Buscar
Resultados para “enfermeros”
Borrar-
Departamento destacado: Trabajo de parto y parto
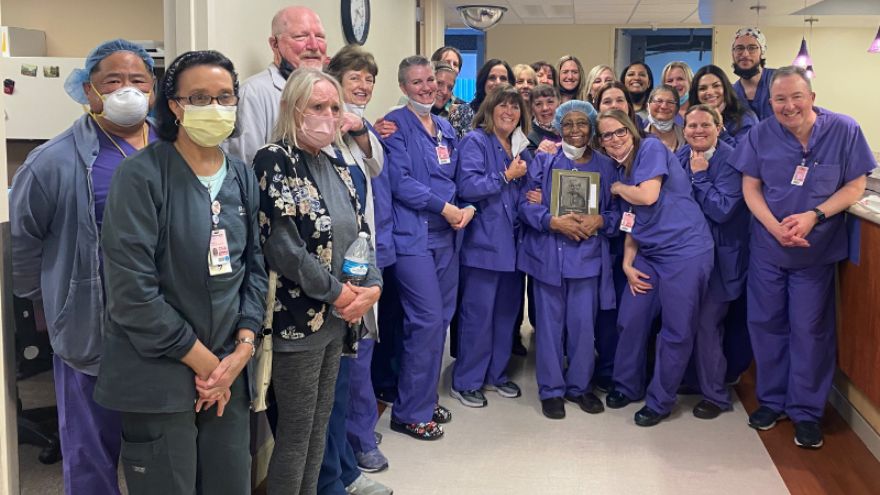
Parents welcoming their new bundles of joy into the world might be overcome with emotions. They're exhausted yet excited to meet their new baby and hold them in their arms. That’s where Renown Health’s Labor & Delivery (L&D) department comes in. When patients arrive at the L&D unit in Renown Regional Medical Center, they are embraced with caring, compassionate nurses, surgical technicians and physicians ready to serve their family. As they get ready for the big moment in their private L&D room or family suite, you can be certain that you, they can be certain that they will receive the excellent care they deserve. Unpredictable, but Never Unprepared Ushering in new life can bring a lot of surprises for parents, but the L&D department is prepared for any challenge. Whether the unit is helping with a routine or high-risk delivery, every patient and newborn are treated with personalized care that is uniquely tailored to their own individual needs and birth preferences, from labor evaluation and birth to post-birth lactation consultation and navigating the nursery. “Our floor is never predictable,” said Bri Goode, Renown L&D nurse. “Our nurses and our staff work as a team to ensure the best care for our patients. I commonly say that we are all 'nurses’ for each patient!” The state-of-the-art technology at their fingertips – including advanced 3D ultrasound machines – coupled with the love and passion the team has for their patients allows them to create an optimal environment for every mother and baby. The unit is also equipped with a Labor Assessment Area, where expectant mothers are evaluated to determine what stage of labor they are in, removing the guesswork and allowing providers to treat the patient and unborn child more efficiently and meet them exactly where they are at in the labor process. Nothing can replace the careful guidance and words of encouragement a patient needs in the delivery room. The L&D department are true patient advocates and firmly believe in the power of listening and the power of staying calm and collected. “To help our patients and ease their fears and anxieties, we always ensure them that our biggest goal is to have a healthy mom and healthy baby,” said Lindsay Strowmatt, Renown L&D nurse. “We constantly reinforce that they are strong and capable. Empowerment goes a long way!” “We always take the time to actually sit down and listen to the patient, no matter how busy we are,” added Krystie Mortensen, Renown L&D nurse and DAISY Award winner. “It’s important for us to understand where their nerves are stemming from and address any changes in plan of care along the way.” While the L&D unit is seen as a “happy place,” as described repeatedly by the members of the team, a seemingly low-risk patient can also turn into an emergency in a matter of seconds. "Our line of work can involve high-stakes emergency care,” said April Tucker, Renown L&D nurse. “We view change as a necessary part of growth, and we save lives.” These steps result in high patient outcome scores, which can be attributed directly to the unit. “We have continually great outcomes from hard work and consistency in care,” said Roya Galata, Renown L&D nurse and Nursing Organizations Alliance (NOA) Lifetime Achievement awardee. “I have tremendous love for my patients and the type of work I do.” Awards Without End With patient safety and experience always top of mind, and with the team continually going above and beyond for all parents and their newborns, it’s no wonder why the L&D department has achieved a long and growing list of both local and national awards and accolades. This year, U.S. News & World Report ranked the L&D unit at Renown Regional as "High Performing in Maternity Care – Uncomplicated Pregnancy.” This award is only the latest in this department’s “Best Of” accolades list, as the unit also achieved a win as the Best Place to Have a Baby in the 2022 Best of Reno Awards. Not only is the department continually recognized, but individual team members also receive coveted awards within their professional associations. As previously mentioned, Krystie Mortensen is a DAISY Award winner, which means that she has been recognized for the “super-human work” she has done throughout her career. Additionally, three team members, including Roya Galata, have received NOA awards, celebrating their contributions to the nursing profession as a whole. Many nurses in this department also choose to pursue lifelong learning by taking advantage of the educational benefits that Renown offers. Several team members have completed their continuing education in midwifery and advanced practice, reaffirming their dedication to delivering healthy babies and helping parents manage their first few days with their newborns. “The teamwork on this unit is phenomenal, and the energy and commitment that the staff comes in with every single day amazes me,” said Lora Carlson, Renown L&D Manager of Nursing. Internally, the L&D department loves to show their spirit at Renown. In December, they received the Best Holiday Decoration award during the 2021 holiday season. The team also enjoys participating (and scoring well) in Renown-sponsored Halloween costume contests. In 2023, the L&D department will only pursue greater heights to continue producing patient outcomes. A Work Family “I stay here because this is my family. My work family.” These strong words were proudly stated by Jeanne Bufkin, Renown L&D Surgical Technician, and echoed by virtually every L&D employee. Having each other’s backs during both times of need and times of celebration is a must in this department, and they do so proudly. “Our staff constantly back each other up,” added Lora Carlson. “They display a lot of adaptability and flexibility. That’s why our unit functions as well as it does.” Several team members in this department experienced the care of the L&D unit at Renown before they became fully-fledged employees. “I had two of my babies here and had wonderful experiences both times,” said Judy McBride, Unit Clerk. “I love being a part of the reason why the next woman can say the same!” Bri Goode also delivered her child at Renown and loved her experience so much that she was also inspired to join the team. “I chose to work at Renown because when I had such a positive experience during my delivery while I was in nursing school, I knew it was a team I wanted to be a part of.” Coming to Renown was clearly an easy decision for this team; staying at Renown is even easier. “I stay here because I love what I do and who I do it with,” said Judy McBride. “I truly feel like I am treated as an asset to this department, and it makes me want to come to work every day and make a difference in these mothers’ lives.” The closeness of this department and the top-of-the-line collaboration displayed by every provider can be felt by the patients during their entire stay at Renown. “We have an amazing collaborative team of physicians, nurses, scrub techs, unit clerks, patient access representatives and environmental services personnel that strive to provide our patients with the best possible care,” said April Tucker. The labor and delivery process is a team effort – and those interested in jumping in on this team effort are welcome to join. Delivering healthy babies and supporting new mothers are cornerstone acts in meeting Renown’s mission of making a genuine difference in the communities we serve. Our L&D department does precisely this and more, never giving up in Fighting the Good Fight.
-
Departamento destacado: Transporte en NICU
Bringing in new life is an exciting and beautiful occasion. The possibilities for the newest members of our world are endless – what will the child grow up to become? What will they achieve in their lifetime? Anyone will agree that a new life is precious and protecting that life by any means possible is a necessity. Sometimes, however, a baby’s journey into our world brings along obstacles. Prematurity, congenital defects and other complications can accompany a birth and the baby’s first few moments of life. But what happens when these complications happen outside of a fully-functioning Labor & Delivery unit, or if the complications need a special level of intervention with a health system capable of caring for their unique needs? Enter the NICU Transport team at Renown Health. As the only Neonatal Intensive Care Unit (NICU) Transport team in northern Nevada, these dedicated nurses, respiratory therapists and neonatal nurse practitioners – who have normal unit duties of their own at Renown Regional Medical Center – step up to the plate to take on this extra duty to support members of their community facing some of the scariest moments of their lives. To them, transporting babies in critical condition and giving them the best chance of life isn’t just a responsibility; it’s a calling. The NICU on Wheels When the Saint Mary’s maternity unit, which was Renown’s partner in NICU transport duties, made the decision to close, our dedicated NICU nurses and respiratory therapists diligently rose to the occasion to fill the demand. Dubbed the “NICU on Wheels,” Renown’s team went from taking on transport duties every other day to 365 days a year – and they are always ready to go at a moment’s notice, whether it’s by ambulance or by fixed-wing aircraft. “When we learned about the closure we knew it was our calling and knew we had to step up,” said Rachel D., Neonatal Transport RN at Renown. “We still have regular days on the floor, and we each switch off being on-call for transport. Once we get a distress call, we have 30 minutes to get to the hospital, grab our gear and go. We have to essentially put a whole room’s worth of portable equipment in one bag.” “I really enjoy being a part of the transport team and making a difference from northern Nevada to northern California,” added Sam V., Supervisor of Respiratory Care at Renown. “We are able to practice at the top of our skill level and use autonomy that not every practitioner gets to use.” Each NICU Transport unit works in teams of three when heading out into the field: one nurse (our bedside experts), one nurse practitioner (our education experts) and one respiratory therapist (our lung and breathing experts). With several years – and in many cases, decades – of experience in NICU nursing, NICU transport duties and respiratory therapy, this team is poised to provide state-of-the-art lifesaving care en route to the hospital. This diverse array of experiences among the team especially comes in handy as they continue to face the increased transport workload. “We are so thankful to have Saint Mary’s employees come over and work on our team after their maternity ward closed,” said Melyssa H., RN, NICU Transport Coordinator at Renown. “Helping the babies, as well as helping the scared families, will always be our top priority.” “I love the complexity that babies provide in the NICU,” added Jennifer J., Neonatal Transport RN at Renown. “Providing hands-on care right at the bedside along other members of the team is such a rewarding experience.” Education is also a crucial tool in NICU care, especially in the field. The nurse practitioners on this team make it their mission to outreach to the community, including our rural health partners, and help them build the tools and skills they need to care for our smallest and most critical patients. “I have been on a few transports where we went out and did not have to bring the baby over to the hospital, and we were able to provide lots of education instead,” said Shiela A., Respiratory Specialist at Renown. “For instance, I was called out to Fallon for a baby that was in respiratory distress. When we arrived, we saw the baby was awake and active although intubated. The tube came out, and we retaped it. While we stayed to observe the baby to make sure everything was okay, the nurse practitioner on the team provided educational tools to the family on what they can improve on regarding their baby’s tubing. Our nurses do such a great job with these teachings.” “When I started, I quickly noticed that more education was needed in the field,” added Jennifer J., RN. “Now I see the momentum we’ve had in these communities really take full force. Because of this education, and the confidence we instill in our patients’ families, each baby’s transition to our team has become so much easier. It has been awesome to watch this progress over the years.” With immense experience, education and a strong commitment to their community under their wing, the NICU on Wheels is only just getting started. Teamwork Makes the Dream Work Running a successful NICU Transport operation, especially as the sole health system participating, takes a village. With only three professionals out in the field, the team leans on their fellow nurses, physicians, surgeons and specialists to make the operation run as smoothly as possible. From REMSA and Care Flight helping load patients in and get them to the hospital safely, to Renown’s Clinical Engineering team who are first on the scene when machines need repairs and troubleshooting, everyone rises to the occasion to achieve the best-possible outcome for our youngest patients at some of the most challenging moments of the beginning of their lives – and they are fully trusted to move those mountains. “Being a part of the NICU Transport team has given us the opportunity to facilitate a deeper, meaningful relationship with providers and a patient’s entire care team,” said Rachel D., RN. “They entrust us with our assessment skills, opinions and skill levels. There is an equal layer of trust between us and them.” Despite the pressure they feel every day, the NICU Transport team never let it overtake them and instead let it empower them. “We are under a lot of pressure and stress regardless of the case, and yet, we all work so well together; the teamwork really is incredible,” said Lisa A., Respiratory Specialist at Renown. “I am very proud of how our team steps up and is very intricate, even down to organization. For example, team members like Shiela arrange all the respiratory bags and make sure they are laid out in a way that makes the procedure as simple as possible to ensure there are no complications.” The nurses and respiratory therapists also partner together on the NICU floor and are always ready to provide coverage when their transport colleagues get a call. Committed to collaboration and ready to jump into action, the NICU Transport team works together to elevate each other and the bottom line for each patient. “This is a full-time gig, and the group works together to make sure everyone is covered; we are all very collaborative,” said Sarah K., Respiratory Specialist at Renown. “We all think of our patients as extra special, and it’s nice to know that you can make a difference in the baby’s life and the lives of the family. We all have a sense of purpose in giving back to the community.” “I am just so thankful to be a part of this team,” added Marcia A., Neonatal Transport RN at Renown. “We really have developed a strong bond.” A Track Record of Success The life-saving measures that each member of the NICU Transport team take surpass hospital walls. The impact they have on each baby are remembered and celebrated for years, and they often develop lifelong relationships with patients and their families after their stay in the NICU. One prime example of this can be found in an impassioned letter from Tess, the mother of a young boy who was in the midst of respiratory distress and needed immediate intervention. Because of the valiant efforts of Renown’s NICU Transport team, her child, Warren, is a healthy and happy baby to this day. She recalls the experience: Warren had stopped breathing while getting routine blood work. He was resuscitated twice while at an area hospital. We made the decision to transfer him to Renown for him to be admitted into the NICU. Within an hour and a half of this decision, Renown had sent a team consisting of a respiratory therapist, nurse and nurse practitioner to come and get him. As soon as the team entered the room, we immediately felt safe and comforted. The team made sure we knew exactly what was going on and what was going to happen in the following hours, and they let us know they would do everything for Warren. He was resuscitated two more times by the respiratory therapist while getting ready for transport. At that time, the decision was made to intubate for a smoother ride to Renown. We knew you all had his best interest in mind, and of course, we trusted you with everything. The intubation went well, and he was packed up and ready to drive. Today, Warren is hitting all of his developmental milestones and is a normal, happy baby in everyone’s eyes. We can’t thank the NICU Transport team enough for taking such good care of Warren and helping him Fight the Good Fight. “This success wasn’t just due to our three-person unit – our manager, Jason, also jumped in and drove all the way to Carson City to stabilize the child,” said Shiela A. “This just goes to show that no matter our title, we are always here to help and make a huge difference in the lives of our patients.” Success stories of children like Warren describe the common mission of the NICU Transport team in detail, and while there are more of these stories to come, the team is always ready to make the necessary sacrifices for the greater good of their patients. “Sarah K. is like Warren’s guardian angel,” said Tess. “We call her ‘Auntie Sarah’ now. He wouldn’t be here if it weren’t for her and the entire NICU Transport team. It takes a special kind of person to work in the NICU. I can never repay this team for what they’ve done for Warren and our family.” “I am proud of this team, their flexibility and the sacrifices they have made to do transport 365 days a year,” added Melyssa H., RN.” The remarkable success of the NICU Transport team serves as proof of the unwavering and tireless commitment of each and every team member, bringing hope to families during their most difficult moments. “NICU Transport forces you to be confident in yourself and your abilities and to push yourself a step further,” said Rachel D., RN. “I am a better nurse because I joined the transport team.”
-
La lactancia no tiene por qué significar dolor en los pezones
If you think sore nipples are just a normal part of breastfeeding, think again. Robin Hollen, APRN, and Breastfeeding Medicine Specialist, says that nursing can be an enjoyable experience for mom and baby without pain and discomfort. A top concern of nursing moms within the first week after delivery is how to prevent sore nipples. Even moms who’ve nursed before struggle with this common issue. While many women think it is a regular part of the nursing experience, it is actually a sign that something isn’t quite right. “Nursing your baby should be enjoyable,” says Robin Hollen, Breastfeeding Medicine Specialist with Renown Health. For over 30 years Robin has been supporting moms to breastfeed. Below she shares some valuable information and tips, helping you create a happy and healthy breastfeeding experience for you and your baby. What causes sore nipples? The most common cause of sore nipples involves incorrect latching. For a proper latch, a baby’s mouth takes in the entire nipple and some of the breast, so that the nipple rests at the back of the mouth where the palate is soft. With an improper latch, the mouth may slip down to the tip of the nipple while the baby nurses. This constant pressure on your sensitive skin may cause discomfort and pain. A board-certified lactation consultant can help assess if your baby is latched correctly and troubleshoot your breastfeeding concerns. Less common causes of sore nipples include: • Improper tongue placement of baby • Clenching • Incorrect breast pump use How can a mother prevent sore nipples from an improper latch? Breastfeeding is a learning experience for both mom and baby. Ask for help with the latch so your baby learns it correctly and maintains its depth. In the past, new mothers were surrounded by a community of women — their own mothers, grandmothers, or other family and friends — to provide assistance and guidance with every latch at the beginning of an infant’s life. In today’s culture, new moms can find themselves on their own with no extended family to lend their knowledge. Nurses, pediatricians and lactation consultants now fill that role; they are the eyes and hands along with the much-needed experience to guide new mothers. Our Breastfeeding Medicine experts assist nursing moms with latch every day. Even a single visit with a lactation consultant observing your breastfeeding baby can provide valuable insight on achieving, and maintaining, the proper latch - preventing future nipple soreness and discomfort. How to heal sore nipples from breastfeeding To heal sore nipples, you must first fix the cause, and correcting the latch prevents further damage. A lactation consultant can also help you address the pain. Below are some breast healing tips: • Your own expressed breast milk is excellent to rub into the nipple for anti-bacterial protection. • For those moms who need more lubricant or fat than breast milk offers, use a lanolin or a cream that is labeled safe for the baby. • Soothies are a gel pads providing comfort in between feedings, but should not be used with lanolin products. • Breast shells, not to be confused with shields, can guard the nipples from irritation or pressure in between feedings. If you have more questions about preventing and healing sore nipples or general breastfeeding concerns, talk to your pediatrician or a Renown Health Breastfeeding Medicine specialist at 775-982-6365.
Read More About Breast Feeding Doesn't Have To Mean Sore Nipples
-
Cuidado confiable desde el hogar
Renown Health has always been on the frontlines of technological advancement, and that innovation remained unwavering during the COVID-19 pandemic. Our telehealth teams heeded the call to provide home monitoring for our patients, transforming how we provide care. The care providers at Renown successfully monitored lower acuity COVID-19 patients from the comfort of their own homes. Bernard Lee was diagnosed with COVID-19 and pneumonia, and was able to return home to continue his recovery with a home monitoring system. While at home, Bernard’s health took a turn for the worse while he was sleeping, but thanks to the continuous monitoring of Health at Home, his worsening vitals did not go unnoticed. “This monitoring system really saved my life,” Bernard said. “It was telling me that my sats were low, but I didn’t even feel the common COVID symptoms; I just felt tired.” Because of his low oxygen saturation (sats) and the continuous monitoring, he woke up to providers calling to check on him in the early morning. He was immediately transferred to the Renown Intensive Care Unit to be cared for and monitored by our expert care teams. Today Bernard is recovering, feeling great and continuously refers to the team and the home monitoring system as his guardian angels.
-
Cuidado al alcance de sus manos: Renown lanza verificador de síntomas virtual
La nueva tecnología ayuda a los pacientes a determinar el mejor nivel de atención para sus necesidades de salud. Renown Health acaba de anunciar una nueva herramienta digital diseñada para mantener a nuestra comunidad segura y saludable. Symptom Checker, que se lanzó hoy, es una plataforma fácil de usar basada en la web que evalúa los síntomas de los pacientes y los dirige sin contratiempos al nivel adecuado de atención dentro de la red Renown. Se puede acceder a Symptom Checker las 24 horas del día, los 7 días de la semana. Para ello, visite Renown Symptom Checker. A partir de allí, un paciente puede identificar cuál es la parte del cuerpo responsable de sus molestias y especificar sus síntomas. Al ingresar sus síntomas, los pacientes reciben un resumen de salud detallado y una guía de atención médica, que los ayuda a determinar la medida más adecuada que deben tomar. Los pacientes pueden programar una visita en una ubicación de Renown directamente a través del portal de Symptom Checker. Los pacientes que experimenten una emergencia médica no deben usar Symptom Checker y, en su lugar, deben llamar al 911. “Gracias a Symptom Checker, nuestros pacientes dispondrán de un apoyo permanente al alcance de su mano que les ayudará a tomar decisiones informadas sobre sus necesidades de atención médica”, declaró Tony Slonim, MD, DrPH, presidente y director ejecutivo de Renown Health. “Entendemos que determinar el nivel de atención adecuado para usted o sus seres queridos puede generar cierta incertidumbre, por lo que nos enorgullece ofrecer continuamente tecnologías nuevas e innovadoras que faciliten a los miembros de nuestra comunidad una vida más saludable”. “Debido a que continuamos experimentando casos de COVID-19 en el condado de Washoe, muchas personas con COVID-19 no están seguras de cuándo deben buscar atención médica, así como el lugar apropiado para recibirla”, explicó Melodie Osborn, RN (enfermera certificada), director de Calidad y Enfermería de Servicios de Salud. “Con Symptom Checker, las personas pueden ingresar fácilmente sus síntomas e incluir la gravedad de los síntomas, y a continuación se les indicará el mejor nivel de atención para sus necesidades de salud individuales. Esto hace que sea una herramienta extremadamente valiosa mientras nos esforzamos por mantener a nuestra comunidad segura y saludable en medio de esta pandemia”. Symptom Checker es de uso gratuito y no requiere que los usuarios sean pacientes de Renown. Además de las casi 200 guías de atención sintomática para niños y adultos, la plataforma también incluye 55 temas de primeros auxilios, 147 temas de asesoramiento sobre crianza de los hijos y 25 tablas de dosificación de medicina de venta sin receta para niños y adultos. El contenido de Symptom Checker está escrito por los médicos Barton Schmitt y David Thompson, que son expertos en triaje de enfermería; las guías de atención de síntomas surgen de los protocolos clínicos utilizados por los médicos y enfermeros de todo el mundo. Acerca de Renown Health Renown Health es la red de atención médica integrada de administración y propiedad local sin fines de lucro más grande de la región, que brinda servicios a Nevada, Lake Tahoe y el noreste de California. Con una fuerza laboral diversa de más de 7,000 empleados, Renown ha fomentado una cultura de excelencia, determinación e innovación de larga data. La organización se compone de un centro de urgencias, dos hospitales de cuidados agudos, un hospital infantil, un hospital de rehabilitación, un grupo médico y una red de atención de urgencias y Hometown Health, la compañía de seguros sin fines de lucro más grande de la región y de propiedad local, Hometown Health. El modelo del instituto de Renown aborda determinantes sociales de la salud e incluye: salud infantil, salud conductual y adicciones, envejecimiento saludable e innovación en la salud. Los institutos clínicos incluyen: cáncer, salud cardíaca y vascular y neurociencias. Actualmente, Renown está inscribiendo participantes en el estudio genético de salud poblacional basado en la comunidad más grande del mundo, el Healthy Nevada Project®. Visite renown.org para obtener más información.
Leer más Acerca de Cuidado al alcance de sus manos: Renown lanza verificador de síntomas virtual
-
Viuda de Reno inspira una nueva política de visitantes para Renown
Renown Health is one of the country’s first health systems to lift visitor restrictions for patients with COVID-19 and encourage the family to be at the patient’s bedside. Read Darlene and Dave’s story to understand why we’re updating our visitor policy. Dave and Darlene Randolph found joy in exploring antique shops and garage sales to find damaged or discarded vintage pieces. Dave would spend many hours scraping, cleaning, sanding, and refinishing items, transforming them into functional, beautiful pieces of furniture. Every piece in their home rekindles a memory and has a story to tell. On Thanksgiving, when Dave was too ill to gather around their antique dining room table, Darlene called the ambulance. Ailing with COVID-19 for two weeks, Dave had not been improving. When the EMTs reached her home and asked Darlene what underlying conditions he had, she said, “all of them.” David was seriously ill. Hospitalized for COVID-19, their communications options were limited. The only way Darlene could communicate with Dave was on a video call or by telephone. Dave spent 17 days hospitalized at Renown Regional Medical Center in Reno. Darlene spent 17 days waiting by the phone for more information on his condition. Darlene said he had “up days and down days,” but thought he might be home, sitting at their antique dinner table for Christmas. Sadly, Dr. David Randolph lost his battle with COVID-19 on December 13, 2020, and died as he slept in a hospital bed. When Darlene wrote his obituary for the newspaper, she gave thanks to the “tremendous nurses and doctors at Renown Regional Medical Center, for providing his care during a time when the family could not be with him.” Taking Action to Inspire Change Darlene wished she could have been there. Over their 45-year marriage, she had always been there. Darlene said, “I had always been at his bedside, as his advocate, to help communicate and straighten things out.” As a registered dietician, she worked in hospitals, knew the protocol, and knew that Renown had a restricted visitor policy to stop the virus’s spread- to other patients, staff, and their family members. Still, she wished she could have spent more time with him. On Christmas Eve, she sat down and wrote to Renown leadership. “As the wife of a COVID patient who recently passed away in your hospital, I want to express my thanks to you and your staff for the care he received in the last days of his life. I am aware that the nurses and staff are working under dangerous conditions and risking their health and lives by caring for multiple COVID patients. The staff is gracious, concerned, and doing everything they can.” She continued, “I know procedures are changing every hour to try to stay ahead of this dangerous virus, and I am sharing my experiences, hoping they will be helpful when establishing policies that impact families.” Darlene explained that despite receiving assurances that Dave’s nurse or a doctor would call daily, sometimes they would forget. She explains in her letter, “how important it is, in these times when the family cannot visit, and has only infrequent communication and is anxiously waiting at home for information about their loved one, how much it means to get a call from someone caring for him at the hospital. If there is a way you can help assure nurses have time to make calls or assist patients in making calls because it is an important part of patient care.” A Person-Centered Visitor Policy After receiving her letter, Renown leadership called Mrs. David Randolph to thank her, offer his sympathies and ask if Renown could help in any way. Darlene asked if he might reconsider allowing families to visit hospital patients during treatment for COVID-19. As the COVID-19 situation has evolved, the policy has as well. Renown hospitals and medical practices now encourage limited visitors for all patients, including those diagnosed with COVID-19. Renown also has extra safety measures to protect the health of patients, visitors and healthcare employees. Darlene is very pleased that her letter inspired this shift in visitor policies for patients with COVID-19. She says, “I have always tried to think of ways I could help other families. Especially those senior couples where one has been hospitalized and the other is home. My wish is to help others.” Renown Health Visitor Policy Renown Health patients may identify two healthy adult “patient supporters” to accompany them on their hospital stay. For more details, visit our Patient Supporter Guidelines page.
Read More About Reno Widow Inspires New Visitor Policy for Renown
-
Renown agradece a la comunidad a medida que termina el servicio desde el automóvil por la COVID-19
Después de administrar más de 73,000 vacunas de primera y segunda dosis a nuestra comunidad, el equipo de vacunación de Renown concluirá sus esfuerzos en el centro de vacunación al paso de Renown a finales de este mes. Renown Health ha tenido el placer de trabajar con el Distrito de Salud del Condado de Washoe, el estado y los Centros para el Control y la Prevención de Enfermedades (Centers for Disease Control and Prevention, CDC) para distribuir los suministros limitados de vacunas contra la COVID-19. Los líderes de la fuerza de trabajo que administra las vacunas contra la COVID-19 en Renown anunciaron hoy que el miércoles, 12 de mayo de 2021 será el último día en que la organización administrará la primera dosis de la vacuna contra la COVID-19 a los miembros de la comunidad en la clínica de vacunación al paso. La clínica de vacunas de Renown permanecerá abierta hasta que todas las personas que reciban su primera dosis de la vacuna a través de Renown tengan la oportunidad de recibir su segunda dosis. Hasta la fecha, el equipo de vacunas de Renown ha administrado más de 73,000 dosis 1 y 2 a miembros del personal médico, empleados de Renown, estudiantes, voluntarios y miembros de la comunidad elegibles. “Ha sido un honor ayudar a nuestros socios de salud locales y estatales en la heroica hazaña de vacunar a los cientos de miles de residentes de la zona que desean recibir la vacuna”, señaló Tony Slonim, MD, DrPH, presidente y director ejecutivo de Renown Health. “Ahora que concluimos nuestros esfuerzos en nuestra clínica de vacunación al paso, nos complace seguir trabajando estrechamente con los líderes de salud de nuestra comunidad y estar preparados para ayudar de nuevo en caso de que se necesite nuestro apoyo en el futuro. Nos enorgullece ser parte de la solución para nuestra comunidad y nos complace haber marcado una verdadera diferencia en la salud y el bienestar de las personas durante este tiempo sin precedentes en la historia”. “Mientras miramos hacia un futuro mejor más allá de la pandemia, no podemos dejar de reflexionar sobre las más de 73,000 dosis de vacunas que nuestros equipos administraron a nuestra comunidad”, declaró Melodie Osborn, RN (enfermera certificada), directora de Enfermería y Calidad de Servicios de Salud en Renown. “La administración de cada dosis de la vacuna fue posible, llueva, nieve o truene, gracias a los dedicados defensores de la atención médica comprometidos con la salud y la seguridad de los habitantes del norte de Nevada; entre ellos, se incluyen nuestros enfermeros, farmacéuticos, equipos de seguridad, expertos en seguridad pública y un sinnúmero de personal voluntario”. “Queremos ofrecer nuestro sincero agradecimiento y aprecio al público por confiar en Renown para recibir sus vacunas, y por su paciencia y apoyo a este importante trabajo”, comentó Wendy Meyers, gerente de Salud y Bienestar de Hometown Health. “Las sonrisas detrás de las mascarillas, las lágrimas de emoción provocadas por los sentimientos de gratitud y alivio, los agradecimientos sinceros, las entregas de alimentos y muchos otros actos de bondad ocuparán siempre un lugar especial en nuestros corazones”. Los miembros de la comunidad mayores de 16 años que aún estén interesados en recibir la vacuna de Pfizer en Renown el 12 de mayo están invitados a programar una cita a través de MyChart; se aceptarán visitas sin cita desde las 12 p. m. hasta las 2 p.m. Los menores de 16 y 17 años deben estar acompañados por su padre, madre o tutor para recibir la vacuna. Para obtener asistencia, llame al 775-982-2781. Para programar su cita de vacunación contra la COVID-19 en el condado de Washoe fuera de Renown, visite covid19washoe.com. Renown seguirá proporcionando actualizaciones continuas para ayudar a mantener la seguridad de nuestra comunidad en nuestro sitio web covid.renown.org. Acerca de Renown Health Renown Health es la red de atención médica integrada de administración local y sin fines de lucro más grande de la región, que presta servicios a Nevada, Lake Tahoe y el noreste de California. Con una fuerza laboral diversa de más de 7,000 empleados, Renown ha fomentado una cultura de excelencia, determinación e innovación de larga data. La organización se compone de un centro de urgencias, dos hospitales de cuidados agudos, un hospital infantil, un hospital de rehabilitación, un grupo médico y una red de atención de urgencias y Hometown Health, la compañía de seguros sin fines de lucro más grande de la región y de propiedad local, Hometown Health. Los institutos clínicos abarcan los campos de cáncer, salud cardíaca y vascular y neurociencias. Actualmente, Renown está inscribiendo participantes en el estudio genético de salud poblacional basado en la comunidad más grande del mundo, el Healthy Nevada Project®. Para obtener más información, visite renown.org.
-
Eliminar el trabajo de adivinanza con el área de evaluación laboral de Renown
Pictured above: A section of Renown’s Labor Assessment Area. When patients expecting a new child are about to give birth, nerves can be especially heightened. Questions flood their minds: Is the baby actually on the way? What’s going to happen next? Are we ready to push? Lucky for them, at Renown Health, the guesswork can finally end with Renown’s Labor & Delivery unit Labor Assessment Area. This unique space is a triage area that helps make more precise labor diagnoses by determining exactly what stage expectant parents are at in the labor process. Funded by a state grant more than a decade ago, the six-bed Labor Assessment Area sees 500-600 patients per month – from patients entering the unit directly, unsure if they are in active labor, to patients who are sent over from elsewhere experiencing labor symptoms, such as high blood pressure and water breaking. The area also serves as a pre-operation space for patients getting ready for procedures such as C-sections. The six cubicles that are enclosed with doors and curtains ensure each patient gets the private, one-on-one care they need. Furthermore, rather than sitting in a waiting room, this area allows expectant parents a comfortable place to prepare for labor. “We are a unit that prides ourselves on getting patients into beds very quickly,” said Debbie Hawley, Associate Nurse Manager in Renown’s Labor & Delivery unit. “This area has allowed us to triage more effectively and allow more patients to collaborate with their provider in a quick manner.”
Read More About Remove the Guesswork with Renown’s Labor Assessment Area
-
Reno Widow inspira una nueva política de visitantes que apoyan a los pacientes
Los hospitales de Renown están entre los primeros del país en eliminar las restricciones de visitantes para pacientes con COVID-19 y anima a las familias a acompañar a los pacientes en el lugar. El Dr. Dave y Darlene, verdaderos cazadores de tesoros, disfrutaban de explorar tiendas de antigüedades y ventas de garaje para encontrar piezas antiguas dañadas o desechadas. Después de llevar el objeto a casa, Dave dedicaba muchas horas a limpiarlo, lijarlo y pintarlo nuevamente hasta que brillara y se convirtiera en una pieza pulida, funcional y hermosa del mobiliario. Cada pieza de su hogar revive un recuerdo y tiene una historia que contar. En el Día de Acción de Gracias, cuando Dave estaba demasiado enfermo para sentarse en su antigua mesa de comedor, Darlene llamó a la ambulancia. Dave llevaba dos semanas enfermo de COVID-19 y no mejoraba. Cuando los técnicos en emergencias médicas (Emergency Medical Technician, EMT) llegaron a su casa y le preguntaron a Darlene qué afecciones subyacentes tenía Dave, ella dijo: “todas”. David estaba gravemente enfermo. Dado que fue hospitalizado por COVID-19, sus opciones de comunicación eran limitadas. La única forma en que Darlene podía comunicarse con Dave era mediante una videollamada o por teléfono. Dave pasó 17 días hospitalizado en el Renown Regional Medical Center en Reno. Darlene pasó 17 días esperando junto al teléfono para obtener más información. Darlene dijo que él tenía “días buenos y días malos”, pero pensó que podría estar en casa, sentado en su antigua mesa para la cena de Navidad. David Ivan Randolph nació en Boston, MA, el 29 de agosto de 1936. Creció en Roxbury y se graduó en la prestigiosa Boston Latin Boys School. Obtuvo una Licenciatura en Artes con especialización en Psicología general, una Maestría en Psicología Experimental de la Northeastern University y un doctorado en Psicología Sensorial y Fisiología de la Universidad de Massachusetts, Amherst. Mientras estaba en la universidad, se incorporó al Cuerpo de Entrenamiento de los Oficiales de Reserva (Reserve Officer Training Corps, ROTC) y, tras su graduación, fue nombrado Teniente en el Cuerpo de Especialistas Médicos del Ejército. Después de la capacitación básica en la Escuela de Capacitación Médica Fort Sam Houston, fue asignado como psicólogo de investigación (capitán) al Ejército de los EE. UU. en la División de Investigación Pionera en Natick, MA. Durante los siguientes 30 años, llevó a cabo una investigaciones sobre la visión en Fort Knox, KY; Filadelfia, PA y, luego, con el recientemente construido Letterman Army Institute of Research (LAIR), División de Riesgos Oculares en el Presidio de San Francisco, CA. David continuó su investigación de la visión en LAIR hasta su jubilación en 1992, cuando el Presidio fue desmantelado. Los hallazgos del Dr. Randolph en materia de ceguera por destello y visión nocturna lo convirtieron en un ponente muy solicitado en conferencias de investigación en Estados Unidos y en el extranjero. En un documental de la PBS se le entrevistó como parte del equipo que desarrolló las gafas que protegen a los soldados de los daños oculares causados por el láser. El Dr. David Randolph perdió su lucha contra la COVID-19 el 13 de diciembre de 2020, y murió mientras dormía en una cama de hospital. Cuando Darlene escribió su obituario para el periódico, dio las gracias a los “excepcionales enfermeros y médicos del Renown Regional Medical Center, por proporcionarle los cuidados necesarios durante el tiempo que la familia no pudo estar con él”. Darlene deseaba haber estado allí. Durante sus 45 años de matrimonio, ella siempre estuvo allí. Darlene dijo: “Siempre he estado junto a su cama, como su defensora, para ayudar a comunicar y enderezar las cosas”. Como nutricionista registrada, trabajó en hospitales y conocía el protocolo. Sabía que, al igual que los hospitales de todo el mundo, Renown había restringido la visita de los miembros familiares para detener la propagación del virus a otros pacientes, al personal y a sus familias. Aun así, ella deseaba poder pasar más tiempo con él. En la víspera de Navidad, se sentó y le escribió al Dr. Anthony Slonim, presidente y director ejecutivo de Renown Health en Reno, NV. “Estimado Dr. Slonim: como esposa de un paciente con COVID-19 que ha fallecido recientemente en su hospital, quiero expresarle mi agradecimiento a usted y a su personal por la atención que recibió en los últimos días de su vida. Soy consciente de que los enfermeros y el personal están trabajando en condiciones peligrosas y arriesgan su salud y su vida al atender a múltiples pacientes con COVID-19. El personal fue amable, se preocupó e hizo todo lo posible por mi esposo y por mí”. Darlene continuó: “sé que los procedimientos cambian cada hora para intentar adelantarse a este peligroso virus, pero compartiré mis experiencias con la esperanza de que sean útiles a la hora de establecer políticas que afecten a las familias”. Darlene explicó que, a pesar de recibir garantías de que el enfermero de Dave o incluso un médico llamarían todos los días, a veces se olvidaban. En su carta, ella explicó: “lo importante que era recibir una llamada de alguien que cuidara de él en el hospital, especialmente en estos momentos en los que la familia no puede visitar, que solo tiene una comunicación infrecuente y que espera ansiosamente en casa noticias de su ser querido”. Darlene preguntó al Dr. Slonim “si hay alguna manera en la que [él] pueda ayudar a garantizar que el personal de enfermería tenga tiempo para hacer llamadas o ayudar a los pacientes para que hagan llamadas, porque es una parte importante de la atención de los pacientes”. Después de recibir su carta, el Dr. Slonim llamó a la esposa de David Randolph para darle las gracias, ofrecerle sus condolencias y preguntarle si Renown podía ayudar de alguna manera. Darlene le preguntó si podría reconsiderar la posibilidad de permitir que las familias visitaran a los pacientes del hospital que recibían tratamiento para la COVID-19. El Dr. Slonim, que también había perdido a su padre por COVID-19 en abril en un hospital de Nueva Jersey, le pidió a su equipo de liderazgo que revisara la solicitud de la Sra. Randolph e hiciera una recomendación. El equipo de liderazgo del hospital hizo una recomendación al Dr. Slonim que fue aprobada inmediatamente. A medida que la situación de la COVID-19 ha evolucionado, la política también lo ha hecho. Con un alto porcentaje del personal hospitalario de Renown vacunado contra la COVID-19, el descenso de las hospitalizaciones de pacientes con COVID-19 y la comprensión de que la mejor comunicación es la que se produce en persona, a partir de la mañana del miércoles, 27 de enero de 2021, los hospitales y consultorios médicos de Renown permiten visitantes limitados para todos los pacientes, incluidos los diagnosticados con COVID-19. Renown sigue contando con medidas de seguridad adicionales para proteger la salud de los pacientes, los visitantes y los empleados de atención médica, y como la situación cambia con la COVID-19, estas directrices están sujetas a cambios. “Al partir de hoy, una persona sana de apoyo al paciente puede acompañar al paciente durante su visita médica o su período de hospitalización”, anunció Tony Slonim, MD, DrPH, presidente y director ejecutivo de Renown: “Vivimos según nuestros valores de atención, integridad, colaboración y excelencia. Le agradecemos a Darlene por recordarnos que la mejor atención es la “atención centrada en las personas”, un enfoque que adopta la perspectiva del paciente y sus seres queridos, mientras promueve un entorno saludable y alentador para los cuidadores y aborda las necesidades de salud de nuestra comunidad”. “En Renown, son los pacientes quienes determinan el significado de la palabra ‘familia’”, afirma Debra Adornetto-Garcia, DNP (licenciada en enfermería), RN (enfermera certificada), NEA-BC (certificación avanzada en enfermería ejecutiva), AOCN (enfermera certificada en oncología avanzada), directora de Enfermería de Servicios Agudos. “Los pacientes pueden designar a cualquier persona que deseen como su persona de apoyo. La figura de la persona de apoyo al paciente es increíblemente importante y forma parte del equipo de atención. Le solicitaremos a esta persona que colabore con el equipo de atención médica del paciente; esto implica ayudar con las comunicaciones a otros miembros familiares y amigos, participar en actividades de capacitación y educación, y ayudar al paciente a cumplir las instrucciones respecto de la atención y los medicamentos. “Cuando se trata de curarse y recuperarse, el papel de todos es importante”, enfatiza Paul Sierzenski, MD, MSHQS, CPE, FACEP, director médico de Servicios Agudos. “Lo que podemos hacer juntos para apoyar la atención al paciente y los resultados excelentes es mucho mejor que lo que cualquiera de nosotros puede hacer solo. Esta creencia da forma a nuestro trabajo, nuestros servicios y la atención que brindamos a los pacientes, sus familias y amigos en Renown”. “Me complace que Renown Health haya modificado las políticas de visitantes para que cada paciente pueda tener un visitante designado. Como expaciente de la Unidad de Cuidados Intensivos (Intensive Care Unit, ICU) y médico actual de esa misma área, sé lo importante que es contar con el apoyo de un ser querido en el hospital y estoy entusiasmado de poder adaptar este aspecto increíblemente importante de la atención al paciente”, afirma Jacob B. Keeperman, MD, FACEP, FAAEM, FAEMS, FCCM, director médico, Renown Regional Transfer and Operations Center, intensivista. Cuando le comunicaron a Darlene que su carta había inspirado este cambio en las políticas de visitantes para los pacientes con COVID-19, se mostró muy satisfecha y dijo: “siempre he tratado de pensar en formas de ayudar a otras familias, especialmente a las parejas de personas mayores en las que uno ha sido hospitalizado y el otro está en casa. Mi deseo es ayudar a los demás”. De acuerdo con las pautas nacionales, a partir del 1/27/2021, una persona de apoyo al paciente podrá acceder a Renown Regional Medical Center y a Renown South Meadows Medical Center según se indica a continuación: El horario de visitas para todos los pacientes, incluidos los diagnosticados con COVID-19, se extenderá de 8 a. m. a 8 p. m. (anteriormente de 3 a 8 p. m.). Ahora se recomienda a todos los pacientes que designen hasta dos personas de apoyo. Debido a limitaciones de espacio, pedimos que las personas de apoyo al paciente realicen visitas individuales. Los pacientes proporcionarán los nombres de hasta dos personas de apoyo al paciente durante la internación/inscripción de pacientes. Los nombres de las personas de apoyo al paciente se ingresarán en el registro médico electrónico del paciente por motivos de privacidad y seguridad del paciente. Renown Children’s Hospital: Acceso abierto. (Se puede designar a dos padres o tutores como personas de apoyo para el paciente, no obstante, debido a las restricciones actuales de espacio, solicitamos que se presente uno a la vez). Para obtener información detallada sobre el programa de persona de apoyo al paciente, visite https://www.renown.org/interact/. Acerca de Renown Health Renown Health es la red de atención médica integrada de administración y propiedad local sin fines de lucro más grande de la región, que brinda servicios a Nevada, Lake Tahoe y el noreste de California. Con una fuerza laboral diversa de más de 7,000 empleados, Renown ha fomentado una cultura de excelencia, determinación e innovación de larga data. La organización se compone de un centro de urgencias, dos hospitales de cuidados agudos, un hospital infantil, un hospital de rehabilitación, un grupo médico y una red de atención de urgencias y Hometown Health, la compañía de seguros sin fines de lucro más grande de la región y de propiedad local, Hometown Health. El modelo del instituto de Renown aborda determinantes sociales de la salud e incluye: salud infantil, salud conductual y adicciones, envejecimiento saludable e innovación en la salud. Los institutos clínicos incluyen: cáncer, salud cardíaca y vascular y neurociencias. Actualmente, Renown está inscribiendo participantes en el estudio genético de salud poblacional basado en la comunidad más grande del mundo, el Healthy Nevada Project®. Visite renown.org para obtener más información.
Leer más Acerca de Reno Widow inspira una nueva política de visitantes que apoyan a los pacientes
-
Trabajo de parto y parto
Having Your Baby at Renown Renown Health’s Labor & Delivery Center, located at Renown Regional is nationally ranked for our maternity care. We proudly deliver more babies annually than any other hospital in the region. As your trusted care partner, we work to provide a personalized birthing experience that begins long before your first contraction and continues well after delivery. With state-of-the-art amenities and a compassionate team of care providers, we deliver advanced maternity care while making your birth experience as joyous and comfortable as possible.
-
Cómo almacenar la leche materna de manera segura
Breast milk. It's often referred to as liquid gold. And fortunately, it can be safely refrigerated or frozen for later use, which can allow you to be a bit more flexible in your new routine with baby. Whether you're getting ready to return to work, planning for the chance date night out or just exclusively pumping, it's crucial to understand the guidelines for proper breast milk storage. Storing Breast Milk Use clean bottles with screw caps, hard plastic cups that have tight caps or nursing bags (pre-sterilized bags meant for breast milk). Be sure to label each container with the date the milk was pumped and your baby's name if the milk is going to childcare providers. You can add fresh, cooled milk to milk that is already frozen, but add no more than is already in the container. For example, if you have two ounces of frozen milk, then you can add up to two more ounces of cooled milk. For healthy full-term infants, milk can be stored as follows: Room temperature - six to eight hours (no warmer than 77°F, or 25°C). Refrigerator - up to five days at 32°-39°F (0°-3.9°C). Freezer– Varies depending on freezer type. Up to two weeks in a freezer compartment located within the refrigerator. Three to six months in a freezer that is self-contained (standard kitchen fridge/freezer combination) and kept at 0°F (-18°C). Breast milk should be stored in the back of the freezer and not in the door. Six to 12 months in a deep freezer that is kept at -4°F (-20°C). Be sure to leave about an inch of space at the top of the container or bottle to allow for expansion of the milk when it freezes. Thawing Breast Milk Place frozen breast milk in the refrigerator to thaw (about 24 hours) then warm by running warm water over the bag or bottle of milk and use it within the next 24 hours. If you need it immediately, remove it from the freezer and run warm water over it until it's at room temperature. Never microwave breast milk and do not refreeze it. Once your baby has started to drink from the bottle, you should use it within one hour. You may find that different resources provide different recommendations about the amount of time you can store breast milk at room temperature, in the refrigerator and in the freezer. Talk to your doctor or lactation consultant if you have any concerns or questions.
-
Los mejores consejos seguros para dormir para su bebé
Becoming a parent for the first time means lots of new unknowns – from learning to breastfeed and swaddle to buckling your newborn into the car seat for the first time. But when it comes to putting them to bed safely, it’s important to remember it really can mean life or death. It’s something we’re taught before our little one is even here: the correct way to put your baby to bed safely. Sadly though, the number of infant deaths continues to climb. The main culprit of sleep-related infant death continues to be all the items parents leave in the crib with their babies. According to the Center for Disease Control and Prevention, there are about 3,500 sleep-related deaths among babies each year. “The best advice is ‘bare is best.’ Keep your infant’s sleep space clutter free – no blankets, bumpers, toys or pillows,” said Karen Wagner, Pediatric Nurse Practitioner. Follow the ABCs for Safe Sleep Remembering the ABCs is an easy way to remember how to put your little one to bed safely. A: Alone No blankets, toys or pillows. “We do recommend using a sleep sack as a blanket alternative,” said Karen. “It prevents the risk of suffocation and keeps your baby warm.” Keep in mind, the greatest risk for suffocation happens when babies are under 1 year of age, so it’s best to save the toys, blankets and pillows for their “big kid bed,” or around 18 months old. B: Back The slogan “back is best” is another good reminder. Keeping your baby on their back until they’re old enough to rollover helps reduce the risk of Sudden Infant Death Syndrome (SIDS). C: Crib It is best to have your baby sleep alone in their crib. While co-sleeping may be enticing, especially after a late-night feed, it increases the risks of possible suffocation. However, “having your child in your room, in their own crib or bassinet, is protective for SIDS,” Karen said. “In fact, we think co-rooming reduces SIDS risk by almost 50 percent.” Co-rooming allows parents to keep new babies in close reach and helps parents oversee their baby’s sleep, just in case something happens.