Buscar
-
How to Spot Depression in Men
Is a man in your life struggling with depression? Many men find it difficult to acknowledge when they need help. Recognize their unique warning signs of depression with insights from psychologist Dr. Herbert Coard. Over 6 million men are diagnosed annually, often displaying symptoms like anger and aggression instead of sadness. Learn how to support them and understand these often-misinterpreted indicators. Behavioral Signs of Depression in Men High levels of the hormone cortisol are released during stressful situations affecting the neurotransmitter, serotonin (a feel-good hormone), contributing to depression. You can identify depression or suicidal tendencies by paying close attention to the following behavioral changes: Anger, irritability, or aggression Avoiding family or social situations Losing interest in family responsibilities, passions and hobbies Lack of sex drive Becoming controlling/abusive in relationships Risk-taking behavior such as; unsafe sex, overspending or gambling Not being able to concentrate or remember details Excessive drinking or drug use Having frequent thoughts about death Talking about suicide Attempting suicide Factors That Lead to Depression in Men Life Events Work stress or long-term unemployment can be huge contributing factors relating to depression. This type of life event can be overwhelming, making it impossible for a man to cope. Changes in Relationships The loss of a relationship can be a significant contributing factor to the emergence of depressive symptoms and past experienced physical, sexual, or emotionally abusive relationships. With this in mind, counseling can often help individual to overcome this type of trauma. Grief and Loss Overwhelming sadness due to the loss of a loved one can trigger depression. Although normal, each person goes through their own grieving period. For example, normal responses to death are insomnia, poor appetite and loss of interest in activities. Pay attention if grief seems prolonged or out of the ordinary. Health Problems In particular, depression coexists with medical conditions. As men age, this can be passed off as normal aging, but it could be more serious. In addition, illnesses such as thyroid disorders, Addison’s disease and liver disease can cause depressive symptoms. Diabetes, cancer, heart disease, or Parkinson’s disease can affect any age, thus triggering or worsening depression. Some older men also feel like they may be suffering from dementia because of difficulties with memory this may be a symptom of depression. A trip to the doctor may be in order to help alleviate concern and worry. Depression in Men and Suicide Frequently the emotional pain occurring with depression can distort a man’s ability to see a solution beyond suicide. Individuals with depression become very rigid and constricted in the way they solve problems. The statistics below speak for themselves, helping us understand the need to reach out to those who need our support. Male suicide rates are on rising – men die by suicide 3.53 times more often than women, accounting for 70% of all suicides. Sadly, every day 129 men commit suicide. White males accounted for 69.67% of suicide deaths in 2017. In 2017, firearms accounted for 50.57% of all suicide deaths. Middle aged Men who are middle aged have the highest suicide rates. 40% of those identifying as transgender have attempted suicide in their lifetime. Males who are guy or transgendered are at an increased risk for suicide attempts, especially before age 25. Veterans often suffer from post-traumatic stress disorder (PTSD) and depression, and are more likely to act on a suicide plan. How You Can Help Now that you can identify some of the warning signs of depression, here’s how you can help: Talk about your concern and communicate that you’re there to help him. Let him know depression is a medical condition and will usually get better with treatment. Suggest professional help from a Primary Care Provider, Psychologist or Therapist. Help set up appointments and offer to accompany him – let him make the decision, but make it clear you’re there for him, no matter what he decides. If you feel he is in a dire or life-threatening situation, contact 911. Call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to talk to a trained counselor. Call the Veteran’s Crisis Line at 1-800-273-TALK (1-800-273-8255) and press “1”
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
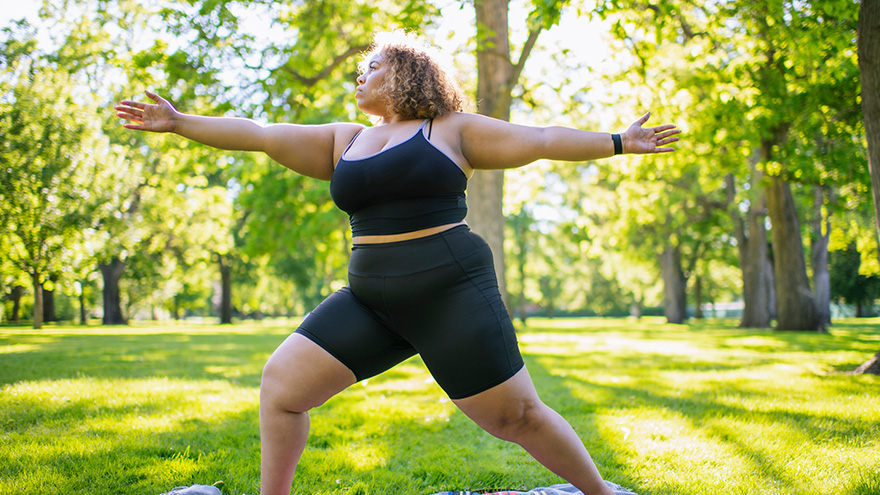
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
© alessandrobiascioli via Canva.com Ensuring a healthier and more inclusive future for LGBTQIA+ children and teens is of utmost importance to health systems in our community, especially Renown. Supporting the physical and mental health of youth in this community is key to those efforts, especially as they face unique challenges in terms of identity acceptance and social integration. Dr. Caroline Barangan, Adolescent Medicine Physician with Renown Children’s Pediatric Specialty Care, discusses what you as a parent, caregiver, friend or support system can do to be a safe space for children and teens who identify as LGBTQIA+. 1. Create a Safe Space at Home The most important action you can take for your LGBTQIA+ teen or child is to accept and support them for who they are, regardless of how they identify. “Being a teenager is already difficult enough, especially within the LGBTQIA+ community, which puts them at risk of being stigmatized, rejected and targets for bullying,” said Dr. Barangan. Your supportive words and actions can make a huge difference as a profound expression of love and understanding. Being patient and willing to learn are the foundations to a healthy and loving relationship with your LGBTQIA+ teen or child. 2. Encourage Regular Check-Ups with a Primary Care Provider (PCP) Establishing your child or teen with a PCP is not only important when an illness occurs but also for annual preventative visits and regular check-ups. “A primary care provider can screen for high-risk behaviors that would put a patient’s health in jeopardy, such as sexual experience, substance use, suicidality and self-harm,” said. Dr Barangan. “These screenings are an opportunity to provide the education and support these kids and teens need to stay healthy.” One of the main concerns LGBTQIA+ youth often have is that they will experience judgment from their provider, or the PCP will disclose sensitive information, including their sexuality or gender identity to their parents, when they are not ready to do so. Dr. Barangan emphatically reminds us that this legally cannot happen. “If a patient asks me to keep something confidential, unless they disclose that they have plans to harm themselves or others, I am legally not allowed to share that information with anyone without their permission,” said Dr. Barangan. 3. Locate Local Resources Northern Nevada is home to a variety of resources for the LGBTQIA+ community at large, including youth members of this community. "Finding resources to help them develop in a positive way and provide them with the information they need, whether it be in school, the household, the community or through a medical or mental health provider, is incredibly important,” said Dr. Barangan. Below is a list of local LGBTQIA+ community resources open to you and your children: Our Center LGBTQIA+ Health Services at Northern Nevada HOPES Northern Nevada Pride Festival & Community Parade (happens every July in Reno) Sassabration (happens every September in Carson City) Lake Tahoe Pride (events and resources shared on Facebook)
Read More About 3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
-
Nurturing Your Child's Back-to-School Mental Health
The back-to-school season is here, and ensuring your child's successful transition involves more than just school supplies and schedules. At Renown Children’s Hospital, and in collaboration with Nevada Pediatric Psychiatry Solutions, we understand the vital role that mental health plays in a child's overall well-being and academic performance. Below we'll guide you through essential tips for a smooth back-to-school experience, with a special focus on nurturing your child's mental health. How to Support Your Child’s Mental Health from Home Remember, the below strategies can be adapted to align with your child's personality, learning style and household dynamics. Flexibility and understanding are key in tailoring these tips to suit your child's unique needs. 1. Be Open to Communication: Recognize that effective communication is the cornerstone of understanding your child's feelings and concerns. Create a safe space where your child feels comfortable expressing their thoughts. Listen to learn, without judgment. Make it a point to validate their emotions and ensure they are heard. Encourage sharing experiences,worries, friends and challenges they may be facing. Having open conversations about sensitive topics opens the door for discussion and understanding. Make yourself available. 2. Establish a Routine: A consistent routine can offer a sense of stability and predictability for your child, and anticipation helps to decrease anxiety and establish a sense of control. Join forces and design a daily schedule that includes time for schoolwork, play, physical activity, meals and relaxation. Be flexible about the structure to allow room for last-minute changes including extra activities based on that day’s needs as well. Always add time for play and bonding. 3. Practice Compassion: Back-to-school can come with big emotions. Listening reflexively and acknowledging these feelings can help you and your child act positively on these big emotions. 4. Get Involved: Actively engage in your child's school life by participating in school events, meetings and discussions. Show interest in their educational journey, ask about their experiences and provide guidance when needed. Being present in their academic pursuits not only boosts their confidence but also strengthens the parent-child bond. 5. Use Positive Reinforcement: Celebrate your child's achievements, no matter how small they may seem. This allows for a sense of accomplishment and boosts self-esteem. Praise efforts, progress and perseverance, whether it's completing an assignment, making a new friend or overcoming a challenge. This positivity encourages a growth mindset and resilience. 6. Organize a Schoolwork Zone: Create a comfortable workspace at home dedicated to school-related tasks. Customize the area based on your child's preferences and needs. Having a designated space for studying and completing assignments promotes focus, reduces distractions and enhances their overall learning experience.
Read More About Nurturing Your Child's Back-to-School Mental Health
-
Departamento destacado: Patient Access
Health systems across the country recently celebrated Patient Access Week from April 2-8. Join us in recognizing our Patient Access team at Renown! Fighting the Good Fight starts the moment a patient steps onto the grounds of our health system. When patients visit Renown on their healthcare journey, they look to the experts to not only help them navigate through the complexities of the process but also ensure their experience with us starts off on the right foot. Renown Health’s Patient Access Representatives (also referred to as “PARs”) are the faces of this entire process. As the key links between patients, providers and insurers, they strive to create a welcoming and respectful environment for everyone. PARs are committed to providing all of Renown’s patients access to the quality care when needed. After all, it’s in their name! A Friendly Face PARs are the front faces of almost all clinical areas at Renown. As the starting point for much of the patient experience, the day-in-the-life of PARs can vary. Checking patients in and out, getting demographic information, verifying insurance, answering phone calls, fostering communication between patients and their care teams, scheduling patients for follow-ups, explaining financial responsibilities and our financial aid programs, creating an overall positive experience and environment, the list goes on – but they all remain united under one goal: setting patients off on the right foot as they access care through our health system. “Each day, PARs are met with new patients who are seeking solutions to different concerns,” said Macy Betts, PAR for Renown Women’s Health. “We are the front doors to this department. We are not just checking patients in and out; we are the first step to the patients receiving the care they deserve.” “We take pride in our work,” added Tanya Quintanilla, Shari Longley and Nancy Arroyo Garcia, PARs for Renown Pediatrics. “Usually, we are the first point of contact within Renown, so we don’t take our role lightly. For example, when we see a newborn, we must ensure the registration has been verified, which consists of patient demographics, patient preferences and insurance verification. We need to be consistent and thorough because what we do affects every point of contact a patient may have within Renown.” “As my team’s senior PAR, my day begins with gathering the outpatient therapy work queue numbers and assigning the team to work them,” added Logan Johnson, Senior PAR in Pre-Registration at Renown. “Our goal is to contact and schedule patients for physical, occupational and/or speech therapy as soon as possible so that they have the maximum benefit and can get back to a normal life as quickly as possible. Our encounters can make or break the entire experience.” PARs never underestimate the power of good communication and compassion. Even during the busiest of times, our PARs work diligently to ensure all patients and their care teams fully understand the administrative side of whichever part of their journey they are about to embark on, lending a helping hand and a smile. “Whether you’re communicating with patients, leaders or coworkers, communication is key,” said Jonathan Figueroa, PAR for the Renown Institute for Heart & Vascular Health (IHVH). “We try and make sure that we do everything possible to make their visit go as smoothly as possible.” “Communication makes the world go round,” added Keith Madrona, Sherry Riley, Erika Rios and Andie Kilpatrick, PARs at Renown Urgent Care – Ryland. “Having a friendly attitude and demeanor is very important. “The PARs in Labor & Delivery do so much more than just registering patients – from escorting expectant parents to their rooms, welcoming newborn babies, processing pre-estimates and more – and the patience and excellent communication I receive from other teams is what keeps me going,” added Nanci Barash-Vietti, PAR for Renown Labor & Delivery (L&D). “This is critical to the success and effectiveness of the PARs in our department.” Shift changes for PARs mimic other teams at Renown, leveraging technology and both written and spoken communication to ensure the next shift begins successfully. "When I come in, the night shift will give me a report on what is going on and what the schedule looks like during the day; then I log in to my computer and get everything that I will need for that day up on the screen,” said Allie Boracchia, PAR for Renown L&D. “Usually around this time we have a 7-8 a.m. induction scheduled for the first patient, so I will grab the pre-made packet that the night shift put together, the unit clerk will call the nurse to get a room number, and I take the patient to the room and have them sign all the forms. After the patient has the baby, then we admit them and finish registration. This is continuous all day long.” Our PARs all agree that regardless of the setting, whether it be emergent or routine, every patient is looking for that advocate from the moment they enter through our doors. “Being friendly, patient and understanding is a must,” said Sheryl Lundgren, PAR for the William N. Pennington Institute for Cancer. “It is so nice being able to brighten the days of patients who are living with a cancer diagnosis.” “In the urgent care setting, a lot of the patients we see are not feeling their best, so it is important that we show them we care and are here to help make check in go smoothly,” added Sam Deithrich, PAR at the Renown Urgent Care – Los Altos. “Patients are relieved that they are speaking to a real person that will help set up appointments,” added Rick Jordan and Celeste Landry, PARs in Lab Services at Renown South Meadows. PARs embrace lifelong learning at Renown, especially as their roles differ day-to-day. They are always ready to jump in and assist on tasks that might be new for them, growing their skills on the job and never hesitating to say, “How can I help?” “As a PAR, you are always learning new things, even when it seems like you know just about everything,” said Liz Cardenas-Ramos, PAR for Renown Endocrinology. “It’s been such a positive experience.” “Giving yourself grace to learn and grow in Patient Access is the key,” said Maggie Savoie, PAR for Renown Primary Care – Fernley. “I find myself learning every day at Renown, and if you’re learning, you’re growing. Being able to take a breath and say, ‘this is a learning opportunity for me, and tomorrow I will be better a better PAR because I’ve gained this knowledge’ is an amazing way to stay positive in the position.” “In L&D, we are all multi-tasking, and every day I am learning something new about my department and patients, as well as how to excel in my position,” added Nanci Barash-Vietti. Renown PARs are the front lines to health care access, and they wear that badge with pride. Jeanette Flores, PAR in the Emergency Department at Renown South Meadows, sums up the role of Patient Access well: “Talk about first impressions!” “I am proud of our team and the excellent care we give our patients,” said Dawn Linker, PAR for the Renown IHVH. “We want them to have a good experience.” Impactful Accomplishments The role of our Patient Access team members goes beyond the desk. A patient’s healthcare journey begins, and sometimes even ends, with the helping hands of our PARs, leaving a lasting positive impression of Renown. "Our interactions with the patients make a difference before they see the provider, so we always demonstrate a welcoming and helpful atmosphere for the patients to feel like their needs are being met,” said Mary Dettling, PAR for Renown Endocrinology. “I love seeing the difference we make in peoples’ lives,” added Shannon Leone, PAR for the Stacie Mathewson Behavioral Health & Addiction Institute. “We can get patients at their toughest and worst times. Watching them overcome their fears, traumas and addictions has been very rewarding.” Our PARs don’t just make goals for themselves – time and time again, they surpass them, all in the name of patient experience and excellence. “We have not only met our monthly point-of-sale scores, but we also have exceeded our stretch goal for the last eight months and our scores have been in the 50th percentile or higher,” said Jeanette Flores. “Along with being the top point-of-sale collectors, we have also been known to be some of the sweetest and most helpful staff at South Meadows,” said Katie Morrill, PAR in the Emergency Department at Renown South Meadows. As their teams grow, so does their impact on our patients. PARs are dedicated to providing the best customer service possible, and with their expanding teams, that service goes even further, even throughout the pandemic. “A year ago, we only had one PAR; now, we have a full and amazing team,” said Alex Bucholz, PAR for Renown Advanced Wound Care. “We have come so far in a short amount of time.” "During the pandemic, we have maintained a core group of individuals who come in every day and help keep this office and all its parts moving smoothly,” added Shannon Leone. “We have maintained a full patient load the last three years and never had to close our office for any reason. We have even had the opportunity to start our Medicated Assisted Treatment and Transcranial Magnetic Stimulation programs.” "We successfully operated and maintained our pediatric COVID clinic, which is the only one within our five clinics,” added Tanya Quintanilla, Shari Longley and Nancy Arroyo Garcia. “We feel proud knowing our tiny humans are protected with the COVID vaccine.” Like many other teams at Renown, our PARs are masters at teamwork. Despite any obstacles that may happen along the way, they are always there for each other to ensure every patient gets the care and attention they deserve. “We call ourselves the ‘A-Team’ here in Pulmonary,” said Shannon Birnberg, PAR for Renown Pulmonary & Sleep Medicine. “We have persevered through changes, additions and departures. We are most proud of bringing different personalities to the team and being super strong and effective.” “I have noticed the team always steps up whenever needed,” added Brittany Hughes, PAR for the Renown IHVH. “Everyone has a great attitude and is very positive!” “While our team is fairly new, we are growing together, learning our strengths and weaknesses and always pushing for stronger unity,” added Angel Freer, PAR in the Emergency Department at Renown Regional. When our PARs find ways to simplify a process or make a workflow run more efficiently, they don’t waste any time in making that happen. They take any opportunity to enhance patient experience. “Our team came up with a solution on how to get patients registered faster,” said Jess Castillo-Marquez, PAR in Lab Services at Renown Regional. “We came up with modalities which assign each PAR their own procedure in which they will be registering for during their scheduled shift. It has been a great success, helping our productivity and keeping our patients satisfied with our service.” “We are proud of our successful implementation of our new therapy workflow,” added Logan Johnson. “Patients are now waiting much less to be contacted about their care.” Our PARs know that teamwork makes the dream work, and their commitment to the patients they serve – and the goals they continue to blow out of the water – continue to inspire them daily. “You are only as strong as your team,” said Aundie Yonker, PAR in the Emergency Department at Renown Regional.
-
Multiple Sclerosis Research Opportunities in Northern Nevada
There are nearly 1 million adults living with MS in the United States alone. For comparison, that is roughly the entire population of the Reno/Sparks and Las Vegas areas combined. MS is a neurological autoimmune condition which means that the immune system of patients with MS attacks the body’s myelin, a protective substance that covers your nerves. When this happens, the unprotected nerves can be damaged. Patients with MS may experience many different symptoms ranging from mild to severe, such as mobility and vision problems, fatigue and difficulty thinking. MS is usually diagnosed between the ages of 20-50, but late onset MS can occur in patients over 50 years old. While there is no cure for MS, there are effective treatments that can help reduce the burden of patients’ symptoms and create a positive quality of life. At Renown Health, we have joined the fight against MS through a partnership between advanced neurology programs and providers and our research office. We are proud to offer newly diagnosed MS patients the opportunity to choose between standard care treatment options or participating in an open label clinical trial, the AGNOS study. This study is assessing the impact of a new medication, ofatumumab, as the first disease modifying therapy participants receive for managing relapsing remitting MS, the most common form of MS.
Read More About Multiple Sclerosis Research Opportunities in Northern Nevada
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Plan Early: Completing Your Advance Directive
We plan for the birth of a child, weddings and retirement, but rarely do we discuss how we want to be cared for at the end of our lives. Getting through this challenging conversation and completing an Advance Directive can give you peace of mind that your loved ones will not have to make difficult choices on your behalf. The best time to complete an Advance Directive is now – don’t wait until a life-limiting illness or crisis occurs to discuss your views about end-of-life care and to learn what choices are available. By preparing in advance, you can help reduce the doubt and anxiety related to decision-making for your family if you cannot speak for yourself. What are Advance Directives? An Advance Directive is a document that states your choices about medical treatment and names another person to make medical decisions on your behalf if you are unable to. This document allows you to make legally valid decisions about future medical care. “Completing your Advance Directive is a gift you give your family,” says Director of Palliative Care, Mary-Ann Brown RN, MSN. “The stress associated with these difficult decisions is decreased if everyone knows what is important to you and what you want at the end of life.”
Read More About Plan Early: Completing Your Advance Directive
-
Estate Planning Mistakes to Avoid
August is National Make-a-Will month. We talked to Renown Health Foundation Planned Giving Officer, Abbey Stephenson, to learn more about wills, trusts, and estate plans and why you should feel motivated this month to get started. Did you know that 2/3 of Americans don't have a will or trust? If this is you, don’t worry, you’re not alone. Although there are laws in place to determine who inherits your assets if you die without a will or trust, having a will or trust ensures your assets go where you want them to go after you are gone. They can also help minimize disputes between family members and heirs about who gets what. In Nevada, the laws that govern who gets what if you die without a will or trust can be found in Chapter 134 of the Nevada Revised Statutes. There are other documents that people often prepare at the same time as their will or trust – like an advance health care directive and durable power of attorney for assets. These documents all together are called an estate plan. Although they have other purposes too (like nominating a guardian for a child, planning for disability or avoiding probate, which is a court process), wills and trusts are documents that say who will receive your assets after you are gone. The most common type of trust is often called a revocable living trust or a family trust. People who have a trust usually still have a will, although it is a shorter form of will called a pour-over will. It’s a good idea to talk to an estate planning attorney about whether or not a trust makes sense for your family or circumstances. Now that you’re ready to get started, here are some mistakes to avoid: 1. Failing to plan Not setting aside the time to plan may be the biggest mistake. Failing to prioritize preparing or updating your estate plan means your last wishes and desires may not be fulfilled. The right documents memorialize what you would like to happen upon your disability and death so that other people can know and follow your wishes with respect to your care and your assets. 2. Failing to coordinate beneficiary designations Certain types of assets like life insurance and retirement accounts are not covered by your will or trust and need to be addressed separately. These types of assets are referred to as non-probate assets because they transfer under contract principles and don’t require court supervision or probate to be distributed to the named beneficiaries. By completing beneficiary designation forms provided by the retirement account custodian, insurance company or financial institution, you can direct your assets to one or more beneficiaries. 3. Failing to title your assets properly Asset titling refers to how you own your asset – such as in your individual name, jointly with someone else, or in a trust or entity. For example, assets titled for two people with a “right of survivorship” will automatically go to the surviving owner. Review your asset titling and make changes, if needed, to ensure your property and assets are passed down the way you intend. 4. Failing to include charities meaningful to you In addition to providing for family members and other important people in your life, you many also choose to give to charities meaningful to you in your estate plan. When you include a charity in your estate plan, that gift is called a planned gift and many charitable organizations, including Renown, recognize such donations through their legacy giving societies. As you prepare to make your own will or a more comprehensive estate plan, we recommend you consult with a lawyer. Here are some free resources that may be helpful too: Renown Health Foundation is proud to sponsor the Family Estate Planning Series put on by PBS Reno and the Community Foundation of Northern Nevada. The free, 8-week course of 90-minute, in-depth workshops is a great place to learn much more and to help you get started in the planning process. The next course begins on September 7, 2022. More information can be found here. Renown Health offers periodic advance health care directive workshops where attendees can learn about, complete, and sign their directive. The next workshop is scheduled for September 14th. More information can be found here. The American College of Trust and Estate Counsel provides information on a number of commonly asked estate planning questions here. If you are interested in including a charitable gift to Renown in your estate plan, we would be happy to talk to you about how your gift will make a difference for our mission. Please contact Abbey Stephenson at abbey.stephenson@renown.org or visit renown.org/LegacyGiving to learn about Renown Health Foundation’s Legacy Giving Society and ways to give.
-
Suicide Risk How to Spot a Friend in Crisis
How can you tell if a friend is in trouble or struggling with suicidal thoughts? And how can you support them in finding help? Are you feeling virtually exhausted? Life is always challenging, but the mental fallout of a global pandemic is real. Contributing to the loneliness epidemic is the shifting American lifestyle. More Americans live alone (28%) now than ever before, and fewer have kids. First, let’s acknowledge this is a time of anxiety and worry for everyone. Economic uncertainty, job transitions, grief, and loneliness are a perfect storm for mental stress. Even before the COVID-19 (coronavirus) pandemic mental health was a concerning issue, now it is a relevant topic of crisis. Secondly, anyone can struggle with suicidal thoughts. Those suffering from drug addiction are especially vulnerable. In particular the U.S. is currently seeing a rise in drug overdoses by almost 18% due to the pandemic. Unfortunately, suicide is responsible for one U.S. death every 11 minutes, according to the Centers for Disease Control and Prevention. Not to mention the millions who think about it, make a plan or attempt it. It is important to remember that suicidal thoughts, plans or intent must be helped immediately. Understanding Suicide Risk To clarify, depression is not a choice. No one wishes for endless days of feeling down, sleepless nights, and feeling as if you are in a dark tunnel. Currently, one in five Americans will experience a mental illness this year. This means one of your friends is struggling, right now. Specifically, consider this: When your body feels pain it talks to your mind. When your mind is suffering who does it talk to? So, how can you tell if a friend is in trouble? According to the National Institute of Mental Health be on the lookout for some depression clues below. Signs and Symptoms of Depression Persistent sad, anxious, or “empty” mood Feelings of hopelessness, or pessimism Irritability Loss of interest or pleasure in hobbies and activities Decreased energy or fatigue Moving or talking more slowly Feeling restless or having trouble sitting still Difficulty concentrating, remembering, or making decisions Signs and Symptoms of Suicide Risk Expressing feelings of hopelessness or having no purpose Talking about feeling trapped or being in unbearable pain Talking about being a burden to others Increasing the use of alcohol or drugs Sleeping too little or too much Withdrawing or isolation Displaying extreme mood swings. Talking about wanting to die or to kill oneself (Reference: Suicide Awareness Voices of Education) How to Help a Suicidal Friend It can feel awkward to approach the subject of suicide with a friend, but take any of the above warning signs seriously. Other ways you can help are by: Encouraging self-care and making sure they take care of basic needs Listen to their worries without judgement Ask them what they need from you, then follow through with action Let them know they are not a burden Don’t minimize or invalidate their feelings Point them to helpful resources Be their advocate and get them help If someone you know is in a life-threatening crisis situation, call 911 immediately. Suicide Risk Resources: National Suicide Prevention 24/7 Lifeline: 1-800-273-8255 Ayuda En Español: (Spanish National Suicide Prevention Lifeline) 1-800-628-9454 Crisis Text Line: Text HOME (or CONNECT) to 741741 to chat with a crisis counselor 24/7 free of charge. The National Alliance on Mental Health: 1-800-950-6264 Substance Abuse and Mental Health Services Administration: (SAMHSA) 24/7 helpline 1-800-662-4357
-
Los seis alimentos con más sal: ¿El alto contenido de sodio aumenta el riesgo de sufrir un derrame cerebral?
Excess amounts of sodium doesn’t just increase your risk of a heart attack, it can also increase your risk of a stroke. Unfortunately, avoiding that saltshaker may not be enough. Did you know that the average American consumes 3,400 milligrams of sodium each day? That’s a dangerous number considering that the American Heart Association recommends limiting daily sodium intake to 1,500 milligrams (about half the weight of a penny) to reduce the risk of heart disease and stroke. The problem is not necessarily that you’re putting too much salt on your food, it’s that salt is already in the foods you’re regularly eating. To help keep your sodium intake at a healthy level, make sure you’re aware of “The Salty Six,” six sneaky foods that are surprisingly high in sodium. Breads, Rolls and Tortillas: Although breads and tortillas may not initially appear to be high in sodium, we often consume several servings. Make sure to keep track of your total servings to see how they add up. Deli Meat, Cured Meats and Poultry: It may surprise you that six thin slices of deli meat can add up to more than half of your daily limit, so be mindful when building those sandwiches. Also, do your best to avoid cured meats, which often means the meat has been salted. Substitute uncured, skinless meats instead. Cheese: Salt is an important addition in the cheese-making process, as it prevents bacterial growth. Unfortunately, that added salt can increase your health risks. Limit the amount of cheese you add to meals to keep your sodium content down. Pizza: Take a quick look at the first three items above and it should be no surprise as to why pizza made the list. One slice and you’ve met at least half of your daily limit. Go easy on the cheese and try adding more veggies instead of meat. Canned Soup: One cup of canned soup can be as high as nearly 1,000 milligrams of sodium. When shopping for canned soup it’s important to check the label – not just on sodium content but serving size as well. Always select low-sodium options when possible or cook your own soup at home. Sandwiches and Burgers: A sandwich or burger from your favorite restaurant can contain more than 100 percent of your daily sodium limit. When dining out, it is best to select low-sodium options or eat a half portion to limit the amount of salt. If some of your favorite foods are on this Salty Six list, don’t panic. Although these foods can be high in sodium, it isn’t necessary to cut these foods out of your diet completely. It’s just important to eat them in moderation and be mindful of your daily sodium intake. Look for low-sodium options, use herbs and spices instead of table salt and do your best to stay under the recommended daily limit of 1,500 milligrams.”
Read More About The Salty Six: Are High-Sodium Foods Increasing Your Stroke Risk?




.jpg?rev=ddb15541cee845129a2355ba27384fb5)





