Buscar
-
What is Polycystic Ovary Syndrome (PCOS)?
Dr. Carilyn Hoffman with Renown's Women's Health explains the symptoms, causes and treatments of Polycystic Ovary Syndrome (PCOS) (also referred to as Polycystic Ovarian Disease (PCOD)), a prevalent condition among women of reproductive age that influences hormonal balance, metabolism and fertility. Make an appointment with Renown Women's Health Click here to schedule Call to schedule: 775-982-5000 PCOS Defined PCOS is a constellation of symptoms characterized by two of the three criteria: multiple small cysts on the ovaries visible via ultrasound, irregular periods and signs of hyperandrogenism. Other symptoms include infertility, insulin resistance, and increased risk of cardiovascular disease. Symptoms of PCOS The symptoms of PCOS can vary from woman to woman, but some of the most common include: Irregular menstrual cycles: This is often one of the first signs of PCOS. Women may experience fewer than nine periods a year, more than 35 days between periods, frequent spotting, and/or abnormally heavy periods. Excess androgen levels: High levels of male hormones may result in physical signs such as excess facial and body hair (hirsutism), severe acne and male-pattern baldness. Polycystic ovaries: Enlarged ovaries containing numerous small cysts can be detected via ultrasound. Causes and Risk Factors The exact cause of PCOS is unknown, but several factors may play a role: Genetic predisposition: A family history of PCOS increases the risk. Insulin resistance: High insulin levels might increase androgen production, causing difficulty with ovulation. Obesity: Women with elevated BMI’s are more likely to have PCOS, although 20% of women with PCOS are not obese. Diagnosis and Treatment Dr. Hoffman outlines that diagnosing PCOS requires a medical history review, a physical exam, blood work and an ultrasound to evaluate the ovaries. Treatment options can range from lifestyle modifications, like diet and exercise and weight loss, to medications for menstrual regulation, fertility assistance, and rarely surgery. Lifestyle Changes A healthy lifestyle is a cornerstone of managing PCOS. Regular exercise, a nutritious diet, and weight management can help reduce symptoms and the risk of long-term health issues. In overweight patients, weight loss as little as 5% has been shown to improve symptoms of PCOS. Medication Medications may include hormonal contraceptives to regulate menstrual cycles, anti-androgens to reduce hair growth and acne, and Metformin to address insulin resistance. Fertility Treatment For women with PCOS who are trying to conceive, ovulation induction with clomiphene or letrozole is sometimes necessary. Sometimes a referral to a reproductive endocrinologist and infertility specialist is needed for more advanced technologies like IVF. Health Implications PCOS is not just about cystic ovaries or irregular periods; it can have profound implications on a woman's overall health. Women with PCOS are at an increased risk for several conditions, including type 2 diabetes, high blood pressure, heart disease, and endometrial cancer.
-
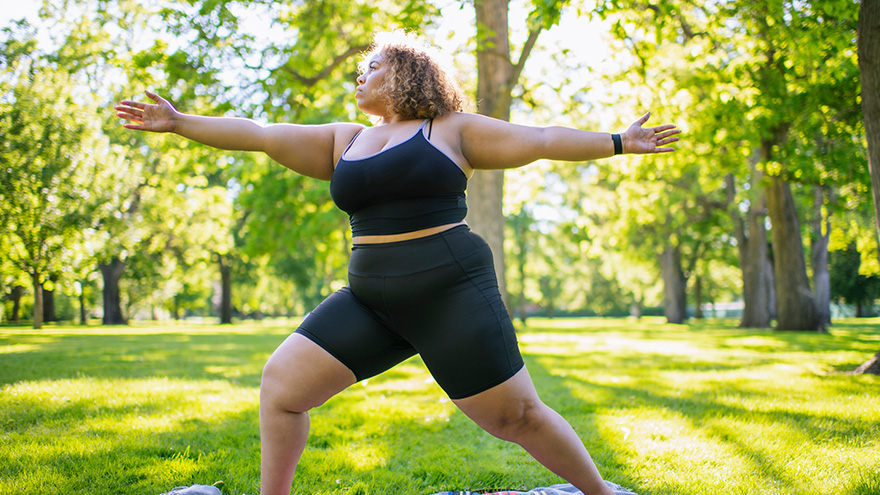
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Sepsis: Causes & Symptoms
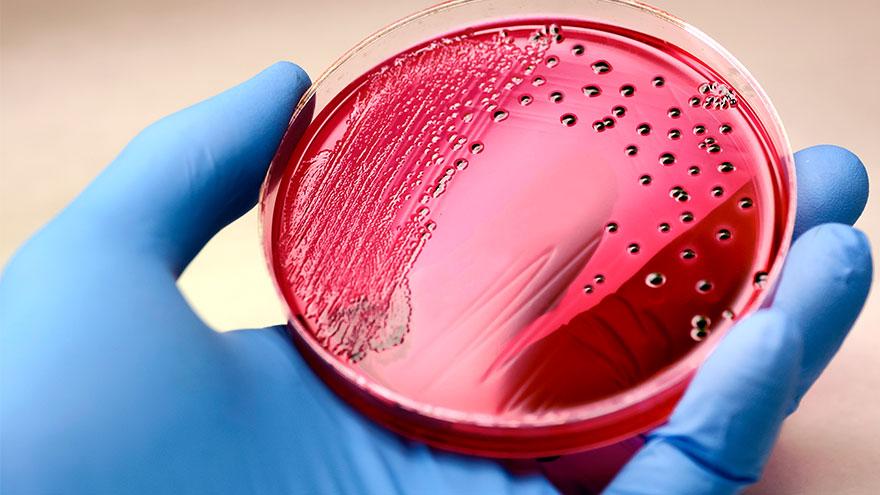
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Importance of Safe Sleep
In today's fast-paced society, it is understandable for parents to want to take shortcuts in caring for their little ones. A s a result, It is tempting to leave a sleeping infant in a car seat or swing after a long day of errands or when you need a moment to catch your breath. But, as convenient as these devices may be, they pose a serious risk to your child's safety. Why Car Seats and Swings Pose Risks for Infant Sleep Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The American Academy of Pediatrics (AAP) states that “infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical.” If a parent must use a car seat or other sitting device, they should only do so for a short period of time and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The American Academy of Pediatrics (AAP) warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. This is because infants can easily slump over or become entangled in the straps, blocking their airway, and causing suffocation. Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The AAP states: Infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical. If a parent must use a car seat or other sitting device, they should only do so for a short period and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The AAP warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. In addition, infants can easily slump over or become entangled in the straps, blocking their airways and causing suffocation.
-
What Does a Doula Do?
If you’re expecting a new baby, you may have been given the advice to hire a doula. You may have seen statistics of improved outcomes among those who’ve had a doula attend their birth. Perhaps you’ve heard that the etymology is from the Greek word meaning “to serve.” But how does a doula serve their clients? A doula is a non-medical birth professional who will guide you through labor, birth, postpartum and beyond. Your doula can discuss your options with you so you can make informed decisions, as well as provide emotional and physical support to ease your experience. While each doula offers their own style, there are certain services that most doulas will provide for their clients. Typically, a birth doula will provide at least one prenatal visit, one postpartum visit and continuous support during active labor. A postpartum doula usually provides support during the 12 weeks immediately following birth, sometimes referred to as the “fourth trimester,” but some will continue care after that as well. Simply put, a doula provides informational, physical and emotional support during the childbearing year(s). Let’s take a closer look at these three ways a doula can support you. The Basics If you don’t know your options, you don’t have any. This is a common phrase in the world of birth work. When you’re in labor, you’re exhausted, in pain and there’s often urgency inherent or implied in any choices you make. So, when an intervention is offered, many birthing people accept it without question. One method that can help the decision-making process is to check your BRAIN: Benefits: What are the benefits of the proposed intervention? Risks: What are the risks of the proposed intervention? Alternatives: What are the alternative options? Intuition: What does your intuition tell you? Nothing: What if we do nothing? What if we wait? When you’re in active labor, you might have difficulty remembering this acronym; that’s where your doula comes in. At your prenatal visits, you can ask your doula for guidance in preparing your birth plan, which can include contingencies for certain potential interventions. And as choices arise during labor, your doula can guide you through the benefits and risks and can provide you with alternative options you might not otherwise be aware of that are available to you. Your doula can remind you to check in with your intuition and can help you quiet your mind so you can listen to your instincts. The Body Although we tend to see depictions of people giving birth on their backs with their feet in stirrups, this is only one of many ways to give birth. Walking and dancing can speed up early labor. Side-lying or hands-and-knees can prevent tearing during the pushing stage. Sometimes labor stalls, and a change of position is often helpful to get things moving again. Your doula can suggest positions depending on your stage of labor. Some labor positions might require the support of another person – your doula could fill this role or assist your partner in doing so. Some doulas also provide massage or even acupressure, and most will do the “hip squeeze” that so many laboring people swear by. If your baby is presenting posterior, or “sunny side up,” your doula can apply counter pressure to alleviate back pain during labor. Some postpartum doulas will do light housework while you rest and bond with your newborn. Others might care for your baby through the night so you can catch up on sleep. Many doulas have also gone through additional training to offer breastfeeding support and may be able to assist you with latch issues and nursing positions. The Mind Pregnancy, birth and postpartum periods can be some of the most emotional times in a person’s life. A doula will hold space for you and help you process your emotions before and after birth. It’s normal to feel apprehensive, or even fearful, about labor and birth, and discussing these feelings is the first step. A doula can help you navigate your concerns in a safe space so you can be prepared emotionally for your upcoming labor. Many doulas will also guide you through writing your birth plan, which can lessen anxiety about the unknown. If you have a history of trauma, your doula can assist in communicating this, so you don’t have to relive the experience every time you meet a new medical provider. Most people will experience some form of what’s often called the Baby Blues in the immediate postpartum period. The third day after birth tends to hit hard, as hormones attempt to regulate, but the Baby Blues can continue for weeks for some new parents. A postpartum doula’s support can be incredibly valuable during this time. When the baby blues last longer than a few weeks, it could considered a mood disorder. Most doulas will recognize signs of postpartum mood disorders and will have resources available for additional support. Choosing the Best Doula for You With so many wonderful doulas in northern Nevada, you might wonder how you could ever choose just one to attend your birth. Some expectant parents are unfortunately restricted by cost. With so many expenses related to a new baby, it can be difficult to budget doula services as well. Thankfully, Nevada Medicaid now covers doula care, and some commercial insurances are following suit. Check with your insurance company to find out if they might cover part of the cost for hiring a doula. If your insurance doesn’t cover doula services, some doulas offer a sliding scale based on income. You may want to interview multiple doulas to find the right one for you. If you’re the kind of person who wants all the information you can get, a more detail-oriented doula might be the best choice. But if you tend to feel overwhelmed by too many options, you might prefer a doula who only offers additional information as the situation calls for it. If you want massage or acupressure during labor, you might want to hire a doula with those certifications. Or maybe informational and physical support are not as important to you as emotional support, in which case your best choice could be a doula who has experience with postpartum mood disorders or trauma support. Regardless of who you hire, be sure to clearly communicate your desires and expectations – not just for your birth, but also for your doula. The most important thing when choosing your doula is trusting your gut. You need to feel comfortable with your doula, as they’ll be tending to you at one of the most vulnerable times in your life. When you find a doula that you click with, who listens to you and supports your choices, you have found the best doula for you.
-
What to Expect at a Well Child Checkup
A well-child checkup is a great opportunity to monitor your child’s growth and development, and it's also a chance to establish a trusting relationship with your child’s pediatrician and have your questions answered. What to Expect at Each Checkup At every checkup, a comprehensive physical examination will be conducted to assess your child's growth parameters, including height, weight and head circumference. A developmental assessment will evaluate the progress of your infant or young child in achieving age-appropriate milestones, encompassing language skills, motor development, problem-solving abilities and psycho-social skills. In addition, your pediatrician will address common concerns such as feeding, sleep patterns, oral health and general infant care. Unless there are specific needs or concerns for your baby, routine laboratory tests are typically unnecessary. Your pediatrician will provide guidance on immunization schedules, post-vaccination expectations and when to seek medical attention. Furthermore, during each visit, you will receive age-specific guidance to help you anticipate your child's expected growth and development, along with essential safety precautions and illness prevention measures. Your pediatrician will discuss various topics, such as placing your baby to sleep on their back, utilizing rear-facing infant car seats until around age two, maintaining home water thermostats below 120 degrees Fahrenheit, ensuring dangerous objects and poisonous substances are out of sight and reach, emphasizing dental health and promoting the use of bike helmets, among other things. Preparing for Your Visit It is recommended that, as a parent, you write down any questions beforehand, so you don’t forget them in the moment. Most importantly, feel comfortable asking your pediatrician about anything that might seem unusual, as you are the parent, and you know best! Before leaving the pediatrician’s office, be sure that you fully understand any instructions given to you and ask for clarification if needed. From your child’s birth through young adulthood, you will be visiting your pediatrician regularly. The American Academy of Pediatrics provides what a regular schedule might look like. Well-Child Checkup Schedule Two to three days after birth and at one month Two months Four months Six months Nine months One year 15 months 18 months 24 months 30 months Three years, and yearly after
-
10 Essential Questions to Ask at Your Child's Pediatrician Visit
Taking a few minutes to prepare for your child's pediatrician visit helps ensure that all your child's medical needs are met. Knowing the right questions to ask your provider can help you get the most out of your visit and ensure you and your child feel comfortable and informed. It is essential to base your questions on your child's specific health needs, but the ten options below are a great place to start. How is my child's overall health and development progressing? Is my child meeting their developmental milestones, and are there any areas where they may need extra support? What vaccinations does my child need, and are they up to date on all required immunizations? Are there any nutritional recommendations or concerns for my child's age and stage of development? What are some strategies for promoting healthy habits and physical activity for my child? Are there any warning signs I should look out for regarding my child's health or behavior? What can I do to help prevent common childhood illnesses like colds, flu strains or ear infections? What should I do if my child gets sick, and when should I seek medical attention? Are there any changes to my child's medication or dosage that I should be aware of? Is there anything else I should know or be aware of regarding my child's health or development?
Read More About 10 Essential Questions to Ask at Your Child's Pediatrician Visit
-
A Fighting Chance at 24 Weeks Sloans Story
Most babies weigh just one pound and are roughly the size of an eggplant when they reach 24 weeks of development inside the womb. It is a crucial stage when internal organs begin functioning, and the babies' respiratory and central nervous systems are still developing. So, in November 2021 when Kallie Johnson experienced a premature rupture of amniotic fluid around this point in her pregnancy, her care team in Winnemucca decided to transport her via Care Flight to Renown Regional Medical Center. The team at Renown Children’s Hospital immediately began discussing the risks of delivering at 24 weeks with the Johnson family. Moving Forward with Hope Knowing the stakes, Kallie remembers never feeling rushed to decide about delivering her baby preterm. “I felt educated and supported by my care team at Renown throughout our entire stay, starting with the education they provided about what it meant to deliver my baby early,” Kallie said. “The team really helped me make the best decision for myself and my family.” Together, Renown employees and the Johnson family moved forward with a healthy set of nerves and a powerful feeling of hope. Weighing in at one pound 11 ounces, Sloan entered the world on Nov. 19, 2021, via emergency Cesarean section. Her birth was classified as a micro preemie because she was born before week 26 of pregnancy and so small that she fit inside the palm of her father Sterling’s hand. A full-term pregnancy is classified as reaching 39 weeks. A Fighting Chance Called a fighter by many Renown Children’s Hospital care team members, Sloan spent over five months in the neonatal intensive care unit (NICU). She was placed on a ventilator, fed through a feeding tube and monitored 24/7, overcoming daily challenges with the Renown team and her family. As a result of being born prematurely, Sloan developed a grade one brain bleed and a congenital heart defect called patent ductus arteriosus, a persistent opening between two major blood vessels, causing too much blood to flow to the lungs and heart. To meet the oxygen needs of her tiny lungs, Sloan was intubated and developed a severe oral aversion and high-arched palate as a result. The effects would lead to difficult developmental and physical challenges that she still conquers today. Yet, with the help of her care team – including physical, occupational and speech therapists, dieticians and doctors – Sloan continues to make progress every day.
-
Departamento destacado: NICU Transport
Bringing in new life is an exciting and beautiful occasion. The possibilities for the newest members of our world are endless – what will the child grow up to become? What will they achieve in their lifetime? Anyone will agree that a new life is precious and protecting that life by any means possible is a necessity. Sometimes, however, a baby’s journey into our world brings along obstacles. Prematurity, congenital defects and other complications can accompany a birth and the baby’s first few moments of life. But what happens when these complications happen outside of a fully-functioning Labor & Delivery unit, or if the complications need a special level of intervention with a health system capable of caring for their unique needs? Enter the NICU Transport team at Renown Health. As the only Neonatal Intensive Care Unit (NICU) Transport team in northern Nevada, these dedicated nurses, respiratory therapists and neonatal nurse practitioners – who have normal unit duties of their own at Renown Regional Medical Center – step up to the plate to take on this extra duty to support members of their community facing some of the scariest moments of their lives. To them, transporting babies in critical condition and giving them the best chance of life isn’t just a responsibility; it’s a calling. The NICU on Wheels When the Saint Mary’s maternity unit, which was Renown’s partner in NICU transport duties, made the decision to close, our dedicated NICU nurses and respiratory therapists diligently rose to the occasion to fill the demand. Dubbed the “NICU on Wheels,” Renown’s team went from taking on transport duties every other day to 365 days a year – and they are always ready to go at a moment’s notice, whether it’s by ambulance or by fixed-wing aircraft. “When we learned about the closure we knew it was our calling and knew we had to step up,” said Rachel D., Neonatal Transport RN at Renown. “We still have regular days on the floor, and we each switch off being on-call for transport. Once we get a distress call, we have 30 minutes to get to the hospital, grab our gear and go. We have to essentially put a whole room’s worth of portable equipment in one bag.” “I really enjoy being a part of the transport team and making a difference from northern Nevada to northern California,” added Sam V., Supervisor of Respiratory Care at Renown. “We are able to practice at the top of our skill level and use autonomy that not every practitioner gets to use.” Each NICU Transport unit works in teams of three when heading out into the field: one nurse (our bedside experts), one nurse practitioner (our education experts) and one respiratory therapist (our lung and breathing experts). With several years – and in many cases, decades – of experience in NICU nursing, NICU transport duties and respiratory therapy, this team is poised to provide state-of-the-art lifesaving care en route to the hospital. This diverse array of experiences among the team especially comes in handy as they continue to face the increased transport workload. “We are so thankful to have Saint Mary’s employees come over and work on our team after their maternity ward closed,” said Melyssa H., RN, NICU Transport Coordinator at Renown. “Helping the babies, as well as helping the scared families, will always be our top priority.” “I love the complexity that babies provide in the NICU,” added Jennifer J., Neonatal Transport RN at Renown. “Providing hands-on care right at the bedside along other members of the team is such a rewarding experience.” Education is also a crucial tool in NICU care, especially in the field. The nurse practitioners on this team make it their mission to outreach to the community, including our rural health partners, and help them build the tools and skills they need to care for our smallest and most critical patients. “I have been on a few transports where we went out and did not have to bring the baby over to the hospital, and we were able to provide lots of education instead,” said Shiela A., Respiratory Specialist at Renown. “For instance, I was called out to Fallon for a baby that was in respiratory distress. When we arrived, we saw the baby was awake and active although intubated. The tube came out, and we retaped it. While we stayed to observe the baby to make sure everything was okay, the nurse practitioner on the team provided educational tools to the family on what they can improve on regarding their baby’s tubing. Our nurses do such a great job with these teachings.” “When I started, I quickly noticed that more education was needed in the field,” added Jennifer J., RN. “Now I see the momentum we’ve had in these communities really take full force. Because of this education, and the confidence we instill in our patients’ families, each baby’s transition to our team has become so much easier. It has been awesome to watch this progress over the years.” With immense experience, education and a strong commitment to their community under their wing, the NICU on Wheels is only just getting started. Teamwork Makes the Dream Work Running a successful NICU Transport operation, especially as the sole health system participating, takes a village. With only three professionals out in the field, the team leans on their fellow nurses, physicians, surgeons and specialists to make the operation run as smoothly as possible. From REMSA and Care Flight helping load patients in and get them to the hospital safely, to Renown’s Clinical Engineering team who are first on the scene when machines need repairs and troubleshooting, everyone rises to the occasion to achieve the best-possible outcome for our youngest patients at some of the most challenging moments of the beginning of their lives – and they are fully trusted to move those mountains. “Being a part of the NICU Transport team has given us the opportunity to facilitate a deeper, meaningful relationship with providers and a patient’s entire care team,” said Rachel D., RN. “They entrust us with our assessment skills, opinions and skill levels. There is an equal layer of trust between us and them.” Despite the pressure they feel every day, the NICU Transport team never let it overtake them and instead let it empower them. “We are under a lot of pressure and stress regardless of the case, and yet, we all work so well together; the teamwork really is incredible,” said Lisa A., Respiratory Specialist at Renown. “I am very proud of how our team steps up and is very intricate, even down to organization. For example, team members like Shiela arrange all the respiratory bags and make sure they are laid out in a way that makes the procedure as simple as possible to ensure there are no complications.” The nurses and respiratory therapists also partner together on the NICU floor and are always ready to provide coverage when their transport colleagues get a call. Committed to collaboration and ready to jump into action, the NICU Transport team works together to elevate each other and the bottom line for each patient. “This is a full-time gig, and the group works together to make sure everyone is covered; we are all very collaborative,” said Sarah K., Respiratory Specialist at Renown. “We all think of our patients as extra special, and it’s nice to know that you can make a difference in the baby’s life and the lives of the family. We all have a sense of purpose in giving back to the community.” “I am just so thankful to be a part of this team,” added Marcia A., Neonatal Transport RN at Renown. “We really have developed a strong bond.” A Track Record of Success The life-saving measures that each member of the NICU Transport team take surpass hospital walls. The impact they have on each baby are remembered and celebrated for years, and they often develop lifelong relationships with patients and their families after their stay in the NICU. One prime example of this can be found in an impassioned letter from Tess, the mother of a young boy who was in the midst of respiratory distress and needed immediate intervention. Because of the valiant efforts of Renown’s NICU Transport team, her child, Warren, is a healthy and happy baby to this day. She recalls the experience: Warren had stopped breathing while getting routine blood work. He was resuscitated twice while at an area hospital. We made the decision to transfer him to Renown for him to be admitted into the NICU. Within an hour and a half of this decision, Renown had sent a team consisting of a respiratory therapist, nurse and nurse practitioner to come and get him. As soon as the team entered the room, we immediately felt safe and comforted. The team made sure we knew exactly what was going on and what was going to happen in the following hours, and they let us know they would do everything for Warren. He was resuscitated two more times by the respiratory therapist while getting ready for transport. At that time, the decision was made to intubate for a smoother ride to Renown. We knew you all had his best interest in mind, and of course, we trusted you with everything. The intubation went well, and he was packed up and ready to drive. Today, Warren is hitting all of his developmental milestones and is a normal, happy baby in everyone’s eyes. We can’t thank the NICU Transport team enough for taking such good care of Warren and helping him Fight the Good Fight. “This success wasn’t just due to our three-person unit – our manager, Jason, also jumped in and drove all the way to Carson City to stabilize the child,” said Shiela A. “This just goes to show that no matter our title, we are always here to help and make a huge difference in the lives of our patients.” Success stories of children like Warren describe the common mission of the NICU Transport team in detail, and while there are more of these stories to come, the team is always ready to make the necessary sacrifices for the greater good of their patients. “Sarah K. is like Warren’s guardian angel,” said Tess. “We call her ‘Auntie Sarah’ now. He wouldn’t be here if it weren’t for her and the entire NICU Transport team. It takes a special kind of person to work in the NICU. I can never repay this team for what they’ve done for Warren and our family.” “I am proud of this team, their flexibility and the sacrifices they have made to do transport 365 days a year,” added Melyssa H., RN.” The remarkable success of the NICU Transport team serves as proof of the unwavering and tireless commitment of each and every team member, bringing hope to families during their most difficult moments. “NICU Transport forces you to be confident in yourself and your abilities and to push yourself a step further,” said Rachel D., RN. “I am a better nurse because I joined the transport team.”
-
Your Top 5 Questions about TAVR Answered
Your heart is the muscle in charge of pumping blood to your entire body. This vital organ is made up of chambers, valves and blood vessels. Your heart valves work similarly to a one-way door: they open and close, controlling blood flow in the correct direction through the heart chambers. For patients who have been diagnosed with a heart-related condition like aortic valve stenosis (narrowing), it is important to know treatment options. Most might think open-heart surgery is the only way to treat a heart valve, but many hospitals, including Renown, also offer a minimally invasive procedure called a Transcatheter Aortic Valve Replacement (TAVR). Dr. Abhilash Akinapelli of Renown Institute for Heart & Vascular Health shares his answers to the top five TAVR questions: 1. What causes aortic valve stenosis? Aortic valve stenosis can be caused by a variety of factors. The main reasons being wear and tear of the valve due to aging; genetically abnormal heart valve (bicuspid aortic valve); long-standing high blood pressure; and other reasons like radiation exposure. 2. Am I a candidate for TAVR? Renown’s heart care teams are made up of your primary care provider, cardiologist and cardio thoracic surgeon. They will evaluate if patients are a good candidate for the TAVR procedure by performing a variety of screenings and tests. Some of these include: Echocardiogram Electrocardiogram (ECG or EKG) Chest X-ray Exercise tests or stress tests Cardiac computerized tomography (CT) scan Cardiac catheterization 3. What are the advantages of the TAVR procedure? The Transcatheter Aortic Valve Replacement (TAVR) procedure is much less invasive than open heart surgery, otherwise known as a Surgical Aortic Valve Replacement (SAVR). Patients can typically return to their normal lifestyles within a week after leaving the hospital. During the TAVR procedure, a stent valve mounted on a balloon is advanced to the heart through the blood vessels in the groin without any incision. Once in position, the balloon will be inflated to firmly expand the new valve inside the diseased old valve, pushing it away to the sides. Once the new valve is in place, it begins working immediately and the deflated balloon is removed. The surgical procedure is approximately one hour long. Patients can get up and walk after four hours and will be discharged the following day if no complications arise. Compared to a SAVR, recovery time is much shorter and less risky for patients above the age of 75. A big advantage for anyone who fits under the criteria for a TAVR. 4. Is the procedure painful? The TAVR procedure is not surgery, but you will still be asleep during the procedure. Since no incision is made, it is essentially a painless procedure. Patients may experience slight discomfort such as aches and pains at the entry site of the catheter. 5. Can I have an MRI and X-rays done after having a TAVR valve? Yes, patients can have MRI scans and X-rays after TAVR. For further questions and information about the TAVR procedure, please consult with your Renown heart care team at 775-982-2452 or through MyChart.
-
Departamento destacado: Surgical Preadmission
Heading into surgery of any kind can bring along feelings of intimidation. With a best-in-class surgery team at Renown Health, patients rest assured that they are in the most capable hands for their entire procedure from start to finish – and while the physical preparation is vital, mental and emotional preparation is equally as important to ensure each patient has a smooth and comfortable experience. The Surgical Preadmission department (a.k.a. “preadmit”) at Renown Regional Medical Center and Renown South Meadows Medical Center is a dynamic and compassionate group of nurses, case managers, chart managers and more who are dedicated to guiding each patient through the surgical process. With extensive knowledge and expertise under their belt, the teams are equipped to make a genuine difference in the health and well-being of all patients, for all surgeries, at all times of the year. Surgery Starting Ground The Surgical Preadmission teams are crucial aspects in the successful outcome of every surgical procedure. Comprised of skilled healthcare professionals, this department is dedicated to providing comprehensive support and care before heading into the pre-operating room. “Our job is to prepare every patient for surgery, make sure all their pre-surgery testing is done, ensure they understand their fasting and medication instructions, have had their questions answered, have a ride home and know what to expect during surgery and after so their recovery can go smoothly and without complications,” said Debra Bennett, RN, Supervisor of Surgical Preadmission at Renown Regional. “Each patient is unique, so each experience is different.” Our preadmit nurses are the masters of communication, directing thorough assessments – including medications, tests and clearances – and addressing any questions or concerns patients may have, never missing the opportunity to inform them of exactly what they will expect in surgery. “I do a complete history on every patient while giving them detailed pre-operating instructions and helping them answer any questions to the best of my ability,” said Nancy Hilts, Surgical Preadmission RN at Renown Regional. “I am proud to be able to help allay their fears and concerns using my 30 years of pre-op experience. I offer an avenue for them to feel comfortable opening up to me.” “We always tell patients that they have great surgeons and a fantastic team that will be watching over them and taking care of them every step of the way,” added Jon Capallupo, Surgical Preadmission RN at Renown South Meadows. “We also give them plenty of educational handouts and video content, in addition to verbal instruction, to ensure they are as prepared as possible.” The nurses then pass the reigns onto the chart managers, who prepare the charts for surgery and ensure all documentation is up-to-date before sending them to the pre-operative team. The expert surgical case managers also step in to prepare a thorough discharge plan, along with reviewing pre-operation orders for status, consent, codes and more. The team does several of these initial visits virtually, and they are looking forward to soon phasing all preadmit case manager preliminary visits into a virtual model. From assisting the pre-op and post-anesthesia care unit (PACU) teams with discharge planning concerns to helping on the outpatient side with anything from oxygen equipment and catheters to transportation issues and those experiencing homelessness, our pre-admit case managers are always up to the challenge. "We are true patient advocates, alleviating concerns and fears along the way,” said Mary Carl, RN, Case Manager at Renown Regional. “Just to name a few things we do on a daily basis, we see our total joint and non-weight bearing patients during their preadmission appointment, so they are aware of the medical equipment they need and if it is covered by insurance; provide education for Aspira catheters and gastrostomy tubes; advocate to ensure tube feeding and dressing changes are set up for hospice and home health patients; and escalate concerns of patient safety to ensure a safe discharge.” In the midst of it all, there is never a dull moment in the preadmit teams. At Renown Regional alone, the preadmit professionals see more than 1,600 patients a month – and each one has a hyper-personalized experience with their very own preadmit team. “Many times, we are the first impression a patient has on our organization; after all, we touch more than 97 percent of patients that are scheduled for surgery, cardiac catheterization lab procedures or interventional radiology,” said Amy Schler, Surgical Preadmission RN at Renown Regional. “We also collaborate with many other departments in the hospital as well, from surgeons and anesthesiologists to case managers and nurse navigators. Our work in preadmit impacts the entire surgical process.” Holding a diverse array of experiences, our preadmit department plays an integral role in our commitment to providing the highest quality of care to every patient. Knowledge is Power Heading into surgery feeling fearful and worried is normal for any patient. However, how would you feel knowing that each individual member on your preadmit team has, on average, 23-25 years of experience in the field? This is the reality for our Surgical Preadmission department – and they put that vast knowledge to great use to bring a sense of calm to patients. “Our team members have worked in various departments within our organization, and they bring a wealth of knowledge that we share with each other, and most importantly, with our patients,” said Amy Schler, RN. “If you have hundreds of years of nursing experience, you can speak not only as a nurse but also as a patient. It allows you to give a more personal perspective on what patients can expect in their recovery. Being able to assess their emotions and provide feedback to our pre-op and PACU teams help the patient have a better experience.” “Many of our nurses have close to 40 years of experience each, and they have an extremely large knowledge base since we see patients from newborn to geriatric and from easy procedures to complex surgeries,” added Debra Bennett, RN. “Another great aspect of our team is the varied nursing backgrounds we all hold – surgery, pre- and post-op, labor and delivery, pediatric intensive care, cardiology, gastroenterology, urology, cardiac cath lab, home health and everything in between. Communication between departments is so important!” All members in this department, regardless of which clinical area they came from, surgical or non-surgical, can easily translate their skills into the work they do in preadmit – and they only continue to grow. “As a surgical preadmission nurse, I have used my years of experience as a nurse in surgical services,” said Terri Delatorre, Surgical Preadmission RN at Renown Regional. “I started as a floor nurse with orthopedics for 12 years, and then I worked with the PACU for 11 years. This has helped me give great understanding and care to our surgical patients.” “Because we have staff with such a vast knowledge base, we can rely on our years of working within our organization to help alleviate fears that the patient may have,” added Amy Schler, RN. We can prepare them for what to expect in pre-op and PACU and educate them on what to expect post-op, including any barriers they may face. For example, mastectomy patients may not realize they will not be able to raise their arms for 7-10 days post-op, and total knee patients have to navigate stairs and housing access. Helping patients think about barriers at home that they may not have thought about helps them prepare prior to surgery, enhances their healing and provides a better surgical experience.” The preadmit team works closely with our best-in-class surgeons and anesthesiologists, continuing to grow their expertise along the way while learning alongside our talented providers. For instance, when it comes to our Renown South Meadows preadmit department, anesthesiologist Nariman Rahimzadeh, MD provides excellent guidance for the entire team on state-of-the-art anesthesiology practices. “I am very proud of the work we do with Dr. Rahimzadeh,” said Lisa Closson, Surgical Preadmission RN at Renown South Meadows. “Together, we ensure patients are safe for both surgery and anesthesia.” Despite the challenges that come their way – whether it be changes to process and workflow to navigating support for patients after they leave the surgery floor – the preadmit team cleverly uses their collective wealth of knowledge to bring hope and comfort to all patients. “Our nurses are such warm, caring and compassionate humans that do their best to ease any fears and anxieties patients may have,” said Debra Bennett, RN. The Pride of Preadmission The pride of our preadmit team lies in their ability to make a positive impact on all patients they serve. To them, their work is not just a job – it's a calling. And they do it all while working together to elevate their team and performance. “Our team is most proud of the quality of care we provide to our patients and our abilities to troubleshoot difficult situations to ensure they have a great surgical experience here at Renown,” said Mary Carl, RN. The entire department supports each other by working collaboratively and relying on each other’s expertise to provide the best possible care for patients. They understand that their success as a team depends on their abilities to support and help each other. “Our team is awesome here at South Meadows,” said Jon Capallupo, RN. “We can turn to each other for support, and we all work very well with each other. I am glad to be a part of this team.” “I am proud of how well all of us in preadmit works with each other every day,” added Lisa Closson, RN. “We try to make patients feel comfortable from the moment they arrive to the time they leave the department.” The pride that our preadmit team expends goes beyond their departmental limits – these team members are also trusted teachers. They work closely with cancer nurse navigators to teach weekly classes for patients who have been newly diagnosed with breast cancer, coupled with lymphedema prevention and education classes. The team also encourages participation in Renown’s free smoking cessation programs to help their patients learn the risks and benefits of quitting smoking. When not serving patients or teaching classes, you can find many of these team members taking charge of multidisciplinary committees within our health system, including breast leadership, gastroenterology leadership, shared governance, infection control and recruitment and retention. On top of it all, this team certainly knows how to celebrate, with several of their members being a part of their own department-wide Celebration Committee, where they gather for retirement parties, baby showers and team get-togethers. Always active and never passing up a challenge, our preadmit department are shining examples of Renown’s Culture Commitments, especially Caring and Collaboration, and the pride in the vital work they do every day is limitless. “I am so happy my position in preadmit opened up for me at a time when I was really feeling challenged in my career,” said Nancy Hilts, RN. “The team that we have here is amazing. I am so grateful and thankful every day for the opportunity. It is an amazing place to work!”
-
Building a Better Birth Team
Giving birth expends as much energy as running a marathon. And just like you would only run a marathon with training beforehand, there are exercises you can do to prepare for birth. But instead of a coach, you'll have your birth team. Your birth team exists to help you navigate pregnancy and labor and support your choices. Let's say you've never put together a birth team before and are wondering where to start. Today we'll go over the three main positions to fill for your birth team's starting lineup. Birthing Person The birthing person is the leader of the team. After all, you can't have a birth team without someone giving birth. This person could be the baby's mother, gestational surrogate, birth parent before adoption, a transgender father or a non-binary parent. If you are not the birthing person, don't presume to know what the ideal labor and birth circumstances should be. And if you are the birthing person, don't allow anyone else to tell you what you want. This is your body and your birth; you are the boss in the birth room. Doula No birth team is complete without a doula, and although doulas have increased in popularity lately, many people still don't know what a doula is. Simply put, a doula is a birth professional – not a medical provider – who offers emotional, physical and informational support during pregnancy, labor and beyond. Most doulas' services include at least one prenatal visit and one postpartum visit, as well as continuous care throughout active labor. Some doulas provide more than one prenatal/postpartum visit, so be sure to ask what is included in their fee. Even if you have a partner who will support you during labor, studies have shown that a doula can significantly increase your likelihood of a positive birth outcome. Even the most supportive partner needs to rest, and a doula can ensure that you still get the care you need while your partner gets a break. Midwife or Obstetrician Finally, you'll want to choose the medical professional who will attend your birth. Many folks choose to give birth with the OB/GYN who does their annual check-ups, but there are many reasons someone might choose a different provider for their birth. The first step to finding the best attending provider for your birth is to decide which model of care aligns closest to your values and goals: the Midwifery Model of Care or the Medical Model of Care. .tg {border-collapse:collapse;border-spacing:0;} .tg td{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; overflow:hidden;padding:10px 5px;word-break:normal;} .tg th{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; font-weight:normal;overflow:hidden;padding:10px 5px;word-break:normal;} .tg .tg-gqvw{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-weight:bold; text-align:left;vertical-align:top} .tg .tg-8vim{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-size:18px; font-weight:bold;text-align:left;vertical-align:top} .tg .tg-qm8j{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;text-align:left; vertical-align:top} .tg {border-collapse:collapse;border-spacing:0;} .tg td{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; overflow:hidden;padding:10px 5px;word-break:normal;} .tg th{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; font-weight:normal;overflow:hidden;padding:10px 5px;word-break:normal;} .tg .tg-gqvw{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-weight:bold; text-align:left;vertical-align:top} .tg .tg-8vim{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-size:18px; font-weight:bold;text-align:left;vertical-align:top} .tg .tg-2rvk{background-color:#ffffff;color:#000000;font-family:Arial, Helvetica, sans-serif !important;text-align:left; vertical-align:top} Midwifery Model of Care Medical Model of Care Philosophy Birth is physiological. Birth is potentially pathological. Interventions Medical interventions can cause more complications, and therefore are only used as needed. Medical interventions should be used, even in non-emergency situations and sometimes as preventative measures. Decisions Birthing person is the key decision maker. Medical professional is the key decision maker. Provider’s Role Providers monitor labor and will intervene or transfer to hospital if needed. Providers assess and control the birthing process.