Buscar
-
Cómo comenzar y actualizar su testamento
August is National Make-a-Will Month. We talked to Abbey Stephenson, Planned Giving Officer at Renown Health Foundation, to learn more about wills, trusts and estate plans and why you should feel motivated this month to get started. Why Make a Will There are so many reasons why it is difficult to make a will or put an estate plan in place. These include: Lack of time or money to prepare a plan The misperception that “only rich people need an ‘estate plan’” How intimidating legal documents can be General discomfort with planning for the future Given the barriers to making a plan, it’s not surprising that only 32% of Americans have a will or trust in place. But having a will or trust matters because these are the documents where you can say who will inherit your assets, who will manage your assets and estate, and who should be guardian of a minor or a child with a disability. Where to Begin If you have been thinking about putting together a will and don’t know where to begin, here are some next steps you can take. 1. Learn the terms. If you have never created a will, trust, or an estate plan, the language can be hard to get used to. A few important terms to know include: Last will and testament (also known as a will): a legal document that describes how you would like your property and other assets to be distributed after your death. This is also the document where you can nominate a guardian for a minor or disabled child. Personal representative (also known as an executor): a person named in a will responsible for collecting your assets, paying your debts and final taxes, and distributing the remaining assets to those stated in your will. Personal representatives must be formally appointed by a judge and report certain information to the judge for review and approval. Living trust (also known as a revocable or family trust): a legal arrangement set up through a document called a trust instrument or a declaration of trust that gives someone called the trustee power to make decisions about the trust creator’s money or property held in the trust. Estate plan: a collection of documents that help organize what happens to you and your assets upon your disability and death. Your estate plan is comprised of documents such as a will, trust, and advance health care directive. If you want to learn more about these terms and estate planning in general, you are invited to attend a free one-hour estate planning education session on Aug. 22, 2024, at 10 a.m. or Oct. 21, 2024, at 11 a.m., hosted by Renown Health Foundation. Click here for more information and to register. 2. Create a list of assets. Start by creating a list of your assets including real estate, investments, bank accounts, retirement accounts, business ownership interests, vehicles, life insurance, valuable personal property like jewelry or artwork, and any other significant assets. Click here and read our free estate planning guide. 3. Put together a list of 2-3 people you trust. When you create your will, you need to name a personal representative who will collect all your assets, pay your debts, and work with the probate court to distribute the balance to the people and charities you name in your will. If you create a trust, you need to name a trustee to manage the trust assets under the terms of the trust document. It is a good idea to include at least two people who can take on these roles in case the first person becomes unavailable. If you do not have anyone you would trust as a personal representative or trustee, there are trust companies, banks, and other professionals and institutions who may be able to assist you. If you are the parent of a child who is under 18 or has a disability, you will also nominate a guardian in your will to care for that child if you and the other parent are gone. 4. Start a list of who you would like to inherit your assets. Which people and organizations would you like to inherit the assets you own at the time of your passing? And which assets or how much would you like them to receive? You might want to consider who relies on you for support such as family members or charities, individuals and organizations that have made a difference in your life, or those you have a special fondness for. It is important to use the legal names of individuals you include as beneficiaries and the Tax ID number for any charity you include. If you decide to make a gift to Renown as part of your will or estate plan and notify us, you will be included in the Renown Legacy Society. Legacy Society members enjoy invitations to exclusive events, special acknowledgments, and other unique benefits. Click here to learn more about the Renown Legacy Society. 5. Put together a list of your professional advisors and enlist their help. Write down the names and contact details for any professional advisors you work with such as your accountant, financial advisor, investment manager, attorney, insurance agent, and planned giving officer. You may want to seek their advice on how best to proceed and which assets are best gifted to which individuals and organizations from a tax standpoint. Collaboration among the professionals with whom you work can help your plan to run more smoothly when it is needed. Depending on your circumstances, it may make sense for you to introduce your trusted individuals to these professionals. 6. Start drafting. Once you have these items in place, you will be in a good position to begin the drafting process. There are many capable estate planning attorneys in our community who can help you with drafting. There are other drafting resources available as well, but only a licensed attorney can provide you with legal advice. Click here to attend the free Family Estate Planning Series sponsored by Renown and presented by PBS Reno and the Community Foundation of Northern Nevada.
Read More About How to Get Started and Make Updates to Your Will
-
Cómo la dieta puede afectar el riesgo y la recuperación del cáncer
Cancer affects millions of lives worldwide. Though medical advancement has done a great deal to increase the human lifespan, proper nutrition has also been proven to help in the prevention of cancer. As researchers continue their hunt for a cure, there is a lot of information out there to support the argument that nutrition is an essential component in disease prevention and management. Nutrition Services: To learn more, call us at 775-982-4000 Linking Diet and Cancer Risk Evidence shows that our diets impact our vulnerability to cancer – and our ability to fight it. The American Cancer Society states that at least 18% of all cancers in the United States are related to excess body weight, physical inactivity, alcohol consumption, and/or poor nutrition. (American Cancer Society Guideline for Diet and Physical Activity | American Cancer Society). Sure, genetics can contribute, but research continues to support the belief that following a healthy diet can reduce the likelihood of developing cancer in the first place. Renown Health’s Jessica Blauenstein, MS, RDN, LDN, CSO, Registered Dietitian and Board-Certified Specialist in Oncology Nutrition confirms the importance of a nutritious diet consisting of: Fruits and Vegetables: Eating a variety of fruits and vegetables provides large amounts of vitamins, minerals and antioxidants. Nutrient-rich, they help in fighting off oxidative stress and inflammation, both of which are factors for developing cancer. Whole Grains: A diet rich in grains such as brown rice, quinoa and oats, contains substantial amounts of fiber that helps in digestion. A few studies have shown that whole grains might offer some protection against colorectal cancer. Lean Proteins: Reducing the amount of red and processed meats in the diet by substituting lean proteins, such as poultry, fish, beans and lentils may lower the risk of developing cancer. Red and processed meats have been associated with colorectal and other cancers when consumed in large amounts. Healthy Fats: Begin focusing on healthy fats from foods like avocados, nuts, seeds and olive oil. These fats are anti-inflammatory, which may play a beneficial role in disease prevention. Avoidance of Sugar and Processed Foods: Sugar and foods high in processed ingredients have been linked to an increased risk of obesity, type 2 diabetes and some cancers. It's important to limit the intake of sugary drinks, candy and snacks in the battle against cancer. A Role of Nutrition in Cancer Recovery Nutrition becomes even more critical for individuals who receive treatment and are in recovery. Treatments such as chemotherapy, radiation therapy and surgery can take a lot out of a body, affecting appetite, digestion and nutrient absorption. Proper nutrition during and after treatment can help: Support Immune Function: A good, balanced diet will provide the essential nutrients that support a resilient immune system, which is important in fighting off infections and supporting overall health during cancer treatment. Maintain Strength and Energy Levels: Proper caloric intake, protein and micronutrients prevent muscle wasting and fatigue, allowing patients to sustain their strength and energy. Address Side Effects: Certain foods and diets can help reduce or alleviate some common side effects associated with cancer treatment, including nausea, vomiting and mucositis. Eating small, frequent meals, maintaining good hydration, and avoiding spicy or acidic foods can all ease treatment-related discomfort associated with the GI tract. Facilitate Healing and Recovery: Nutrient-rich foods promote healing and the repair of tissues that may be damaged after surgery or other medical interventions. Foods high in proteins, vitamins and minerals play a significant role in repairing and replacing damaged tissues and cells. Correct Nutritional Deficiencies: Cancer and its treatment cause vitamin D, vitamin B12 and iron deficiencies in the diet. Nutrition therapy through a registered dietitian or nutritionist can identify those deficiencies and help manage them through dietary changes or supplementary means. Related information: Nourishing Your Loved One Through Cancer Treatment
Read More About How Diet Can Affect Cancer Risk and Recovery
-
Tazón saludable de verano
Say Hello to Summer in a Bowl If you've wanted to add a heart-healthy dish to your recipe repertoire, now's the time. This tasty vegan bowl loaded with turmeric chickpeas, marinated tofu and quinoa offers essential nutrients and beneficial fats to help maintain healthy cholesterol levels and reduce the risk of heart disease.
-
Motivar a los niños a comer alimentos saludables
Do you have a picky eater in your household? Or maybe you've got a snack monster who’s all about chips and candy? We're here to share a few fun strategies to motivate your little superheroes to snack on healthy foods instead! Rainbow Power-Up Eating a rainbow isn't just for unicorns! Different colors mean different powers: Red foods like strawberries and tomatoes help your heart. Orange foods like carrots and sweet potatoes help your eyes spot things like an eagle! Green foods like spinach and broccoli help you grow super strong bones. So, create a plate with as many colors as possible. The more colors, the more powers! Super Smoothies Blend your favorite fruits, such as bananas, berries and mangoes. Add some milk or yogurt and a handful of spinach. Your kids won't taste the spinach, and they'll drink a supercharged smoothie that gives them the energy to tackle any challenge. Create a Parfait Packed with Delicious Layers! Veggie Villans Who said veggies can't be fun? Turn them into heroes by giving them cool names and fun shapes. Make carrot sticks "Captain Crunch" or broccoli florets "Broc the Rock." Dip them in hummus or peanut butter for an extra flavor kick. Snack Attack Plates Create snack plates that are as fun as they are nutritious. Combine: Cheese cubes Grapes or apple slices Nuts or seeds Whole-grain crackers Mix and match these for your perfect plate! Make Your Own Trail Mix Fuel-Up Challenges Challenge your kids to eat three different healthy foods each day. Turn it into a family game to see who can eat the most colors or try the most fruits and veggies. You can even draw up a "super snacks" chart to keep track of your progress. Final Super Tip! Even superheroes have cheat days. Don't worry if your family doesn't eat healthy every meal. Just aim to eat more of the good stuff than the not-so-great stuff. Your kid's bodies will reward them with tremendous energy, focus and strength.
-
Prepare su propia mezcla de senderos: 4 Recetas rápidas y fáciles
Craving a crunchy, sweet, and nutritious snack? Try making your own trail mix! Perfect blends of nuts, dried fruits, and a touch of chocolate can be whipped up using bulk bin ingredients or pantry staples. Enjoy this delicious, healthy snack on a hike, at the office, or on your next road trip through Nevada's scenic deserts.
Read More About Make Your Own Trail Mix: 4 Quick and Easy Recipes
-
Nutrir a su ser querido a través del tratamiento contra el cáncer
Eating healthy is a daily challenge for many, but for those with cancer, it is an even harder struggle. A cancer diagnosis affects not only those diagnosed but family members and friends, too. One key area of concern is making sure your loved one stays well by eating healthy food every day. Here are some vital cancer nutrition tips from Jessica Blauenstein, a Board Certified Specialist in Oncology Nutrition and Registered Dietitian at Renown Health. Help to Prepare Meals and Snacks for Daily Cancer Nutrition Make it grab and go. Easy-to-make meals help reduce the burden of having to cook and prepare food. Having easy to grab snacks on the counter or in the fridge can help ensure your loved one has access to those nutrients when needed. Sit outside of the kitchen. This allows your loved one to avoid cooking smells which can make them feel sick as a side effect of cancer treatments. Also try serving them cold foods such as sandwiches, cheese and crackers, or shakes which have a mild scent. Try drinkable meals. Some people with cancer find it easier to sip their calories over the course of 30 minutes to an hour. Consider smoothies or supplemental shakes such as Ensure Complete, Fairlife shakes, Orgain shakes, or Boost Plus to name a few. A great foundation for a smoothie is a protein source (Greek yogurt, protein powder, nut butters or milk) with a carbohydrate (fruits, juice or berries). Add other ingredients as desired, such as spinach, kale, and ground flaxseed or chia seeds to give it more vitamins, minerals, and fiber. Snack Ideas for Those Undergoing Cancer Treatment The following ideas are both quick and easy to make for your loved one. Chicken or tuna salad with whole grain crackers or as a sandwich on whole grain bread Greek yogurt mixed with cereal, fruit and/or nuts Cottage cheese with banana, cinnamon and/or peanut butter Favorite fruit with 100% natural peanut or almond butter spread - Try peanut butter with bananas, apples, or even celery Their favorite veggies dipped in a salad dressing of your choice - For example, carrots with hummus, tahini, or ranch dressing Cheese and whole grain crackers - Add tomato slices with a small amount of avocado, and a dash of oregano on top for more flavor Eggs scrambled with cheese, vegetables and/or salsa Peanut butter and jelly sandwich on whole grain bread A baked sweet potato with some favorite toppings Hard boiled eggs and/or egg salad with whole grain crackers, or as a sandwich on whole grain bread Oatmeal or cream of wheat prepared with milk, fruit and/or nuts Sometimes your loved one may not feel like eating or refuse to eat. If treatment side effects are impacting your loved one’s ability to eat, please visit the websites below containing recipes tailored to treat side effects. Cook for Your Life ELLICSR Of course, you may also consult a registered dietitian and/or the patients care team, if you have more cancer nutrition concerns.
Read More About Nourishing Your Loved One Through Cancer Treatment
-
Celebramos el equilibrio del azúcar en sangre esta temporada de fiestas
As the holiday season draws near, we find more reasons to celebrate with loved ones. At Renown Health, we are kicking off the celebrations early this November with American Diabetes Month. Approximately 37 million Americans, including 270,000 Nevadans, have been diagnosed with diabetes with as many as 95% of those diagnosed living with type 2 diabetes mellitus (T2DM). What is Type 2 Diabetes? Type 2 diabetes is a chronic health condition that occurs because your body is not using insulin (a hormone made by the pancreas to help cells use the food we eat for energy) as well as it should, resulting in high blood sugar levels. It is important to obtain a diagnosis for T2DM and ensure it is well-controlled to prevent serious health complications. Those with diabetes are at higher risk for blindness, kidney failure, heart disease, stroke and amputation. Tips for Supporting Your Health with Type 2 Diabetes Know Your Blood Sugar Levels: Work with your healthcare provider to establish target blood sugar levels, and make sure to monitor your levels regularly as advised by your healthcare provider to prevent or delay health complications associated with T2DM. Focus on Your Plate: Eating foods such as fruits and vegetables, lean meats or plant-based proteins, healthy fats and whole grains supports diabetes management. If choosing healthy foods is difficult due to your busy schedule, cost or simply because you aren’t sure where to start, talk with your healthcare provider who may refer you to a registered dietitian. Registered dietitian nutritionists are certified nutrition specialists who can provide education and practical tips for eating to support your T2DM diagnosis with visits covered by many insurance plans. Prioritize Staying Active: Engaging in regular exercise is good for everyone, especially those living with T2DM. Exercise helps your cells become more sensitive to insulin and therefore supports healthy blood sugar levels. Always check with your healthcare provider prior to beginning a new exercise plan. Support Stress Reduction: Stress is unavoidable but can be managed through regular exercise, getting enough quality sleep (7-8 uninterrupted hours per night) and practicing meditation and other mindfulness techniques. Plan Ahead for Holiday Gatherings: There’s still room for celebration while focusing on blood sugar management. Consider bringing a healthy dish to your gathering, focus on filling your plate with vegetable sides and eating those first and incorporate a family walk after dinner. If traveling, pack nutritious snacks that support your health and keep you full. Lastly, enjoy the special dishes and desserts this season has to offer in single-serving portions.
Read More About Celebrating Blood Sugar Balance This Holiday Season
-
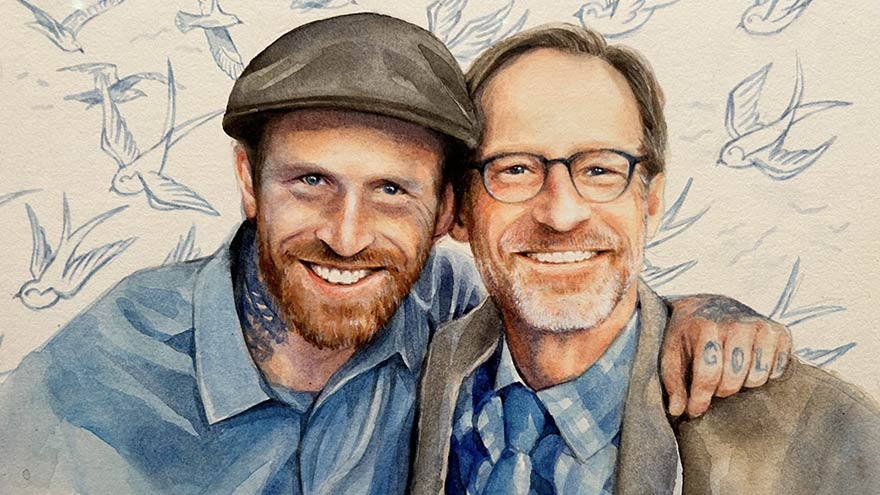
Por qué doy: La historia de Dan
In the fall of 2020, Dan's world was suddenly shaken when he received a distressing call: his son, Jeremy, was admitted to Renown with complications from spinal meningitis. Without a second thought, Dan rushed from Southern California to be by Jeremy's side. For an agonizing 10 days, Dan remained in the ICU. He was overwhelmed with worry and helplessness as Jeremy fought for his life on a ventilator. During this time, Dan, an esteemed artist and professor, found comfort in the collection of artworks adorning the walls at Renown. With more than 2,000 pieces of original art, Renown has meticulously curated hospital rooms, hallways and various spaces to support those in need. Dan, who talks about art's magic every day as a professor, experienced its power in a new light.
-
¿Por qué me cae el cabello? Explicación de la alopecia
© MikeSaran via Canva.com Hair is often considered a symbol of identity and self-expression, from scalps and eyebrows to beards and bodies. But what happens when this symbol starts to fall out? The 6.7 million people across the country living with alopecia know this feeling all too well. Alopecia, or hair loss, is a medical condition with variable causes, presentations and treatments. Experts at Renown Health dive into the world of alopecia, its causes and how to address it – especially as we embrace National Alopecia Awareness Month this September. Types of Alopecia The term “alopecia” is a broad umbrella term that encompasses many different forms of hair loss that can present itself at any age, no matter your gender or ethnicity. The most common types include: Alopecia Areata: An autoimmune disorder where the immune system targets hair follicles, typically resulting in patches of hair loss on the scalp and/or other body parts. More severe forms of alopecia areata also exist, such as alopecia totalis and alopecia universalis. Androgenetic (or Androgenic) Alopecia: A disorder also known as male or female pattern baldness that causes gradual hair thinning and loss often around the temples and crown. Unlike alopecia areata, this form of alopecia is usually hereditary. Telogen Effluvium: A condition resulting in hair shedding, typically after high-stress or infectious events, such as after giving birth or after a COVID-19 infection. This usually resolves itself within a few months to a year. Traction Alopecia: Hair loss resulting from the effects of tight braiding or styling of the hair, which can cause permanent loss over time. Scarring and Inflammation-Mediated Hair Loss: Patterns of hair loss related to lupus, lichen planus or other autoimmune conditions that can unfortunately be permanent and progressive. Options to Treat Alopecia While there isn’t a cure for most types of alopecia, some treatments are available to help minimize the effects of the condition and promote hair growth. Treatment varies depending on the type of alopecia. Potential options can include: Topical Minoxidil: An FDA-approved over-the-counter medication available in foam or liquid form and applied directly to the scalp, which helps stimulate hair growth by increasing blood flow to hair follicles. Hormone Therapies: A hormone regimen that can help minimize the resulting hair thinning and balding. Corticosteroids: A topical cream or ointment – or an injection for severe cases – that help reduce inflammation and re-grow hair. Low-Level Laser Therapy: A therapeutic, non-invasive intervention involving wearing special caps or combs that release painless, low-level lasers to stimulate hair follicles. Healthy Diets and Nutritional Supplements: A diet rich in vitamins and minerals essential for hair health, such as biotin and collagen, can aid in recovery. Vitamin D and iron are also important hair growth nutrients. Stress Management: Stress can impact the speed and frequency of hair loss. Managing your stress can help mitigate the effects of alopecia. Treatment for alopecia is not a one-size-fits-all approach. A scalp skin biopsy may help determine a cause for hair loss and help guide the best management strategies with your provider. Addressing the Emotional Impacts Even though alopecia isn’t life-threatening, the impacts of the condition can affect your self-esteem and self-image. The most powerful tool to help you manage alopecia is knowledge. Keeping yourself educated about your condition, and encouraging your loved ones to do the same, can help arm yourself with the acceptance and self-compassion you need and help combat misconceptions. With the rise in awareness in the mainstream media for alopecia and other hair conditions, beauty standards and fashion are shifting to become more inclusive for those experiencing hair loss. Celebrating the many diverse hairstyles and fashion statements can help you regain your confidence. There are many options you can advantage of to help style your hair and protect your scalp: Hairpieces: Wigs, extensions and other hairpieces can help cover up balding or thinning patches and add volume to your hair. Hairpieces have come a long way in the past few decades, and many use real human hair. Hats: Hats serve a dual purpose – a fun fashion accessory to help boost your confidence and a method of protecting your scalp from the sun. As someone with alopecia, your scalp is more exposed, and hats can provide that extra layer of protection you need. Scalp Sunscreens: While regular body sunscreens can provide good scalp sun protection, they can result in oily scalp and hair appearance. Sunscreens that are specifically designed for the scalp are available at most beauty stores or online. Remember, patience is fundamental, as many treatments require consistent use over time to see noticeable results. Stay resilient, and don’t give up – you are not alone in your alopecia journey.
Read More About Why Is My Hair Falling Out? Alopecia Explained
-
Departamento destacado: Acceso del paciente
Health systems across the country recently celebrated Patient Access Week from April 2-8. Join us in recognizing our Patient Access team at Renown! Fighting the Good Fight starts the moment a patient steps onto the grounds of our health system. When patients visit Renown on their healthcare journey, they look to the experts to not only help them navigate through the complexities of the process but also ensure their experience with us starts off on the right foot. Renown Health’s Patient Access Representatives (also referred to as “PARs”) are the faces of this entire process. As the key links between patients, providers and insurers, they strive to create a welcoming and respectful environment for everyone. PARs are committed to providing all of Renown’s patients access to the quality care when needed. After all, it’s in their name! A Friendly Face PARs are the front faces of almost all clinical areas at Renown. As the starting point for much of the patient experience, the day-in-the-life of PARs can vary. Checking patients in and out, getting demographic information, verifying insurance, answering phone calls, fostering communication between patients and their care teams, scheduling patients for follow-ups, explaining financial responsibilities and our financial aid programs, creating an overall positive experience and environment, the list goes on – but they all remain united under one goal: setting patients off on the right foot as they access care through our health system. “Each day, PARs are met with new patients who are seeking solutions to different concerns,” said Macy Betts, PAR for Renown Women’s Health. “We are the front doors to this department. We are not just checking patients in and out; we are the first step to the patients receiving the care they deserve.” “We take pride in our work,” added Tanya Quintanilla, Shari Longley and Nancy Arroyo Garcia, PARs for Renown Pediatrics. “Usually, we are the first point of contact within Renown, so we don’t take our role lightly. For example, when we see a newborn, we must ensure the registration has been verified, which consists of patient demographics, patient preferences and insurance verification. We need to be consistent and thorough because what we do affects every point of contact a patient may have within Renown.” “As my team’s senior PAR, my day begins with gathering the outpatient therapy work queue numbers and assigning the team to work them,” added Logan Johnson, Senior PAR in Pre-Registration at Renown. “Our goal is to contact and schedule patients for physical, occupational and/or speech therapy as soon as possible so that they have the maximum benefit and can get back to a normal life as quickly as possible. Our encounters can make or break the entire experience.” PARs never underestimate the power of good communication and compassion. Even during the busiest of times, our PARs work diligently to ensure all patients and their care teams fully understand the administrative side of whichever part of their journey they are about to embark on, lending a helping hand and a smile. “Whether you’re communicating with patients, leaders or coworkers, communication is key,” said Jonathan Figueroa, PAR for the Renown Institute for Heart & Vascular Health (IHVH). “We try and make sure that we do everything possible to make their visit go as smoothly as possible.” “Communication makes the world go round,” added Keith Madrona, Sherry Riley, Erika Rios and Andie Kilpatrick, PARs at Renown Urgent Care – Ryland. “Having a friendly attitude and demeanor is very important. “The PARs in Labor & Delivery do so much more than just registering patients – from escorting expectant parents to their rooms, welcoming newborn babies, processing pre-estimates and more – and the patience and excellent communication I receive from other teams is what keeps me going,” added Nanci Barash-Vietti, PAR for Renown Labor & Delivery (L&D). “This is critical to the success and effectiveness of the PARs in our department.” Shift changes for PARs mimic other teams at Renown, leveraging technology and both written and spoken communication to ensure the next shift begins successfully. "When I come in, the night shift will give me a report on what is going on and what the schedule looks like during the day; then I log in to my computer and get everything that I will need for that day up on the screen,” said Allie Boracchia, PAR for Renown L&D. “Usually around this time we have a 7-8 a.m. induction scheduled for the first patient, so I will grab the pre-made packet that the night shift put together, the unit clerk will call the nurse to get a room number, and I take the patient to the room and have them sign all the forms. After the patient has the baby, then we admit them and finish registration. This is continuous all day long.” Our PARs all agree that regardless of the setting, whether it be emergent or routine, every patient is looking for that advocate from the moment they enter through our doors. “Being friendly, patient and understanding is a must,” said Sheryl Lundgren, PAR for the William N. Pennington Institute for Cancer. “It is so nice being able to brighten the days of patients who are living with a cancer diagnosis.” “In the urgent care setting, a lot of the patients we see are not feeling their best, so it is important that we show them we care and are here to help make check in go smoothly,” added Sam Deithrich, PAR at the Renown Urgent Care – Los Altos. “Patients are relieved that they are speaking to a real person that will help set up appointments,” added Rick Jordan and Celeste Landry, PARs in Lab Services at Renown South Meadows. PARs embrace lifelong learning at Renown, especially as their roles differ day-to-day. They are always ready to jump in and assist on tasks that might be new for them, growing their skills on the job and never hesitating to say, “How can I help?” “As a PAR, you are always learning new things, even when it seems like you know just about everything,” said Liz Cardenas-Ramos, PAR for Renown Endocrinology. “It’s been such a positive experience.” “Giving yourself grace to learn and grow in Patient Access is the key,” said Maggie Savoie, PAR for Renown Primary Care – Fernley. “I find myself learning every day at Renown, and if you’re learning, you’re growing. Being able to take a breath and say, ‘this is a learning opportunity for me, and tomorrow I will be better a better PAR because I’ve gained this knowledge’ is an amazing way to stay positive in the position.” “In L&D, we are all multi-tasking, and every day I am learning something new about my department and patients, as well as how to excel in my position,” added Nanci Barash-Vietti. Renown PARs are the front lines to health care access, and they wear that badge with pride. Jeanette Flores, PAR in the Emergency Department at Renown South Meadows, sums up the role of Patient Access well: “Talk about first impressions!” “I am proud of our team and the excellent care we give our patients,” said Dawn Linker, PAR for the Renown IHVH. “We want them to have a good experience.” Impactful Accomplishments The role of our Patient Access team members goes beyond the desk. A patient’s healthcare journey begins, and sometimes even ends, with the helping hands of our PARs, leaving a lasting positive impression of Renown. "Our interactions with the patients make a difference before they see the provider, so we always demonstrate a welcoming and helpful atmosphere for the patients to feel like their needs are being met,” said Mary Dettling, PAR for Renown Endocrinology. “I love seeing the difference we make in peoples’ lives,” added Shannon Leone, PAR for the Stacie Mathewson Behavioral Health & Addiction Institute. “We can get patients at their toughest and worst times. Watching them overcome their fears, traumas and addictions has been very rewarding.” Our PARs don’t just make goals for themselves – time and time again, they surpass them, all in the name of patient experience and excellence. “We have not only met our monthly point-of-sale scores, but we also have exceeded our stretch goal for the last eight months and our scores have been in the 50th percentile or higher,” said Jeanette Flores. “Along with being the top point-of-sale collectors, we have also been known to be some of the sweetest and most helpful staff at South Meadows,” said Katie Morrill, PAR in the Emergency Department at Renown South Meadows. As their teams grow, so does their impact on our patients. PARs are dedicated to providing the best customer service possible, and with their expanding teams, that service goes even further, even throughout the pandemic. “A year ago, we only had one PAR; now, we have a full and amazing team,” said Alex Bucholz, PAR for Renown Advanced Wound Care. “We have come so far in a short amount of time.” "During the pandemic, we have maintained a core group of individuals who come in every day and help keep this office and all its parts moving smoothly,” added Shannon Leone. “We have maintained a full patient load the last three years and never had to close our office for any reason. We have even had the opportunity to start our Medicated Assisted Treatment and Transcranial Magnetic Stimulation programs.” "We successfully operated and maintained our pediatric COVID clinic, which is the only one within our five clinics,” added Tanya Quintanilla, Shari Longley and Nancy Arroyo Garcia. “We feel proud knowing our tiny humans are protected with the COVID vaccine.” Like many other teams at Renown, our PARs are masters at teamwork. Despite any obstacles that may happen along the way, they are always there for each other to ensure every patient gets the care and attention they deserve. “We call ourselves the ‘A-Team’ here in Pulmonary,” said Shannon Birnberg, PAR for Renown Pulmonary & Sleep Medicine. “We have persevered through changes, additions and departures. We are most proud of bringing different personalities to the team and being super strong and effective.” “I have noticed the team always steps up whenever needed,” added Brittany Hughes, PAR for the Renown IHVH. “Everyone has a great attitude and is very positive!” “While our team is fairly new, we are growing together, learning our strengths and weaknesses and always pushing for stronger unity,” added Angel Freer, PAR in the Emergency Department at Renown Regional. When our PARs find ways to simplify a process or make a workflow run more efficiently, they don’t waste any time in making that happen. They take any opportunity to enhance patient experience. “Our team came up with a solution on how to get patients registered faster,” said Jess Castillo-Marquez, PAR in Lab Services at Renown Regional. “We came up with modalities which assign each PAR their own procedure in which they will be registering for during their scheduled shift. It has been a great success, helping our productivity and keeping our patients satisfied with our service.” “We are proud of our successful implementation of our new therapy workflow,” added Logan Johnson. “Patients are now waiting much less to be contacted about their care.” Our PARs know that teamwork makes the dream work, and their commitment to the patients they serve – and the goals they continue to blow out of the water – continue to inspire them daily. “You are only as strong as your team,” said Aundie Yonker, PAR in the Emergency Department at Renown Regional.
-
11 Consejos que los cuidadores deben conocer
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Planifique con anticipación: Cómo completar su directiva anticipada
We plan for the birth of a child, weddings and retirement, but rarely do we discuss how we want to be cared for at the end of our lives. Getting through this challenging conversation and completing an Advance Directive can give you peace of mind that your loved ones will not have to make difficult choices on your behalf. The best time to complete an Advance Directive is now – don’t wait until a life-limiting illness or crisis occurs to discuss your views about end-of-life care and to learn what choices are available. By preparing in advance, you can help reduce the doubt and anxiety related to decision-making for your family if you cannot speak for yourself. What are Advance Directives? An Advance Directive is a document that states your choices about medical treatment and names another person to make medical decisions on your behalf if you are unable to. This document allows you to make legally valid decisions about future medical care. “Completing your Advance Directive is a gift you give your family,” says Director of Palliative Care, Mary-Ann Brown RN, MSN. “The stress associated with these difficult decisions is decreased if everyone knows what is important to you and what you want at the end of life.”
Read More About Plan Early: Completing Your Advance Directive








.jpg?rev=ddb15541cee845129a2355ba27384fb5)

