Buscar
-
8 pruebas de evaluación de la salud importantes para hombres
Men are generally less likely to visit their doctor for exams, screenings, and consults compared to women. To address this, we've collaborated with Dr. Bonnie Ferrara of Renown Health, to compile a list of eight essential screenings that can help men maintain their health. 1. Blood Pressure Tests Ages 20+ Blood Pressure tests measure the pressure in your arteries as your heart pumps. Biennial (every two years) checks are recommended if you have normal blood pressure or more frequently if you have high blood pressure (hypertension) or low blood pressure (hypotension). The United States Preventative Services Taskforce cites normal blood pressure below 120 systolic (top number) and 80 diastolic (bottom number). 2. Cholesterol Screening Ages 20+ High levels of cholesterol increase your risk of stroke and heart disease. A simple blood test will help your healthcare provider determine your numbers and if you're at risk. If you have a family history of diabetes or heart disease, you may need yearly screenings. But, again, your doctor can provide the best course of action.
-
How to Spot Depression in Men
Is a man in your life struggling with depression? Many men find it difficult to acknowledge when they need help. Recognize their unique warning signs of depression with insights from psychologist Dr. Herbert Coard. Over 6 million men are diagnosed annually, often displaying symptoms like anger and aggression instead of sadness. Learn how to support them and understand these often-misinterpreted indicators. Behavioral Signs of Depression in Men High levels of the hormone cortisol are released during stressful situations affecting the neurotransmitter, serotonin (a feel-good hormone), contributing to depression. You can identify depression or suicidal tendencies by paying close attention to the following behavioral changes: Anger, irritability, or aggression Avoiding family or social situations Losing interest in family responsibilities, passions and hobbies Lack of sex drive Becoming controlling/abusive in relationships Risk-taking behavior such as; unsafe sex, overspending or gambling Not being able to concentrate or remember details Excessive drinking or drug use Having frequent thoughts about death Talking about suicide Attempting suicide Factors That Lead to Depression in Men Life Events Work stress or long-term unemployment can be huge contributing factors relating to depression. This type of life event can be overwhelming, making it impossible for a man to cope. Changes in Relationships The loss of a relationship can be a significant contributing factor to the emergence of depressive symptoms and past experienced physical, sexual, or emotionally abusive relationships. With this in mind, counseling can often help individual to overcome this type of trauma. Grief and Loss Overwhelming sadness due to the loss of a loved one can trigger depression. Although normal, each person goes through their own grieving period. For example, normal responses to death are insomnia, poor appetite and loss of interest in activities. Pay attention if grief seems prolonged or out of the ordinary. Health Problems In particular, depression coexists with medical conditions. As men age, this can be passed off as normal aging, but it could be more serious. In addition, illnesses such as thyroid disorders, Addison’s disease and liver disease can cause depressive symptoms. Diabetes, cancer, heart disease, or Parkinson’s disease can affect any age, thus triggering or worsening depression. Some older men also feel like they may be suffering from dementia because of difficulties with memory this may be a symptom of depression. A trip to the doctor may be in order to help alleviate concern and worry. Depression in Men and Suicide Frequently the emotional pain occurring with depression can distort a man’s ability to see a solution beyond suicide. Individuals with depression become very rigid and constricted in the way they solve problems. The statistics below speak for themselves, helping us understand the need to reach out to those who need our support. Male suicide rates are on rising – men die by suicide 3.53 times more often than women, accounting for 70% of all suicides. Sadly, every day 129 men commit suicide. White males accounted for 69.67% of suicide deaths in 2017. In 2017, firearms accounted for 50.57% of all suicide deaths. Middle aged Men who are middle aged have the highest suicide rates. 40% of those identifying as transgender have attempted suicide in their lifetime. Males who are guy or transgendered are at an increased risk for suicide attempts, especially before age 25. Veterans often suffer from post-traumatic stress disorder (PTSD) and depression, and are more likely to act on a suicide plan. How You Can Help Now that you can identify some of the warning signs of depression, here’s how you can help: Talk about your concern and communicate that you’re there to help him. Let him know depression is a medical condition and will usually get better with treatment. Suggest professional help from a Primary Care Provider, Psychologist or Therapist. Help set up appointments and offer to accompany him – let him make the decision, but make it clear you’re there for him, no matter what he decides. If you feel he is in a dire or life-threatening situation, contact 911. Call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to talk to a trained counselor. Call the Veteran’s Crisis Line at 1-800-273-TALK (1-800-273-8255) and press “1”
-
When Should You Consider Hospice? 5 Important Signs
Deciding on hospice care for a loved one is a deeply personal and challenging decision, balancing their wishes and medical realities. Rebecca Edwards, DNP, from Renown Hospice Care, explains the signs indicating when it might be time for hospice and offers guidance on navigating this decision with compassion and clarity. Understanding Hospice Care Before exploring the decision-making process, it’s crucial to have a clear understanding of what hospice means. Hospice care represents a shift in how we approach living with a terminal condition, emphasizing comfort, dignity, and quality of life above all else. When there is no longer a pathway to a cure, side effects of treatment outweigh the benefits, or someone is simply tired of frequent hospital visits, then it may be time for hospice. Hospice care is mainly done in the home, where most people wish to be. It's a compassionate, team approach to care that focuses on meeting the physical, emotional, and spiritual needs, supporting their families, and honoring individual preferences. 5 Critical Signs to Be Aware Of Decline in Overall Health: When a loved one's health continues to decline despite ongoing medical interventions, this may be a sign that these treatments are no longer effective. Increasing Pain and Symptoms: When managing symptoms such as pain, nausea, fatigue or shortness of breath becomes increasingly challenging, hospice can offer specialized support and expertise in symptom management. Frequent Hospitalizations: Repeated hospitalizations or emergency room visits can signify that the disease has progressed to a point where managing symptoms and providing comfort at home or in a hospice setting is a more appropriate approach. Difficulty with Daily Activities: If your loved one is experiencing difficult with activity of daily living such as dressing, bathing, or mobility, it may be a sign that they require additional support and assistance. Prognosis of Six to 12 Months: Hospice Care is typically recommended for patients with a prognosis of about one year or less if the disease follows its normal course. However, it’s important to remember that every individual is unique and prognosis can vary.
Read More About When Should You Consider Hospice? 5 Important Signs
-
Motivar a los niños a comer alimentos saludables
Do you have a picky eater in your household? Or maybe you've got a snack monster who’s all about chips and candy? We're here to share a few fun strategies to motivate your little superheroes to snack on healthy foods instead! Rainbow Power-Up Eating a rainbow isn't just for unicorns! Different colors mean different powers: Red foods like strawberries and tomatoes help your heart. Orange foods like carrots and sweet potatoes help your eyes spot things like an eagle! Green foods like spinach and broccoli help you grow super strong bones. So, create a plate with as many colors as possible. The more colors, the more powers! Super Smoothies Blend your favorite fruits, such as bananas, berries and mangoes. Add some milk or yogurt and a handful of spinach. Your kids won't taste the spinach, and they'll drink a supercharged smoothie that gives them the energy to tackle any challenge. Create a Parfait Packed with Delicious Layers! Veggie Villans Who said veggies can't be fun? Turn them into heroes by giving them cool names and fun shapes. Make carrot sticks "Captain Crunch" or broccoli florets "Broc the Rock." Dip them in hummus or peanut butter for an extra flavor kick. Snack Attack Plates Create snack plates that are as fun as they are nutritious. Combine: Cheese cubes Grapes or apple slices Nuts or seeds Whole-grain crackers Mix and match these for your perfect plate! Make Your Own Trail Mix Fuel-Up Challenges Challenge your kids to eat three different healthy foods each day. Turn it into a family game to see who can eat the most colors or try the most fruits and veggies. You can even draw up a "super snacks" chart to keep track of your progress. Final Super Tip! Even superheroes have cheat days. Don't worry if your family doesn't eat healthy every meal. Just aim to eat more of the good stuff than the not-so-great stuff. Your kid's bodies will reward them with tremendous energy, focus and strength.
-
Make Your Own Trail Mix: 4 Quick and Easy Recipes
Craving a crunchy, sweet, and nutritious snack? Try making your own trail mix! Perfect blends of nuts, dried fruits, and a touch of chocolate can be whipped up using bulk bin ingredients or pantry staples. Enjoy this delicious, healthy snack on a hike, at the office, or on your next road trip through Nevada's scenic deserts.
Read More About Make Your Own Trail Mix: 4 Quick and Easy Recipes
-
Nourishing Your Loved One Through Cancer Treatment
Eating healthy is a daily challenge for many, but for those with cancer, it is an even harder struggle. A cancer diagnosis affects not only those diagnosed but family members and friends, too. One key area of concern is making sure your loved one stays well by eating healthy food every day. Here are some vital cancer nutrition tips from Jessica Blauenstein, a Board Certified Specialist in Oncology Nutrition and Registered Dietitian at Renown Health. Help to Prepare Meals and Snacks for Daily Cancer Nutrition Make it grab and go. Easy-to-make meals help reduce the burden of having to cook and prepare food. Having easy to grab snacks on the counter or in the fridge can help ensure your loved one has access to those nutrients when needed. Sit outside of the kitchen. This allows your loved one to avoid cooking smells which can make them feel sick as a side effect of cancer treatments. Also try serving them cold foods such as sandwiches, cheese and crackers, or shakes which have a mild scent. Try drinkable meals. Some people with cancer find it easier to sip their calories over the course of 30 minutes to an hour. Consider smoothies or supplemental shakes such as Ensure Complete, Fairlife shakes, Orgain shakes, or Boost Plus to name a few. A great foundation for a smoothie is a protein source (Greek yogurt, protein powder, nut butters or milk) with a carbohydrate (fruits, juice or berries). Add other ingredients as desired, such as spinach, kale, and ground flaxseed or chia seeds to give it more vitamins, minerals, and fiber. Snack Ideas for Those Undergoing Cancer Treatment The following ideas are both quick and easy to make for your loved one. Chicken or tuna salad with whole grain crackers or as a sandwich on whole grain bread Greek yogurt mixed with cereal, fruit and/or nuts Cottage cheese with banana, cinnamon and/or peanut butter Favorite fruit with 100% natural peanut or almond butter spread - Try peanut butter with bananas, apples, or even celery Their favorite veggies dipped in a salad dressing of your choice - For example, carrots with hummus, tahini, or ranch dressing Cheese and whole grain crackers - Add tomato slices with a small amount of avocado, and a dash of oregano on top for more flavor Eggs scrambled with cheese, vegetables and/or salsa Peanut butter and jelly sandwich on whole grain bread A baked sweet potato with some favorite toppings Hard boiled eggs and/or egg salad with whole grain crackers, or as a sandwich on whole grain bread Oatmeal or cream of wheat prepared with milk, fruit and/or nuts Sometimes your loved one may not feel like eating or refuse to eat. If treatment side effects are impacting your loved one’s ability to eat, please visit the websites below containing recipes tailored to treat side effects. Cook for Your Life ELLICSR Of course, you may also consult a registered dietitian and/or the patients care team, if you have more cancer nutrition concerns.
Read More About Nourishing Your Loved One Through Cancer Treatment
-
Departamento destacado: Farmacia
When it comes to each patient’s healthcare journey, medication is often a key chapter. After all, medication is one of the most common treatment methods to help patients on the road back to health. In 2023, 4.83 billion prescriptions were filled in the U.S., and with this number only anticipated to rise annually, having an expert pharmacy team on your side to make certain you are prescribed the ideal dosage to treat your condition, prepare your prescriptions on time and help you manage your medications responsibly is important. Fortunately, at Renown Health, we have best-in-class inpatient and outpatient pharmacy teams to fill both prescriptions and promises for excellent care. Renown Pharmacy plays a vital role in helping us foster a health system that prioritizes patient well-being above all else. This department exemplifies the impact that a unified, expert pharmacy team can have on patient outcomes now and in the future. The Masters of Medication Spanning three hospitals plus ambulatory locations across the health system, Renown’s growing pharmacy team – full of dedicated pharmacists, pharmacy technicians and even medical assistants – manages medications in a wide variety of patient settings, touching nearly every aspect of the healthcare continuum: Outpatient Retail Pharmacies Renown Regional Medical Center – 75 Pringle Way The Healthcare Center – 21 Locust Street Renown South Meadows Medical Center – 10101 Double R Blvd Inpatient Pharmacies Renown Rehabilitation Hospital Renown Regional Medical Center (including Renown Children’s Hospital) Renown South Meadows Medical Center COMING SOON: Conrad Breast Center Pharmacy (in honor of Kristina Ferrari) in the Specialty Care Center at Renown South Meadows Ambulatory Pharmacies Anticoagulation Services – Institute for Heart & Vascular Health (IHVH) Pharmacotherapy Program – IHVH and Renown Medical Group Locations Congestive Heart Failure Pharmacotherapy Program – Center for Advanced Medicine B at Renown Regional Chronic Obstructive Pulmonary Disease (COPD) Pharmacotherapy Program – Renown South Meadows Endocrinology Pharmacotherapy Program – Renown South Meadows Additional Pharmacy Programs Medical Reconciliation Pharmacy Residency Clinical pharmacists at Renown bridge the gap between medicine and compassionate support, making sure each patient receives personalized care one prescription at a time. “There are various roles pharmacists play within Renown,” said Clarissa Munoz, Clinical Pharmacist in the Renown Regional Inpatient Pharmacy. “Staff pharmacists work diligently to ensure correct medications are dispensed, and if compounded, make sure they were prepared properly. They also work hard to answer medication messages and phone calls, help verify orders and make sure ode trays/RSI kits are appropriately stocked and ready when needed. Clinical pharmacists work from satellite pharmacies on the floor and focus on reviewing patient charts and aim to provide additional interventions to the providers to optimize treatment strategies. We also serve as a resource for nursing staff and help answer medication questions.” “My role in the pharmacy is pretty expansive,” added Chanelle Ajimura, Clinical Pharmacist in the Renown Regional Outpatient Pharmacy. “I maintain inventory to confirm patients can receive their medications in a timely manner both for our discharge and retail patients while balancing the Meds to Beds program, which offers medication delivery to the bedside and bedside medication counseling; collaborating with an interdisciplinary team to find the most affordable price for patients; and verifying that the dose, strength, indication, etc. is appropriate for the patient from start to finish.” “In the pharmacy, I make sure patients are receiving appropriate drug therapy by checking for major drug interactions and ensuring appropriate dosing,” added Courtney Church, Clinical Pharmacist in the Renown Regional Outpatient Pharmacy. “I also make recommendations to providers so patients can get cost-effective therapy.” Our pharmacy technicians work behind-the-scenes ensuring efficient medication management, making a difference in the lives of patients every day. “A pharmacy technician is responsible for making sure the patient gets their medications on time and at the lowest price possible,” said Nate Graham, Pharmacy Technician in the Renown Regional Outpatient Pharmacy. “This is done by working with patients, insurance companies and case workers. We fill prescriptions, enter prescriptions into our system, receive and send orders for medications and maintain a clean pharmacy with an accurate inventory.” “We do a variety of things; the task people probably know the most is counting out the medications and putting them in the amber vials,” added Rachel Vallin, Pharmacy Technician in the Renown Regional Outpatient Pharmacy. “We also help patients at the front of the pharmacy, ring out their prescriptions, answer some basic questions (deferring to a pharmacist as necessary) and billing insurance. Meds to Beds is my favorite part because I feel the most involved. I take medications to patients who are discharging up to their hospital rooms so they have it with them when they leave.” “As a technician, I confirm that all medications of new admissions are available in our machines prior to admitting and then maintain stock during each patient’s stay,” added Tammara Axtman, Pharmacy Technician at Renown Rehabilitation Hospital. "I also assist our nurses when needed in regard to any of their questions with both EPIC and Omnicell.” Our pharmacy team is also on the move all across our health system, thanks to our Ambulatory Pharmacy programs. For patients experiencing a serious heart, lung, or endocrine condition that requires ongoing drug therapy maintenance and guidance, our ambulatory pharmacies step in to carefully monitor how their medications impact their health and well-being. “Our role as pharmacists in this department is non-traditional because we actually see patients in the exam rooms face-to-face,” said Cory Lankford, Ambulatory Care Clinical Pharmacist for Renown’s Anticoagulation Services. “We modify their medication regimens and drug recommendations under collaborative practice agreements.” “Because our role is so unique, we have a lot of opportunities to make a positive impact on patients,” added Janeen Abe, Ambulatory Care Clinical Pharmacist for Renown’s Anticoagulation Services. “We do a lot of direct patient interaction, including counseling patients on their medications and helping them navigate through their disease state.” “As a medical assistant in this department, we’re called the patient ‘liaisons’ to orchestrate who they should go to whether it’s a nurse, a provider or a pharmacist,” added Kiara Scruggs, Medical Assistant for Renown’s Anticoagulation Services. “We look at each patient’s medications and help with the Warfarin blood thinner monitor. We get to do a lot with patients." A key resource within the Pharmacy department and the emergency admission process, our Medical Reconciliation ("Med Rec") team stays on top of each patient's medication records. By ensuring each medication regimen is accurately reflected in each patient's chart and that patients continue to take their at-home medications while admitted to the hospital, this team provides vital insight into medications that could be a contributing factor to each patient's symptoms, including drug interactions. “Our medication reconciliation pharmacy technician team are true detectives,” said Heather Townsend, Clinical Pharmacy Supervisor. “When a patient arrives to the hospital, Med Rec works with patients, families, caregivers and outpatient pharmacies to compile a list of medications the patient has been taking a home. This list is used to make sure medications are not contributing to the patient’s symptoms and to assure medications are continued throughout the hospital stay. The addition of the medication reconciliation team has been one of the greatest advancements in medication safety.” “As a Med Rec Tech, we interview patients and family members and call pharmacies, skilled nursing facilities, etc. to obtain an accurate and complete medication list/history to outline what the patient is currently taking on a daily basis,” added Kara McGee, Medical Reconciliation Pharmacy Technician. “We make sure that we document the correct medication, dose, route, frequency and directions. This information is crucial because the nurses, pharmacists and physicians look at our work to figure out if any medications are contributing to the patient's health condition, and for the continuation of home medications on admission.” “Even though the Med Rec Tech might seem small in the hospital realm, it is very vital for patient information and beneficial to the patient's health,” added Brizza Villafan, Medical Reconciliation Pharmacy Technician. “There is never a dull moment in this work.” No matter the diagnosis, having Renown Pharmacy as an integral part of your healthcare team is a win-win situation for both you and them: you receive access to medication to help you heal, delivered to you with precision and care, and the pharmacy team has the opportunity to care for you and make a positive impact, a role they take seriously.
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
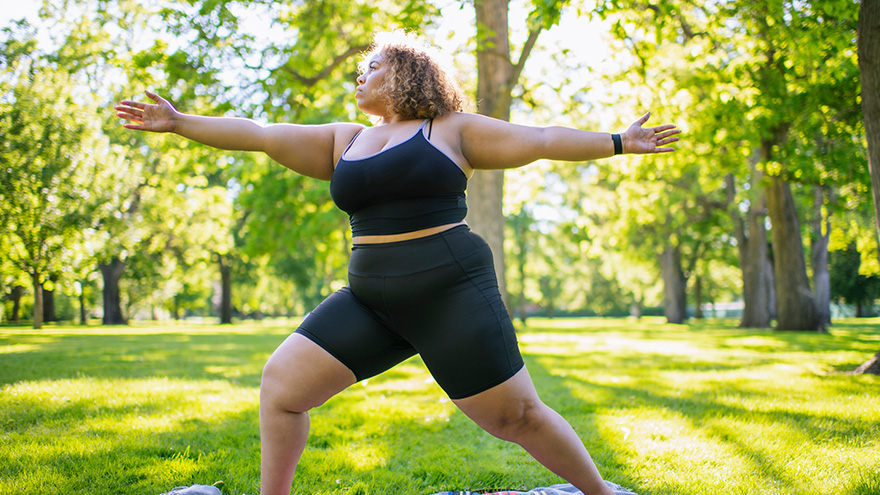
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Celebrating Blood Sugar Balance This Holiday Season
As the holiday season draws near, we find more reasons to celebrate with loved ones. At Renown Health, we are kicking off the celebrations early this November with American Diabetes Month. Approximately 37 million Americans, including 270,000 Nevadans, have been diagnosed with diabetes with as many as 95% of those diagnosed living with type 2 diabetes mellitus (T2DM). What is Type 2 Diabetes? Type 2 diabetes is a chronic health condition that occurs because your body is not using insulin (a hormone made by the pancreas to help cells use the food we eat for energy) as well as it should, resulting in high blood sugar levels. It is important to obtain a diagnosis for T2DM and ensure it is well-controlled to prevent serious health complications. Those with diabetes are at higher risk for blindness, kidney failure, heart disease, stroke and amputation. Tips for Supporting Your Health with Type 2 Diabetes Know Your Blood Sugar Levels: Work with your healthcare provider to establish target blood sugar levels, and make sure to monitor your levels regularly as advised by your healthcare provider to prevent or delay health complications associated with T2DM. Focus on Your Plate: Eating foods such as fruits and vegetables, lean meats or plant-based proteins, healthy fats and whole grains supports diabetes management. If choosing healthy foods is difficult due to your busy schedule, cost or simply because you aren’t sure where to start, talk with your healthcare provider who may refer you to a registered dietitian. Registered dietitian nutritionists are certified nutrition specialists who can provide education and practical tips for eating to support your T2DM diagnosis with visits covered by many insurance plans. Prioritize Staying Active: Engaging in regular exercise is good for everyone, especially those living with T2DM. Exercise helps your cells become more sensitive to insulin and therefore supports healthy blood sugar levels. Always check with your healthcare provider prior to beginning a new exercise plan. Support Stress Reduction: Stress is unavoidable but can be managed through regular exercise, getting enough quality sleep (7-8 uninterrupted hours per night) and practicing meditation and other mindfulness techniques. Plan Ahead for Holiday Gatherings: There’s still room for celebration while focusing on blood sugar management. Consider bringing a healthy dish to your gathering, focus on filling your plate with vegetable sides and eating those first and incorporate a family walk after dinner. If traveling, pack nutritious snacks that support your health and keep you full. Lastly, enjoy the special dishes and desserts this season has to offer in single-serving portions.
Read More About Celebrating Blood Sugar Balance This Holiday Season
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know