Buscar
-
De la enfermera de la NICU de Renown a la madre de la NICU: El viaje inspirador de Mariah DaSilva
Located on the 5th floor of the Tahoe Tower, Renown’s newly updated Level III Neonatal Intensive Care Unit (NICU) is decorated with colorful artwork on the walls, the lights dim for the newborns resting, and parents conversing next to the bassinet with nurses on their baby’s journey to health. In the quiet, shuffling hallways stands Mariah DaSilva, a Renown NICU Nurse, whose own birth story showed her true compassion and professional dedication to what it means to care for the tiniest and most vulnerable patients. From the Medical Floor to the NICU Mariah started her nursing career on the medical floor at Renown; however, after a year, she was excited to see her dream job open in the NICU and helping to provide compassionate care for the most fragile patients. “I’ve always known that I wanted to work with babies so being a NICU nurse was a dream of mine,” said Mariah. “I truly love what I do, and I can’t imagine being anywhere else than the NICU.” A high-stakes environment, the NICU is where babies are transferred to after birth when they require medical intervention. They care for babies as young as 23 weeks gestation, up to full-term babies. Any babies born less than 35 weeks are automatically admitted into the NICU for treatment. Other than prematurity, babies can be admitted to the NICU for respiratory distress, low blood sugar (hypoglycemia), cardiac anomalies, birth defects, seizures and other medical conditions that need treatment or assessment. A Day in the NICU: The Heart of Care A typical day for Mariah starts with reviewing her assignments and receiving a detailed report from the night shift. Preparing for the day involves scrubbing in and wiping down patient care areas to maintain a clean environment. Once everything is set, she begins a series of scheduled care tasks, which include performing assessments, feeding, changing diapers and facilitating parent involvement in their baby’s care “There are so many exciting ‘firsts’ that happen in the NICU; parents holding their baby for the first time, parents' first time changing their baby’s diaper, bathing their baby for the first time, first time breast-feeding or bottle-feeding, the baby’s first time taking a full bottle, watching a baby breathe on their own without any respiratory support, etc.,” said Mariah. “There are so many big milestones that happen in the NICU that I am so incredibly lucky to be a part of.” The NICU nurses work closely with neonatologists, nurse practitioners, respiratory therapists, speech therapists, physical therapists, occupational therapists and other specialists to deliver comprehensive care. This teamwork and collaboration ensure that each baby receives the best care possible for their health journey. Mariah shared a reflection on her team: “Our NICU team is amazing. Being a part of a team that is so compassionate and collaborative is amazing. We all work closely together to ensure we’re providing the best care possible for every single baby that comes to the NICU. We are all very protective of the babies that we care for in the NICU and truly want the best outcomes for them and their families. Taking care of such a vulnerable population comes with a lot of responsibility and we take pride in what we do each day.” As with all healthcare professionals, NICU nurses require immense strength and compassion to care for the youngest patients in a highly sensitive environment. “More often than not, we have really good days in the NICU, but we also have really hard days that affect every single person in the NICU,” said Mariah. “The loss of a baby, delivering bad news to a parent, an extended NICU stay and a baby withdrawing from drugs are all situations that we unfortunately deal with in the NICU. These situations are all very challenging, but we have to stay strong for the babies and their families.”
Read More About From Renown NICU Nurse to NICU Mom: Mariah DaSilva’s Inspiring Journey
-
Un viaje de apoyo: Cómo las subvenciones de la Sociedad Americana contra el Cáncer afectan a los pacientes en Renown
For many cancer patients, a significant hurdle is simply getting to treatment. Patients from Nevada and California often face considerable financial and logistical challenges when traveling for care. Limited resources for transportation and lodging can result in missed appointments, treatment interruptions and delays in follow-up care. To address this crucial need, Renown Health Foundation partners with the American Cancer Society (ACS) to ensure our patients can access the care they need by reducing financial barriers many patients face ACS awarded $70,000 to Renown Health Foundation last year. These funds, distributed as gas cards and lodging support to qualifying patients, have proven to be a lifeline in assisting those in need. Fueling Hope with Gas Cards Through our partnership with ACS, Renown supported 128 cancer patients over the past year. This assistance provided 2,260 round trips, ensuring that patients from Nevada and California could attend their critical treatments at the William N. Pennington Cancer Institute at Renown. These patients, aged 15 to 94, traveled up to 320 miles, sometimes from remote areas such as Tonopah, Elko and Susanville, for their cancer care “We're deeply committed to supporting our patients through every step of their journey, and our partnership with the American Cancer Society is instrumental in making that happen,” said Jocelyn Mata, Oncology Social Worker at the Pennington Cancer Institute. “Without them, we wouldn't be able to provide the crucial financial assistance that many of our patients need.” Jocelyn works with qualifying patients to provide gas cards and accommodations at The Inn at Renown, a hotel at Renown Regional Medical Center. She ensures they can focus on their treatment without worrying about the financial burden. Lodging Support for Peace of Mind Along with transportation aid, we can provide safe and comfortable lodging for qualifying patients. "We encourage patients to rest and, if they have a long journey home, to stay overnight," said Dr. Max Coppes, Director of the William N. Pennington Cancer Institute. "Providing lodging support ensures they have a safe and comfortable place to recover before making the trip back." This assistance is crucial for those who travel far from home, allowing them to focus on healing without the added stress of finding and affording accommodation.
-
Las piezas del rompecabezas: Thonet LaBadie’s Breast Cancer Journey
“A breast cancer diagnosis begins much like a jigsaw puzzle to be worked through. It’s an overwhelming mess of scattered pieces that make no clear sense, poured out of the box into a crumbling pile of confusion. But slowly with persistence, focus, determination, a positive attitude and working through the challenges day by day and piece by piece, they in time both become whole and beautiful again.” – Thonet LaBadie On Feb. 13, 2015, Thonet’s life as she knew it took a drastic turn. In just one moment, everything shifted. The happy and healthy wife, mother of 17-year-old twins, former teacher and immunization specialist was about to face the fight for her life. That fateful day nearly a decade ago was when she received the unsettling news: she had breast cancer, and it had metastasized to her lymph nodes. Though she was faced with a daunting diagnosis, Thonet’s positive spirit and zest for life never wavered. Never did she think, “why me?” Nor did she think, “I’m not strong enough.” Her thought process was quite the opposite – “I am going to ride this rollercoaster until it stops, and I walk away cancer free.” With her loving family and friends rallying behind her, as well as her expert Cancer Care teams at Renown Health and Cancer Care Specialists (formerly known as Reno Oncology Consultants), Thonet knew that her journey would not be traveled alone, and she was determined to defeat cancer once and for all. She promised her daughter Jourdyn she would stay strong and not give up the fight. The Unexpected Discovery Thonet did everything she believed was right in her preventative healthcare journey. She lived an active lifestyle, she filled her life with love and happiness, she did not have any genetic markers for breast cancer and never missed a preventive check-up. Someone like her shouldn’t develop such a debilitating disease, right? As it turns out, she was told by professionals that with this disease, it’s become more often not about who develops breast cancer – but when. Breast cancer makes up for about 30% of cancer diagnoses in women across the U.S. So, when Thonet felt a lump in her breast in Nov. 2014, she knew she had better play it safe than sorry. She took her concerns to her doctors, who ran all the necessary tests. The unfortunate result: invasive ductal carcinoma (stage 2B), the most common form of breast cancer. Though Thonet was terrified, she was also tenacious. She was ready to Fight the Good Fight right then and there. Thonet chose to undergo a bilateral mastectomy. So that’s precisely what she did in April 2015 at Renown Regional Medical Center. Thonet was ready to put breast cancer behind her, but unfortunately, the trek was just beginning. During her mastectomy, her care team tested her lymph nodes. Four were removed. What came next was her most valiant fight of all: chemotherapy coupled with radiation, as well as more reconstructive breast surgeries along the way. Courageous Connections With 36 radiation treatments, 8 rounds of chemotherapy, 6 surgeries and 1 brave spirit, Thonet's healthcare journey has been nothing short of vigorous. Fortunately, she had an expert oncology team on her side every step of the way. And it goes even further – Thonet’s college acquaintance Dr. Jennifer Sutton, an oncology physician at the William N. Pennington Cancer Institute (formerly the Renown Institute for Cancer), was her radiation oncologist. She felt comfort knowing that a significant aspect of her care was in the hands of a trusted physician and a team of loving nurses, cancer care navigators and radiation therapists, whom she calls the “Renown Radiation Rockstars.” Thonet felt an immense connection not only to her warm and welcoming care team but also the other oncology patients she met along the journey. Patients facing cancer often receive radiation treatments several times a week, so Thonet had a chance to make close relationships with the other patients who were on a similar path as she was. Throughout her treatment process, Thonet participated in cancer support groups, which she believes are vital for anyone diagnosed with the disease. “Had it not been for my diagnosis, I would have never met all the amazing people I did at Renown and beyond,” she recalls. “At the end of my treatments, I knew I was going to miss them.” The love and support of Thonet’s care team, fellow patients, family, friends and community helped her remain positive throughout the entire process, always focusing on the positive – even during the most physically and emotionally tolling parts of treatment. Crossing the Finish Line Every day brought a new obstacle to overcome, whether it was a treatment, a side effect or an emotional response to the intense journey. Thonet’s motto throughout it all was “day by day, one foot in front of the other, from start to finish.” In Dec. 2016, Thonet finally made it to that finish line. With the completion of chemotherapy and radiation behind her, she walked out the front doors of the Pennington Cancer Institute, threw her fist in the air in excitement and finally got to revel in the fact that she had her health back. She had survived. Inspired by her journey and her breast cancer “sisters” she met while in treatment, Thonet wanted to give the same level of care and attention she received back to her fellow community members battling cancer. She proudly serves as a breast cancer “angel,” offering comfort and support to those who need it most. Thonet is also looking forward to the completion of the Pennington Cancer Institute’s Conrad Breast Center, currently under construction at Renown South Meadows Medical Center, noting how important it is for breast cancer patients to have expanded access to crucial cancer care in south Reno. Today, at nine years cancer-free, Thonet is thoroughly enjoying her life. She loves traveling, spending time with family and seeing her now-adult son and daughter thrive in their own lives. She also recently underwent hip replacement surgery and is proud to be back on her tandem bike with her loving husband of 33 years, Mike, who she credits for his never-ending support in sickness and in health. “No looking back – only forward to healthy living. Onward!” Thonet exclaims. And for anyone out there going through cancer treatments, Thonet has some words of wisdom to take to heart: “Cancer chose the wrong person when it tried to tackle us. Stay strong and fight on, day by day. On even the most difficult, darkest day, remember that you are stronger than you know.”
Read More About The Pieces of the Puzzle: Thonet LaBadie’s Breast Cancer Journey
-
Conozca a Haley Longfield: Un terapeuta de radiación y corredor de barril reconocido
Many Renown Health employees have deep roots in the northern Nevada community and Haley Longfield is one of them. She’s a fifth-generation northern Nevadan currently living in Fernley and commuting to Reno three days a week for her job as a Radiation Therapist for the William N. Pennington Cancer Institute at Renown Health. She’s also a wife, mother of a 1-year-old, and an avid horseback rider who enjoys the western way of life. This year, Haley is excited to compete in the Reno Rodeo for a second time. A Life-Long Passion Haley started riding horses in the fourth grade and quickly fell in love with it. A few years later, she started barrel racing and developed a profound love for the adrenaline-filled sport. “When I turned 18, my dad gave me all of the responsibility of owning a horse,” said Haley. “Ever since then, I’ve been paying for and taking care of my own horses.” As many who know and love horses would likely agree, Haley says they are therapeutic for the mind, body and soul. “Riding horses is a great way for me to use my brain and focus, or think about nothing at all,” said Haley. Recently, Haley qualified to compete in this year’s Reno Rodeo in barrel racing with her 7-year-old mare named Hershey. “The first time I competed in the Reno Rodeo was quite a few years ago with my high school rodeo horse, and Hershey is the granddaughter of that horse,” said Haley. “The thing that I’m most excited about in competing at this year’s Reno Rodeo is getting to ride a homegrown horse in my hometown rodeo – she’s gorgeous, easy-going and gives it her all.” Above: Haley Longfield on her horse Hershey at a barrel race Circle of Support Haley feels grateful to have the support of her family, friends and team at Renown. “In addition to my family and friends, I have an incredible team at Renown that cheers me on both in my professional and personal endeavors,” said Haley. “I couldn’t do it all without them.” Alongside qualifying for the Reno Rodeo, Haley also recently received her bachelor's degree in applied science with an emphasis in radiation therapy. Her career development goals consist of moving into leadership within her department. “My leader and team have been nothing but supportive of my goals. Our leader is invested in everyone’s personal development and aspirations, as well as our professional and career development,” said Haley. “I’m excited to one day follow in my leader’s footsteps and help employees in our department reach their own goals. I aspire to become a great leader like she’s been to us.”
Read More About Meet Haley Longfield: A Renown Radiation Therapist & Barrel Racer
-
Departamento destacado: Programación de cirugías y procedimientos
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
Lo que necesita saber sobre el ahogamiento por agua fría
Northern Nevada's stunning lakes, including Lake Tahoe, with its average summer water temperature of 50 degrees, present a potential risk of hypothermia. Unlike mild 50-degree air, water at the same temperature poses severe, life-threatening risks, including rapid-onset hypothermia and drowning. Awareness of the symptoms and taking proper precautions are crucial to prevent cold-water drowning. The 4 Phases of Cold-Water Drowning 1. Cold Shock Response: This response affects breathing and happens within the first minute. An automatic gasp reflex occurs in response to rapid skin cooling. If the head goes below water, water may be breathed into the lungs, resulting in drowning. A life jacket will help keep your head above water during this critical phase. Additionally, hyperventilation, like the gasp reflex, is a response to the cold and will subside. Panic will make this worse, so the key is to control breathing. 2. Cold Incapacitation: This response occurs within the first five to 15 minutes in cold water. In order to preserve core heat, vasoconstriction takes place decreasing blood flow to the extremities to protect the vital organs. The result is a loss of movement to hands, feet, arms and legs. Unless a life jacket is being worn, the ability to stay afloat is next to impossible. 3. Hypothermia: Important to note, it can take 30 minutes or more for most adults to become hypothermic. So there’s time to take action and survive. Keeping panic at bay is critical, as you have more survival time than you think. Symptoms include: Shivering Slow and shallow breathing Confusion Drowsiness or exhaustion Slurred speech Loss of coordination Weak pulse 4. Circum-rescue Collapse: This experience can happen just before rescue and is not well understood. Symptoms range anywhere from fainting to death. Some experts believe an abrupt drop in blood pressure may cause this final stage of cold water drowning, post-rescue. Additional Safety Tips and Helpful Resources Always wear a personal flotation device as well as a wetsuit or drysuit. Your personal flotation device is the most important piece of water safety gear. Try not to panic as the first phases will subside. Controlled breathing is to staying calm. Research suggests the body can withstand the cold longer than we think. The Heat Escape Lessening Posture (HELP) is a position which helps conserve energy if you’re wearing a personal flotation device. By hugging your knees to your chest, this posture helps maintain body heat for some time.
Read More About What You Need To Know About Cold Water Drowning
-
¿Qué es el síndrome de ovario poliquístico (PCOS)?
Dr. Carilyn Hoffman with Renown's Women's Health explains the symptoms, causes and treatments of Polycystic Ovary Syndrome (PCOS) (also referred to as Polycystic Ovarian Disease (PCOD)), a prevalent condition among women of reproductive age that influences hormonal balance, metabolism and fertility. Make an appointment with Renown Women's Health Click here to schedule Call to schedule: 775-982-5000 PCOS Defined PCOS is a constellation of symptoms characterized by two of the three criteria: multiple small cysts on the ovaries visible via ultrasound, irregular periods and signs of hyperandrogenism. Other symptoms include infertility, insulin resistance, and increased risk of cardiovascular disease. Symptoms of PCOS The symptoms of PCOS can vary from woman to woman, but some of the most common include: Irregular menstrual cycles: This is often one of the first signs of PCOS. Women may experience fewer than nine periods a year, more than 35 days between periods, frequent spotting, and/or abnormally heavy periods. Excess androgen levels: High levels of male hormones may result in physical signs such as excess facial and body hair (hirsutism), severe acne and male-pattern baldness. Polycystic ovaries: Enlarged ovaries containing numerous small cysts can be detected via ultrasound. Causes and Risk Factors The exact cause of PCOS is unknown, but several factors may play a role: Genetic predisposition: A family history of PCOS increases the risk. Insulin resistance: High insulin levels might increase androgen production, causing difficulty with ovulation. Obesity: Women with elevated BMI’s are more likely to have PCOS, although 20% of women with PCOS are not obese. Diagnosis and Treatment Dr. Hoffman outlines that diagnosing PCOS requires a medical history review, a physical exam, blood work and an ultrasound to evaluate the ovaries. Treatment options can range from lifestyle modifications, like diet and exercise and weight loss, to medications for menstrual regulation, fertility assistance, and rarely surgery. Lifestyle Changes A healthy lifestyle is a cornerstone of managing PCOS. Regular exercise, a nutritious diet, and weight management can help reduce symptoms and the risk of long-term health issues. In overweight patients, weight loss as little as 5% has been shown to improve symptoms of PCOS. Medication Medications may include hormonal contraceptives to regulate menstrual cycles, anti-androgens to reduce hair growth and acne, and Metformin to address insulin resistance. Fertility Treatment For women with PCOS who are trying to conceive, ovulation induction with clomiphene or letrozole is sometimes necessary. Sometimes a referral to a reproductive endocrinologist and infertility specialist is needed for more advanced technologies like IVF. Health Implications PCOS is not just about cystic ovaries or irregular periods; it can have profound implications on a woman's overall health. Women with PCOS are at an increased risk for several conditions, including type 2 diabetes, high blood pressure, heart disease, and endometrial cancer.
-
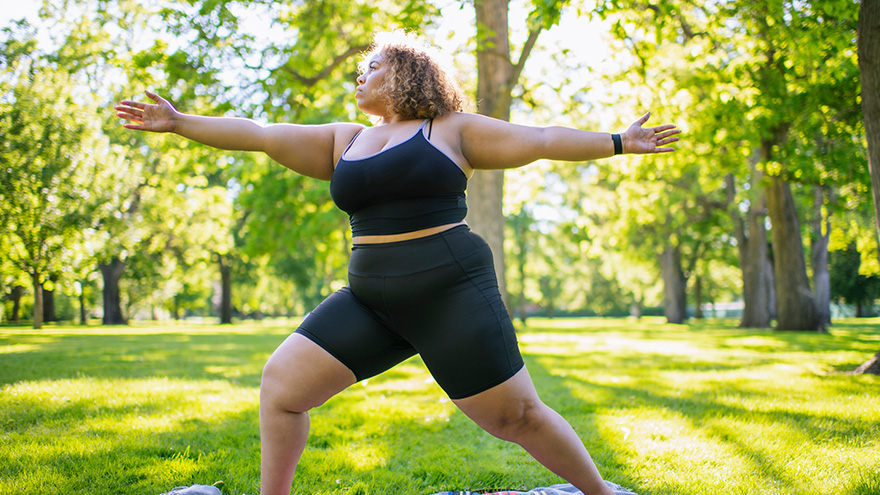
Estrategias para una pérdida de peso duradera
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
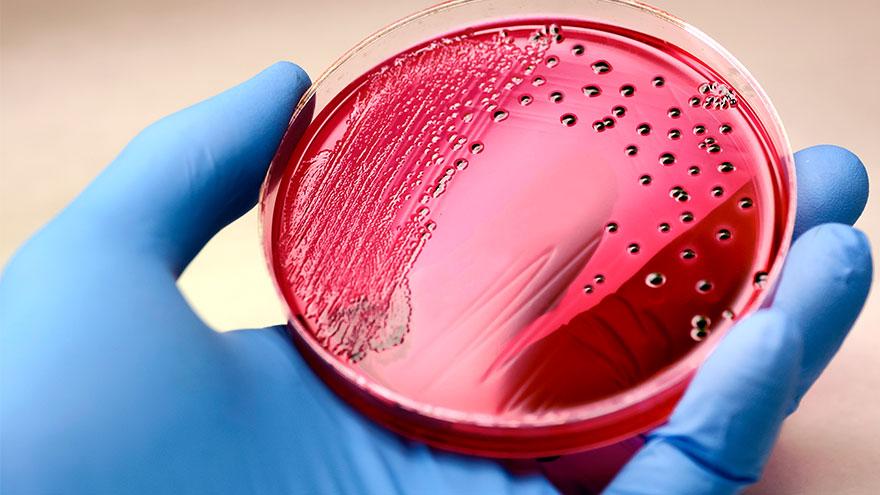
Septicemia: Causas y síntomas
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Importancia del sueño seguro
In today's fast-paced society, it is understandable for parents to want to take shortcuts in caring for their little ones. A s a result, It is tempting to leave a sleeping infant in a car seat or swing after a long day of errands or when you need a moment to catch your breath. But, as convenient as these devices may be, they pose a serious risk to your child's safety. Why Car Seats and Swings Pose Risks for Infant Sleep Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The American Academy of Pediatrics (AAP) states that “infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical.” If a parent must use a car seat or other sitting device, they should only do so for a short period of time and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The American Academy of Pediatrics (AAP) warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. This is because infants can easily slump over or become entangled in the straps, blocking their airway, and causing suffocation. Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The AAP states: Infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical. If a parent must use a car seat or other sitting device, they should only do so for a short period and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The AAP warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. In addition, infants can easily slump over or become entangled in the straps, blocking their airways and causing suffocation.
-
¿Qué hace una doula?
If you’re expecting a new baby, you may have been given the advice to hire a doula. You may have seen statistics of improved outcomes among those who’ve had a doula attend their birth. Perhaps you’ve heard that the etymology is from the Greek word meaning “to serve.” But how does a doula serve their clients? A doula is a non-medical birth professional who will guide you through labor, birth, postpartum and beyond. Your doula can discuss your options with you so you can make informed decisions, as well as provide emotional and physical support to ease your experience. While each doula offers their own style, there are certain services that most doulas will provide for their clients. Typically, a birth doula will provide at least one prenatal visit, one postpartum visit and continuous support during active labor. A postpartum doula usually provides support during the 12 weeks immediately following birth, sometimes referred to as the “fourth trimester,” but some will continue care after that as well. Simply put, a doula provides informational, physical and emotional support during the childbearing year(s). Let’s take a closer look at these three ways a doula can support you. The Basics If you don’t know your options, you don’t have any. This is a common phrase in the world of birth work. When you’re in labor, you’re exhausted, in pain and there’s often urgency inherent or implied in any choices you make. So, when an intervention is offered, many birthing people accept it without question. One method that can help the decision-making process is to check your BRAIN: Benefits: What are the benefits of the proposed intervention? Risks: What are the risks of the proposed intervention? Alternatives: What are the alternative options? Intuition: What does your intuition tell you? Nothing: What if we do nothing? What if we wait? When you’re in active labor, you might have difficulty remembering this acronym; that’s where your doula comes in. At your prenatal visits, you can ask your doula for guidance in preparing your birth plan, which can include contingencies for certain potential interventions. And as choices arise during labor, your doula can guide you through the benefits and risks and can provide you with alternative options you might not otherwise be aware of that are available to you. Your doula can remind you to check in with your intuition and can help you quiet your mind so you can listen to your instincts. The Body Although we tend to see depictions of people giving birth on their backs with their feet in stirrups, this is only one of many ways to give birth. Walking and dancing can speed up early labor. Side-lying or hands-and-knees can prevent tearing during the pushing stage. Sometimes labor stalls, and a change of position is often helpful to get things moving again. Your doula can suggest positions depending on your stage of labor. Some labor positions might require the support of another person – your doula could fill this role or assist your partner in doing so. Some doulas also provide massage or even acupressure, and most will do the “hip squeeze” that so many laboring people swear by. If your baby is presenting posterior, or “sunny side up,” your doula can apply counter pressure to alleviate back pain during labor. Some postpartum doulas will do light housework while you rest and bond with your newborn. Others might care for your baby through the night so you can catch up on sleep. Many doulas have also gone through additional training to offer breastfeeding support and may be able to assist you with latch issues and nursing positions. The Mind Pregnancy, birth and postpartum periods can be some of the most emotional times in a person’s life. A doula will hold space for you and help you process your emotions before and after birth. It’s normal to feel apprehensive, or even fearful, about labor and birth, and discussing these feelings is the first step. A doula can help you navigate your concerns in a safe space so you can be prepared emotionally for your upcoming labor. Many doulas will also guide you through writing your birth plan, which can lessen anxiety about the unknown. If you have a history of trauma, your doula can assist in communicating this, so you don’t have to relive the experience every time you meet a new medical provider. Most people will experience some form of what’s often called the Baby Blues in the immediate postpartum period. The third day after birth tends to hit hard, as hormones attempt to regulate, but the Baby Blues can continue for weeks for some new parents. A postpartum doula’s support can be incredibly valuable during this time. When the baby blues last longer than a few weeks, it could considered a mood disorder. Most doulas will recognize signs of postpartum mood disorders and will have resources available for additional support. Choosing the Best Doula for You With so many wonderful doulas in northern Nevada, you might wonder how you could ever choose just one to attend your birth. Some expectant parents are unfortunately restricted by cost. With so many expenses related to a new baby, it can be difficult to budget doula services as well. Thankfully, Nevada Medicaid now covers doula care, and some commercial insurances are following suit. Check with your insurance company to find out if they might cover part of the cost for hiring a doula. If your insurance doesn’t cover doula services, some doulas offer a sliding scale based on income. You may want to interview multiple doulas to find the right one for you. If you’re the kind of person who wants all the information you can get, a more detail-oriented doula might be the best choice. But if you tend to feel overwhelmed by too many options, you might prefer a doula who only offers additional information as the situation calls for it. If you want massage or acupressure during labor, you might want to hire a doula with those certifications. Or maybe informational and physical support are not as important to you as emotional support, in which case your best choice could be a doula who has experience with postpartum mood disorders or trauma support. Regardless of who you hire, be sure to clearly communicate your desires and expectations – not just for your birth, but also for your doula. The most important thing when choosing your doula is trusting your gut. You need to feel comfortable with your doula, as they’ll be tending to you at one of the most vulnerable times in your life. When you find a doula that you click with, who listens to you and supports your choices, you have found the best doula for you.
-
Los 5 principales beneficios para la salud de Pickleball
Over the past couple of years, pickleball has become the fastest-growing sport among people of all ages. It’s a combination of tennis, ping-pong and badminton that originated in 1965. This sport can be played indoors or outdoors on a pickleball court where two players (singles) or four (doubles) hit a perforated hollow plastic ball over a 36-inch-high net using solid-faced paddles. A pickleball court is the same size as a double’s badminton court and measures 20×44 feet. Pickleball is a fun, low-impact game that keeps people healthy and active. Kaitlyn Jacobson, Physician Assistant at Renown Urgent Care – Ryland, plays pickleball herself and is a big fan of the sport. Here she shares the top five health benefits of playing pickleball.