams tremendously.” “We rely on each other,” added Ashleigh Carty, Customer Engagement Representative. "I love the relationships we create with one another.” Employees in the CEC come from many walks of life, choosing to work at Renown and Hometown Health for a variety of different reasons, many related to the positive power our health system holds. Team members in this department hold a myriad of different career backgrounds, including pharmacy technicians, medical assistants, population health professionals, community health workers and more. Some team members, like Nikki Clifford, Customer Engagement Representative Lead, heard wonderful things about Renown from her mother, who also works for Renown. According to Nikki, “seeing how happy my mom has been in her career made me want to join too. I’ve loved it here ever since.” Katie Lunau, Supervisor of Customer Engagement, also grew up in a family involved in healthcare, and she wanted to follow in their footsteps. Choosing Renown as the place to follow her family path was a simple one, because “Renown stood out as the company that was actively involved in the community helping others.” For other team members, like Susana Arroyo Garcia, Ashleigh Carty and Stephanie Perez Campbell, Renown and Hometown Health’s impact on the local healthcare landscape was their primary driver for choosing a career here and in the CEC specifically. “Renown is very well-known in the area,” said Stephanie Perez Campbell. “I went to school in Reno for public health, so Renown came up all the time in my schooling. I knew Renown had a lot of different opportunities available for career growth, and with the friendly environment I always experienced here, it was an easy decision.” “Once I went through the interview process and joined the team, I immediately realized that there are outstanding managers, support systems and communication skills here. People genuinely care,” added Ashleigh Carty. Ashleigh is exactly right. As emphasized by every team member, employees in the CEC care. Their heightened levels of care and empathy set the bar high for all at Renown and Hometown Health, and their impact will be felt for years to come.
Read More About Department Spotlight: Customer Engagement Center
-
7 Important Vasectomy Questions for Your Doctor
If you and your partner are looking for a more permanent birth control method, you might consider a vasectomy. Although vasectomies are common, knowledge about them isn’t quite as common or talked about. If you are considering a vasectomy, talking with your primary care doctor is a great way to learn more and start the process. We consulted with Dr. Aurosis Reddy a primary care doctor with Renown Health – South Carson, about key topics to discuss with your doctor when considering a vasectomy. What is a vasectomy? A vasectomy – also called male sterilization – is a form of male birth control that blocks sperm from reaching semen, according to the American Urological Association (AUA). How effective and safe are vasectomies? Vasectomies are one of the most effective methods of birth control with a long-term success rate of over 99%. A vasectomy has been a safe and successful birth control method for many years. More than 500,000 men elect to have vasectomies every year in the U.S., and the number is rising. A vasectomy is also generally a low-risk procedure with a low complication rate ranging between 1-2%. What does the recovery period look like? A vasectomy is typically a quick procedure that takes under thirty minutes and can be performed in an outpatient setting under local anesthesia. Recovery from a vasectomy is also considered relatively easy. After a vasectomy, most can: Resume everyday activities within two to three days Resume normal exercise in one week Start engaging in sexual activity again in one week Your doctor can provide more details on what your individualized recovery process will look like.
Read More About 7 Important Vasectomy Questions for Your Doctor
-
Meet Gabby, Renown Regional ER Nurse and Miss Rodeo Nevada
Renown Health is proud to embrace the Reno-Sparks culture that makes our community stand out, which is why we sponsor the Reno Rodeo, an early summer staple with roots in the community as deep as our own. One of our many ties with the Reno Rodeo includes Renown Regional’s own emergency room nurse and Miss Rodeo Nevada 2022, Gabby Szachara. A Reno native, Gabby developed a love for the Reno Rodeo at a very young age. “I loved watching the girls on the Reno Rodeo Flag Team when I was little and knew I wanted to be part of the Reno Rodeo someday,” said Gabby. “As I got older, I started to make connections and build relationships with some people in the rodeo scene, and they generously lent me their horses so I could participate in the Reno Rodeo Flag Team.” Gabby was on the flag team for three years before being crowned Miss Rodeo Nevada 2022 last year. Before joining the Reno Rodeo Flag Team, Gabby was a student at the University of Nevada, Reno, and a member of the women’s volleyball team. In December 2017, she graduated with a bachelor’s degree in public health. At first, Gabby was interested in a career in sports medicine – it made sense with her background in athletics. But, after working in the medical field as a certified nurse assistant and an emergency medical technician, she grew passionate about patient care and decided she wanted to become a nurse. “I’ve always loved teamwork and helping others,” said Gabby. “It’s important to me to be there for others, especially when it might be their worst day.” In December 2021, Gabby graduated from Truckee Meadows Community College with a nursing degree and joined Renown Health this February. “I love Renown for various reasons. Everyone here is so nice and welcoming, and there is a great team dynamic,” said Gabby. “And I love that Renown’s main color is purple because that is my favorite!” When Gabby isn’t in her scrubs and caring for patients, she is in western wear and carrying out her duties as Miss Rodeo Nevada. “I do a lot of traveling across the country to attend other rodeos,” said Gabby. “I enjoy meeting so many wonderful people and experiencing the culture of different states.” Gabby’s main goals as Miss Rodeo Nevada are to promote the western way of life, agriculture, rodeo and community benefit. In addition, she visits local schools to talk with kids about how they can get involved in these areas and inspires them to turn their dreams into reality. Gabby has a special place in her heart for the Reno Rodeo. “Reno is my home, and the Reno Rodeo is the heart and soul of summer in northern Nevada. Everyone comes together and dusts off their boots to have fun and also contribute money to important causes in our community,” said Gabby. “I love the comradery, the friendly and healthy competition and the great people.” If you’re going to the Reno Rodeo this weekend, watch for Gabby and her horse, “Torque.” And if you see Gabby in the halls at Renown Regional, give her a high-five for all her hard work as a nurse and Miss Rodeo Nevada!
Read More About Meet Gabby, Renown Regional ER Nurse and Miss Rodeo Nevada
-
La historia de Paola: incorporar la esperanza y la determinación en el cuidado del paciente
You may recognize her from billboards around town or the cover of Renown's latest annual report, but what you might not know is the story behind the now-familiar face. Paola Espinoza-Patino is the oncology unit's associate nurse manager at Renown Regional, and she grounds her work in hope and determination daily. Meet Paola:
Read More About Paola’s Story: Bringing Hope and Determination to Patient Care
-
Enfermedad hepática no alcohólica y genética: ¿Existe alguna relación?
What exactly is the relationship between genetics and disease? Powered by Renown Health, the Healthy Nevada Project is one of the most visible genomic studies in the United States. They are recruiting participants here in northern Nevada to understand the relationship between genetics and nonalcoholic liver disease. Joseph Grzymski, Principal Investigator at the Healthy Nevada Project and Chief Scientific Officer at Renown Health, shares why this study is so important and who should take part. Many people are aware that heavy drinking can lead to liver disease. Yet they are unaware that other types of liver disease are not caused by alcohol consumption. These types of liver disease are more difficult to diagnose but are equally dangerous. What is NASH? A build-up of fat causes nonalcoholic Fatty Liver Disease (NAFLD) in the liver. The most dangerous form is called Nonalcoholic Steatohepatitis (NASH). It causes inflammation and damages liver cells, leading to fibrosis, scarring of the liver, and decreased liver function. If NASH goes untreated, irreversible liver damage can occur, leading to cirrhosis, cancer, or liver failure. These conditions can be fatal. What’s most concerning about NASH is that the symptoms don’t typically cause pain and aren’t noticeable. The good news is that a new local study is raising awareness about this disease by recruiting at-risk people for NASH. Am I at risk for developing NASH? The following factors put you at risk: Obesity Type 2 diabetes Metabolic syndrome High blood lipids, such as cholesterol and triglycerides Does having a family member with nonalcoholic liver disease increase my risk? We do not know a lot about inheriting NASH, although a lot risk factors run in families. One goal of this study is to better understand the genetic component of NASH. There are certainly other risks too, such as environmental and behavioral risk factors. However, we don’t yet have a good grasp on how these impact NASH risk. How is NASH diagnosed? Diagnosis is traditionally done with either a liver ultrasound or biopsy. However, both procedures are expensive and the invasive biopsy has risks. Therefore doctors often use risk factors or less invasive blood tests for diagnosis. This NASH study will include a new blood test called the enhanced liver function (ELF) test. Doctors and researchers have data suggesting that the ELF test is a better diagnostic test for NASH risk. Conducting this cutting-edge test with study participants allows them to share results with their doctors to ensure the best care. What can I do to reduce my NASH risk? Limiting exposure to the risk factors of NASH often lowers risk. Eating a healthy diet, maintaining a recommended weight and exercising regularly can proactively lower your risk.
Read More About Nonalcoholic Liver Disease and Genetics: Is There a Link?
-
¿Qué es el Healthy Nevada Project?
The Healthy Nevada Project (HNP) is one of the most visible genomic studies in the United States, and guess what? Renown Health powers it! The Healthy Nevada Project (HNP) aligns with Renown's goal to do the best for our patients. The genomic study is at no-cost for Nevadans and gives participants insight into different genetic traits, including results on three prevalent and serious health conditions known as CDC Tier 1 conditions. CDC Tier 1 Conditions Include: Hereditary Breast and Ovarian Cancer Syndrome (HBOC) Lynch Syndrome Familial Hypercholesterolemia (FH) Not only does HNP give participants insights into their genetic background, but it also facilitates Renown's ability to study population health. Research lays the foundation for the future of medicine, and Renown's HNP is on the cutting edge of genetic research. We do this by providing skilled researchers access to studies for the diseases that currently have limited treatment, including nonalcoholic steatohepatitis liver disease or NASH. For example, the observational NASH study helps researchers understand genetic links to the disease. Make an Appointment to Get Screened If you haven't already, join the over 55,000 HNP participants and make an appointment to have yourself screened. You can schedule a screening appointment through MyChart. Click “Schedule an Appointment" and select Research Appointment - Genetic Screening. Prior to your appointment, please complete e-Check-in and complete your consent form.