Buscar
-
Departamento destacado: Farmacia
When it comes to each patient’s healthcare journey, medication is often a key chapter. After all, medication is one of the most common treatment methods to help patients on the road back to health. In 2023, 4.83 billion prescriptions were filled in the U.S., and with this number only anticipated to rise annually, having an expert pharmacy team on your side to make certain you are prescribed the ideal dosage to treat your condition, prepare your prescriptions on time and help you manage your medications responsibly is important. Fortunately, at Renown Health, we have best-in-class inpatient and outpatient pharmacy teams to fill both prescriptions and promises for excellent care. Renown Pharmacy plays a vital role in helping us foster a health system that prioritizes patient well-being above all else. This department exemplifies the impact that a unified, expert pharmacy team can have on patient outcomes now and in the future. The Masters of Medication Spanning three hospitals plus ambulatory locations across the health system, Renown’s growing pharmacy team – full of dedicated pharmacists, pharmacy technicians and even medical assistants – manages medications in a wide variety of patient settings, touching nearly every aspect of the healthcare continuum: Outpatient Retail Pharmacies Renown Regional Medical Center – 75 Pringle Way The Healthcare Center – 21 Locust Street Renown South Meadows Medical Center – 10101 Double R Blvd Inpatient Pharmacies Renown Rehabilitation Hospital Renown Regional Medical Center (including Renown Children’s Hospital) Renown South Meadows Medical Center COMING SOON: Conrad Breast Center Pharmacy (in honor of Kristina Ferrari) in the Specialty Care Center at Renown South Meadows Ambulatory Pharmacies Anticoagulation Services – Institute for Heart & Vascular Health (IHVH) Pharmacotherapy Program – IHVH and Renown Medical Group Locations Congestive Heart Failure Pharmacotherapy Program – Center for Advanced Medicine B at Renown Regional Chronic Obstructive Pulmonary Disease (COPD) Pharmacotherapy Program – Renown South Meadows Endocrinology Pharmacotherapy Program – Renown South Meadows Clinical pharmacists at Renown bridge the gap between medicine and compassionate support, making sure each patient receives personalized care one prescription at a time. “There are various roles pharmacists play within Renown,” said Clarissa Munoz, Clinical Pharmacist in the Renown Regional Inpatient Pharmacy. “Staff pharmacists work diligently to ensure correct medications are dispensed, and if compounded, make sure they were prepared properly. They also work hard to answer medication messages and phone calls, help verify orders and make sure ode trays/RSI kits are appropriately stocked and ready when needed. Clinical pharmacists work from satellite pharmacies on the floor and focus on reviewing patient charts and aim to provide additional interventions to the providers to optimize treatment strategies. We also serve as a resource for nursing staff and help answer medication questions.” “My role in the pharmacy is pretty expansive,” added Chanelle Ajimura, Clinical Pharmacist in the Renown Regional Outpatient Pharmacy. “I maintain inventory to confirm patients can receive their medications in a timely manner both for our discharge and retail patients while balancing the Meds to Beds program, which offers medication delivery to the bedside and bedside medication counseling; collaborating with an interdisciplinary team to find the most affordable price for patients; and verifying that the dose, strength, indication, etc. is appropriate for the patient from start to finish.” “In the pharmacy, I make sure patients are receiving appropriate drug therapy by checking for major drug interactions and ensuring appropriate dosing,” added Courtney Church, Clinical Pharmacist in the Renown Regional Outpatient Pharmacy. “I also make recommendations to providers so patients can get cost-effective therapy.” Our pharmacy technicians work behind-the-scenes ensuring efficient medication management, making a difference in the lives of patients every day. “A pharmacy technician is responsible for making sure the patient gets their medications on time and at the lowest price possible,” said Nate Graham, Pharmacy Technician in the Renown Regional Outpatient Pharmacy. “This is done by working with patients, insurance companies and case workers. We fill prescriptions, enter prescriptions into our system, receive and send orders for medications and maintain a clean pharmacy with an accurate inventory.” “We do a variety of things; the task people probably know the most is counting out the medications and putting them in the amber vials,” added Rachel Vallin, Pharmacy Technician in the Renown Regional Outpatient Pharmacy. “We also help patients at the front of the pharmacy, ring out their prescriptions, answer some basic questions (deferring to a pharmacist as necessary) and billing insurance. Meds to Beds is my favorite part because I feel the most involved. I take medications to patients who are discharging up to their hospital rooms so they have it with them when they leave.” “As a technician, I confirm that all medications of new admissions are available in our machines prior to admitting and then maintain stock during each patient’s stay,” added Tammara Axtman, Pharmacy Technician at Renown Rehabilitation Hospital. "I also assist our nurses when needed in regard to any of their questions with both EPIC and Omnicell.” Our pharmacy team is also on the move all across our health system, thanks to our Ambulatory Pharmacy programs. For patients experiencing a serious heart, lung, or endocrine condition that requires ongoing drug therapy maintenance and guidance, our ambulatory pharmacies step in to carefully monitor how their medications impact their health and well-being. “Our role as pharmacists in this department is non-traditional because we actually see patients in the exam rooms face-to-face,” said Cory Lankford, Ambulatory Care Clinical Pharmacist for Renown’s Anticoagulation Services. “We modify their medication regimens and drug recommendations under collaborative practice agreements.” “Because our role is so unique, we have a lot of opportunities to make a positive impact on patients,” added Janeen Abe, Ambulatory Care Clinical Pharmacist for Renown’s Anticoagulation Services. “We do a lot of direct patient interaction, including counseling patients on their medications and helping them navigate through their disease state.” “As a medical assistant in this department, we’re called the patient ‘liaisons’ to orchestrate who they should go to whether it’s a nurse, a provider or a pharmacist,” added Kiara Scruggs, Medical Assistant for Renown’s Anticoagulation Services. “We look at each patient’s medications and help with the Warfarin blood thinner monitor. We get to do a lot with patients." No matter the diagnosis, having Renown Pharmacy as an integral part of your healthcare team is a win-win situation for both you and them: you receive access to medication to help you heal, delivered to you with precision and care, and the pharmacy team has the opportunity to care for you and make a positive impact, a role they take seriously.
-
Know when to visit an ER: Top 5 concerns
When a sudden illness or injury occurs, the emergency room (ER) provides immediate medical attention to those in need. Understanding the top reasons for visiting the ER can help people make informed decisions about seeking emergency care. Here are the five most common reasons people in Nevada visited an ER in 2023. 1. Abdominal pain One of the top reasons people visit the ER is abdominal pain. The abdomen has many organs, including the stomach, liver, small and large intestines, gallbladder and pancreas. Significant pain in this area can be a cause of concern. Warning signs of a serious problem include abdominal pain with fever, vomiting, and not being able to move or perform everyday tasks due to pain. Seeking medical attention when experiencing these symptoms is essential. Emergency physicians can perform abdominal exams, assess the condition and rule out significant threats. 2. Fever High fevers that do not get better with medicine and are accompanied by other symptoms can cause concern. This can indicate that the body is fighting off an infection or illness. Fever with symptoms like vomiting, pain, altered mental status, shortness of breath or inability to perform daily functions are warning signs to watch out for. Adults and children should visit an ER, where the team can assess the causes of the fever. 3. Chest pain and shortness of breath Chest pain and discomfort, or pain in the upper body can suggest warning signs of a heart attack. If a person is experiencing signs of a heart attack, call 911 immediately to ensure timely treatment or assessment by a medical professional. Heart attack symptoms include: Chest pain, including pain that can be described as chest pressure, heaviness or squeezing Discomfort in the chest, arms, back, neck, shoulders and jaw Difficulty breathing Sweating with any of the above symptoms When visiting a Renown ER for chest pain, a trained medical professional will promptly perform an Electrocardiogram (EKG) in an area where preliminary assessments, also known as triage, take place. Individuals experiencing shortness of breath or trouble breathing, whether from a respiratory infection, asthma complications or other pre-existing conditions should not ignore symptoms as these can signify more serious issues. Warning signs of respiratory distress may include: A significant change in breathing rate A significant change in the amount of energy used to inhale or exhale when breathing Changing of the skin color to blue, gray or paleness, which can indicate a lack of oxygen Nasal flaring Chest retractions, which can suggest difficulty bringing air into the lungs What this looks like: the chest sinking in just below the neck, breastbone or rib cage while breathing 4. Neurological symptoms Sudden and severe headaches or seizures may prompt individuals to visit the ER if symptoms are extremely disorientating or debilitating. These symptoms could be indicative of various conditions, including strokes or neurological disorders that require prompt evaluation. If a person is experiencing signs of stroke, call 911 immediately to ensure timely treatment. Stroke symptoms include: Numbness, weakness or loss of movement in the face, leg or arm, especially on one side Confusion, including trouble speaking or understanding Trouble with vision or loss of balance When choosing emergency care for signs and symptoms of stroke, a Comprehensive Stroke Center can provide patients with immediate intervention, including evaluation, treatment and education. 5. Cough/flu-like symptoms Emergency departments are staffed by medical professionals trained to prioritize and treat emergency and trauma situations. Receiving care at an ER should be reserved for severe symptoms and life-threatening conditions. It’s best to schedule a visit with a primary care physician for mild cold and flu symptoms. Most urgent care locations are equipped with rapid testing options, including RSV, COVID-19, influenza, mononucleosis, urinary issues and strep throat. It is critical to distinguish between common respiratory infections and more severe cases, such as pneumonia or complications from the flu. Symptoms that may warrant a visit to the ER include: Rapid decline in the ability to perform regular daily activities Coughing or throwing up blood Severe dehydration and inability to drink fluids High fever not responsive to medication Understanding top ER visits in Nevada While these ER complaints are common reasons for emergency room visits in Nevada, it's important to remember that emergency care is available for all immediate medical needs. Do not hesitate to seek help at an emergency room if someone experiences a sudden or severe health concern. Quick and appropriate action can make a significant difference in keeping you and your loved ones healthy. Renown Health is the largest locally governed, not-for-profit healthcare network in northern Nevada, providing leading emergency and trauma care by board-certified emergency physicians 24/7 at three locations, including the region’s only pediatric emergency department. Renown Health emergency rooms prioritize swift assessments, advanced diagnostic tools and compassionate care, providing leading emergency and trauma care. Trust Renown ER for not just emergency care but exceptional care. Learn more at renown.org/ER.
-
El Papel de los Ginecólogos Obstetras en la Atención de la Salud de la Mujer
Obstetrician-gynecologists (OBGYNs) see patients from menses (the monthly menstrual cycle that occurs as a part of the female reproductive system), pregnancy and childbirth through menopause and play a pivotal role in managing reproductive health and overall wellness. Dr. James Alexander with Renown Women's Health explains. "As experts in women's health, we are uniquely positioned to recognize subtle changes or symptoms that might indicate broader health issues. This comprehensive approach allows us to serve as a valuable first touchpoint for various health concerns." Preventive Screenings: A Proactive Approach One key aspect is an OBGYN's ability to recommend preventive screenings based on your symptoms, age, lifestyle and medical history. For instance, lipid screenings are critical for monitoring cholesterol levels, which can be a significant factor in women’s heart disease. An OBGYN keeps up with the current guidelines for routine screening as well as in women with risk factors such as high blood pressure, diabetes, or a family history of heart disease during your visit. By identifying risks and abnormal screening early, they can collaborate with you to implement lifestyle changes or treatments to reduce your risk of heart conditions. Schedule Your Screening Appointment Make an Appointment by Phone: 775-982-5000
Read More About The Expanded Role of OBGYNs in Women's Healthcare
-
Most Common Reasons Women Visit the ER
If you or someone you know is experiencing a medical emergency, it's essential to seek immediate attention by calling 9-1-1 or visiting the ER for a thorough evaluation by a trained medical professional and timely intervention. Access to a convenient and trusted emergency room (ER) is critical to any person’s healthcare needs, including medical emergencies related to women’s health. We explored some common scenarios and warning signs prompting women to seek immediate medical attention with Aiden Gould, Board-Certified Emergency Physician at Renown Health. When your medical emergency can’t wait, Renown ER is here to provide you with the region’s leading emergency care to diagnose and treat your condition or illness. Understanding Common Reasons Women Visit the Emergency Room Gynecological Emergencies: One of the most common reasons women may seek emergency care is due to gynecological emergencies such as severe pelvic pain, abnormal bleeding or complications related to pregnancy. These issues can be alarming and warrant immediate medical attention if the issue persists or is out of the ordinary for you. Emotional and Physical Well-Being: For those facing diverse medical or mental health emergencies, seeking prompt assistance is crucial for a thorough assessment and safe, timely intervention. Renown ER teams are equipped with trained professionals who provide compassionate care for individuals seeking help in the following situations: Suicide risk assessment and intervention Substance abuse assessment Assault and trauma care Crisis support and intervention Resources for ongoing care and well-being support Severe Abdominal Pain: Unexplained and severe abdominal pain that is substantially different than what is normal for you is a symptom you should never ignore as it can indicate underlying issues. Warning signs of an acute medical situation include fever, vomiting or a rapid change in motor function and inability to move due to pain. Respiratory Distress: Difficulty breathing, persistent coughing and other respiratory issues can be especially concerning. Women with pre-existing respiratory conditions like asthma or those experiencing sudden respiratory distress should seek immediate care from a medical professional. Warning signs of respiratory distress may include a significant change in one’s breathing rate, changing of the skin color to blue, gray or paleness due to lack of oxygen, nose flaring and chest retractions. Cardiovascular Emergencies: Heart-related issues are not exclusive to men. Women can also experience cardiovascular emergencies that often go undiagnosed because symptoms differ from men. Symptoms like chest pain, extreme fatigue, vomiting or pain in the abdomen, shortness of breath or palpitations should be evaluated by an emergency medical professional as timely intervention is critical in such cases. Renown leads the region in cardiology care with our technological expertise and patient-centered approach. Our comprehensive team diagnoses heart disease and other cardiac conditions, offering personalized treatment plans. Neurological Symptoms: Sudden and severe headaches, seizures or other neurological symptoms may prompt women to visit the ER if symptoms are extremely disorientating or debilitating. These symptoms could be indicative of various conditions from mild to severe, including strokes or neurological disorders that require prompt evaluation. Renown Regional Medical Center is a Comprehensive Stroke Center, providing primary stroke care including evaluation, treatment and education to patients who arrive at a Renown facility with the signs and symptoms of a stroke. Compassionate Care in Times of Need At Renown Health, we understand that your time is valuable, especially in emergency situations. That's why we strive to provide patients with exceptional care, compassion and respect. Plan ahead and make informed decisions about seeking medical care by viewing your estimated triage wait time at a Renown ER.
-
Understanding the Reasons Behind Heavy Menstrual Cycles
While menstrual cycles can be an annoying inconvenience for many women, heavy bleeding (menorrhagia) is not normal and can disrupt your life. A few days of heavy flow at the start of your period is usually nothing to worry about. However, if you’re frequently experiencing very heavy periods, you should discuss it with your gynecologist or primary care provider. Dr. Megan Fish, an OB-GYN with Renown Women’s Health, discusses various reasons, evaluation and treatment methods when it comes to heavy menstrual cycles. What is classified as heavy menstrual bleeding? The American College of Obstetricians and Gynecologists considers heavy bleeding to be any of the following signs: Bleeding that lasts more than 7 days. Bleeding that soaks through one or more tampons or pads every hour for several hours in a row. Needing to wear more than one pad at a time to control menstrual flow. Needing to change pads or tampons during the night. Menstrual flow with blood clots that are as big as a quarter or larger. What are the most common reasons for heavier periods? A variety of reasons why someone might have heavy periods. Fortunately, most of these problems are treatable. Because each woman's period is unique, only a doctor can definitively determine the cause of your heavy periods. Some of the most common issues that cause heavy periods include: Hormone imbalances such as anovulation, thyroid disease and Polycystic Ovary Syndrome (PCOS). Structural abnormalities in your uterus such as polyps or fibroids. Precancer and cancer such as uterine, cervical, vaginal, ovarian or endometrial hyperplasia. Infections such as chlamydia, gonorrhea, endometritis or vaginitis. Other medical conditions such as liver disease, kidney disease or Pelvic Inflammatory Disease. Medications such as blood thinners and aspirin, hormone replacement therapy, Intrauterine devices (IUDs), birth control pills and injectables. Pregnancy-related problems such as a miscarriage or ectopic pregnancy.
Read More About Understanding the Reasons Behind Heavy Menstrual Cycles
-
What to Expect at a Renown Health ER
Access to a trusted and efficient emergency room (ER) in times of unexpected medical emergencies is crucial. Renown Health’s emergency and trauma care is available at three ER locations, including the region’s only level II trauma center and ER designed for pediatric patients to provide you and your family with prompt, high-quality and specialized care by board-certified emergency physicians when you need it. Dr. John Hardwick, board-certified emergency physician at Renown Health, describes a guide to emergency care at Renown Health below. Timely and Compassionate Care: Renown ER is committed to delivering timely and compassionate care. Experienced medical professionals at Renown will communicate openly with you, involving you in the decision-making process and addressing any concerns you may have. Upon arrival, you can expect to be promptly assessed by a team of skilled medical professionals who will prioritize your needs based on the severity of your illness or condition. Click here to learn more about the emergency care process, from check-in to discharge. Expert Medical Team: With advanced technology and experienced specialists from Northern Nevada Emergency Physicians, all patients are in good hands for emergency care at Renown Health. Our pediatric and adult emergency physicians have completed fellowship training in specialty areas such as sports medicine, ultrasound and emergency medical services. Team members in the emergency department will ensure you are informed and as comfortable as possible during your visit to minimize any pain or discomfort you may feel. Efficient Triage Process: Renown ER utilizes an efficient triage process to prioritize patients based on the urgency of their medical condition. This ensures that those with more critical conditions receive immediate attention, while still providing timely care for others. Tests such as labs or diagnostic services will often be completed while you wait to see a physician to expedite the process. Comprehensive Diagnostic Services: The ERs at Renown offer comprehensive diagnostic services to quickly identify your symptoms. This may include X-rays, laboratory tests, CT scans and other imaging studies, helping emergency physicians make informed decisions about your treatment plan. Specialty Care and Collaboration with the Renown Health Network: We offer the area's largest network of specialized providers and services to help ensure you receive industry-leading, personalized care during and after your emergency room visit. This collaboration means you’ll have access to more specialists and a wide range of expertise to continue your care without leaving the Renown Health network. State-of-the-Art Facilities: Renown Health invests in state-of-the-art facilities and equipment to ensure that patients receive the best possible care. Renown ERs are equipped with modern medical technology, allowing board-certified emergency physicians to diagnose and treat a wide range of medical conditions. Post-ER Visit Support and Resources: Your experience with Renown Health doesn't end when you leave the ER. Our team will address your questions and provide you with post-visit instructions, medications and follow-up recommendations to continue your care. With a commitment to timely and compassionate care and a team of expert healthcare professionals, you can trust Renown ER to provide the highest standard of emergency medical services when you need it most.
-
6 Healthcare Action Items for the LGBTQIA+ Community
Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
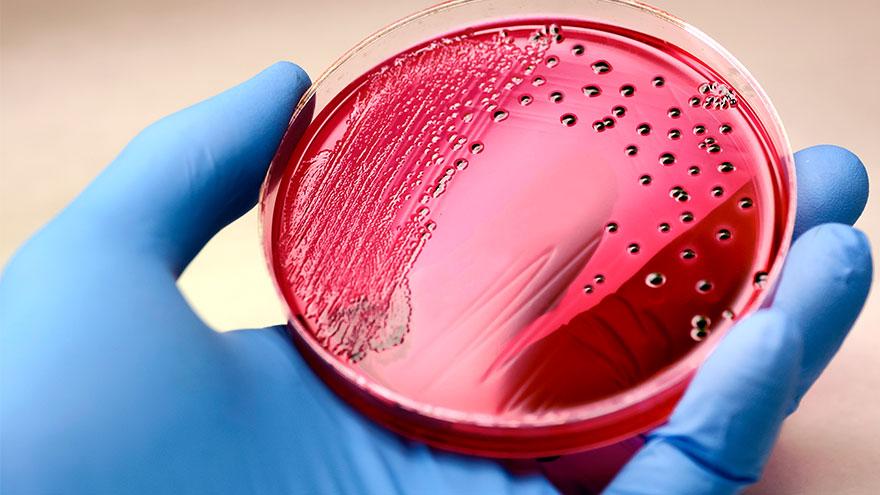
Sepsis: Causes & Symptoms
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Head Injuries, Sprains and Broken Bones
Participating in sports and physical activities is enjoyable and beneficial for our health. However, the risk of injuries comes with the fun and excitement of sports. Sports-related injuries, including sprains, traumatic brain injuries and broken bones, are more common than we realize and can land you in the emergency room. Dr. Scott Shepherd, Emergency Medicine Physician, provides a wealth of information. Traumatic Brain Injuries: The Invisible Threat Traumatic brain injuries come in many forms. From “mild” brain injuries, concussions, to major brain injuries and bleeds. Sometimes it is very difficult to tell the difference between a major injury and a minor injury because many of the symptoms are the same. Concussions Concussions are a type of “mild” traumatic brain injury resulting from a blow to the head or a violent shaking of the body that causes a transient alteration in mental function. They are particularly prevalent in contact sports such as football, soccer and boxing. A concussion can affect memory, judgment, reflexes, speech, balance and muscle coordination. Typically, concussions are not life threatening and usually short lived. However, multiple concussions can lead to permanent disabilities. So, remember there is nothing “mild” about injuring your brain. Contusions The more serious brain injuries from brain contusions (actual bleeding in the brain material) and bleeding that presses on the brain are life threatening. These injuries are caused by the same blow to the head as a concussion and the symptoms are the same from memory deficits, loss of coordination to coma. Because of this, anyone who has a blow to the head and is not acting normal should be evaluated by a medical professional. Anyone suspected of having a severe head injury should seek immediate medical attention and follow a strict protocol for rest and a gradual return to play. It is important to note a person may not lose consciousness if they suffer a concussion; however, major consequences can occur if not properly managed. If you suspect you have an emergency that needs immediate medical attention, please call 911 or visit an emergency room near you. While it is impossible to prevent traumatic brain injuries altogether, the severity of the injury can be mitigated through proper helmet usage and knowing your skill level when participating in high-risk activities. The guidelines for picking a helmet for summer activities such as mountain biking, dirt biking and riding off highway vehicles are similar to those of picking a helmet for winter sports. Learn more about choosing the right helmet. Any blow to your head, neck or upper body can result in a major head injury Signs to watch for include the following: Headache Dizziness Blurred vision Difficulty with thinking, attention or memory Sensitivity to noise or light Ringing in the ears Changes in hearing Double vision Changes in behavior Balance issues Nausea/vomiting Sprains: The Annoying Twist One of the most common sports injuries is a sprain, which occurs when ligaments that connect bones are stretched or torn. Sprains typically occur in joints, such as the ankle, knee or wrist, and are often caused by sudden twists or impacts. Symptoms may include: Pain Swelling Bruising Limited range of motion Rest, ice, compression and elevation (RICE) are the initial recommended treatment, followed by physical therapy to regain strength and mobility.
-
What it Means to be a Level II Trauma Center
When the sudden need for emergency or critical care arises, the level of a trauma center is an important designation that helps explain the types of resources available. Renown Regional Medical Center is proud to be the only Level II Trauma Center in our region, which is a critical service to provide. We spoke with Bret Frey, MD, an emergency care physician, to discuss what this means for our community. Requirements for Designation as a Level II Trauma Center To be a designated Level II Trauma Center, a hospital must have 24-hour immediate coverage by general surgeons and multiple specialties, such as orthopedic surgery, neurosurgery, emergency medicine and more. In addition, this hospital must provide trauma prevention and ongoing education for its teams and incorporate a comprehensive quality assessment program. “What it means for this community is nothing short of amazing,” said Dr. Frey, who explained that Renown has over 20 specialty physicians on-call and ready to provide trauma care. According to Dr. Frey, many communities of the same or larger size have fewer specialists ready and available to provide this level of care. Renown Regional Medical Center is located near downtown Reno. The Emergency Department has several helipads and ambulance banks to intake patients requiring emergency care. Patients can also receive emergency walk-in care. On the same campus is Renown Children’s Hospital, which is home to the only pediatric Emergency Room dedicated solely to pediatric patients. Emergency and trauma care is just one area in which Renown Health is the regional leader. When patients or families choose Renown during an emergency, they will have access to all the resources provided through the entire health network. This means access to the many specialists available to consult on different conditions or care situations, inpatient care if needed, referrals to other areas of the network and medications to go. “I’m very happy and proud to be a part of building something very special in this community,” said Frey.
Read More About What it Means to be a Level II Trauma Center
-
What to do if you Experience a Summer Burn
As families spend more time outdoors to enjoy the summer temperatures, it's important to be aware of potential hazards that can lead to burns – be it sunburns, burns sustained while grilling or navigating the hot surfaces often found around pool decks and parks. All these burn types are not only painful but can also cause severe damage to the skin and require immediate medical attention. Ross Albright, MD, an emergency care physician, explores effective preventive measures to avoid burns during the summer and discusses when it's essential to seek medical care. Stay Sun Safe While soaking up the sun is a favorite summer pastime for many, it's important to protect your skin from harmful ultraviolet (UV) rays. Sunburns not only damage the skin but also increase the risk of more severe burns. Follow these tips for staying safe in the sun: Apply broad-spectrum sunscreen with a minimum SPF of 30 before heading outdoors and reapply every two hours. Seek shade during peak hours of sun intensity, typically between 10 a.m. and 4 p.m. Wear protective clothing, such as wide-brimmed hats, sunglasses and lightweight, long-sleeved garments. Fire and Hot Object Safety Summer is full of fun outdoor activities like BBQs, campfires and fireworks, all of which can pose a fire hazard if not handled carefully. To prevent burns caused by fires: Maintain a safe distance from open flames and grills and always use oven mitts or potholders when handling hot objects. Keep a fire extinguisher and a first aid kit readily available. Keep children away from hot objects and fireworks and educate them about the dangers of touching or playing with them. Hot Surface Safety Asphalt, metal slides and surfaces around the pool retain heat and are likely to be significantly hotter than other materials such as a wooden picnic table to grassy pathway (these can still be hot too!). So, it's crucial to be cautious around these materials to prevent burns: Use caution when near hot surfaces surrounding water sources, such as pool decks or metal slides. Always wear shoes when walking on hot surfaces such as asphalt, concrete and even sand. Ensure that playground equipment such as slides and swings are cool to the touch before your kiddos start climbing around. Recognizing Severity of Burns and Seeking Care Despite our best efforts, burns can still occur. It's essential to know when a burn requires medical attention: First-degree burns, characterized by redness, pain and minor swelling, can typically be treated at home with cool water and over-the-counter pain relievers such as ibuprofen (Advil or Motrin) or acetaminophen (Tylenol). Second-degree burns, which may cause blistering and more intense pain, should be evaluated by a healthcare professional. Third-degree burns, indicated by charring or blackened skin, deep tissue damage or burns that cover a large area, require immediate emergency care. Preventing burns during the summer is paramount to enjoying a safe and enjoyable season. By following these tips, you can significantly reduce the risk of burns and ensure prompt medical attention when necessary. Stay informed, stay safe and have a burn-free summer! If you or someone you know experiences a burn, it's important to seek immediate medical care.
-
When to Seek Care for Abdominal Pain
Abdominal pain is one of the most common complaints that brings individuals to the emergency room. We spoke with emergency physician Bret Frey, MD, to ask about when and where to seek care for abdominal pain. Dr. Frey advises that any time you feel something is developing inside your body that is substantially different from what is normal for you, understand that something is wrong. He further explains that warning signs of an acute medical situation include fever, vomiting or a rapid change in function and ability to move due to pain. These symptoms indicate that one needs to be evaluated by a medical professional. This evaluation will include the care team conducting an examination and asking a series of questions to determine if additional diagnostics, such as lab work or imaging, are needed. Be prepared to discuss where the pain is and what it feels like, in addition to how long it’s been bothering you and if it’s constant or intermittent. While appendicitis often comes to mind when thinking about abdominal pain, Dr. Frey says that this is not the bulk of cases that the Emergency Department sees. In fact, often the pain does not have a specific diagnosis, but our team of board-certified emergency physicians are experienced in assessing and caring for those experiencing the acute symptoms he described. “We often don’t come away with an answer about exactly what it is, but we substantially rule out life threats in a very methodical and systematic way,” said Frey. The abdomen includes many organs, including the stomach, liver, small and large intestines, gallbladder and pancreas. In addition, pain stemming from your chest, pelvis or back may be felt in the abdominal area. If you are experiencing abdominal issues that are persistent but not an emergency, talk to your primary care doctor about what you are experiencing, and be prepared to review the history of this pain, medications, allergies and diet. He or she will be a good partner to review conditions such as gas, heartburn, constipation, diarrhea, inflammation or menstrual and ovulation pain. Drinking plenty of water is always an important part of supporting your health.









.jpg?rev=f89fdc95b1824f868e98988928b0a6bb)
