Buscar
-
A Therapist's Tips to Prevent and Manage Osteoporosis
Want to know more about osteoporosis and osteopenia? We'll dive into these conditions and give you some handy tips on preventing future problems and taking care of your bones. What is Osteopenia? Osteopenia (low bone density) is the initial stage of bone mineral density loss, which can eventually progress to osteoporosis if steps are not taken to prevent it. What is Osteoporosis? Osteoporosis is a condition that weakens our bones. While it literally means “porous bone," it doesn’t mean that our bones are doomed to succumb to the changes that can happen to us silently over time. Our bones are living tissues that are constantly breaking down and remodeling themselves. Osteoporosis and osteopenia are typically diagnosed by testing bone mineral density using scans that your primary care provider can easily order. This is important testing because it dictates your risk of breaking a bone in common areas like your hip, wrist or spine. It also helps set the stage for talking with your healthcare team to develop a treatment plan. Most people will reach their peak bone mass in their mid to late twenties. There are several factors that increase our risk of osteoporosis or osteopenia as we age, such as menopause, genetics and other lifestyle factors. However, there are several things you can do to mitigate this breakdown and assist your body in the constant remodeling it does to our bones. 3 Controllable Factors to Build Strong Bones 1. Talk to your primary care provider They can go over a plan and prescribe things such as vitamin D, calcium and medications that can help if you are at risk or have osteoporosis or osteopenia. 2. Maintain a healthy diet Talk to a dietician if you need further help as they can be an invaluable resource to develop a plan. Eat foods rich in calcium, vitamin D and vitamin C. These assist with the rebuilding of bone. Examples include but aren’t limited to leafy greens, legumes, salmon and healthy dairy products. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per week. Alcohol interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. 3. Exercise Talk to your primary care provider to get a referral to physical therapy if you need help with exercise. Our bones adapt to the stresses we put them through. Therefore, exercise should be tailored to putting the right stress on our bones. There is good quality research that most exercise is safe when dealing with less bone mineral density. The exercises should be progressively challenging and increase the load for resistance and weight training at least two to three days a week. Examples include squats, step-ups, chest presses and rows. Exercises higher in velocity will lead to more power and bone adaptation. Examples include quicker push-ups, marching and quicker walks. Exercises that are weight-bearing will lead bones to adapt to the stress placed on them. Movements such as mini stomps, step-ups, jumping, jogging and so forth may be used depending on how your body tolerates these things to really stimulate bone adaptation. There are aspects of aging and bone health we can’t control, but we can take steps to minimize the chances of bone loss and osteoporosis. Talk to your healthcare team to determine your risk and don’t forget to show your bones a little TLC – you’re going to need them.
Read More About A Therapist's Tips to Prevent and Manage Osteoporosis
-
COPD Explained: Protecting Your Lungs and Managing Symptoms
COPD (chronic obstructive pulmonary disease) is a progressive lung condition often mistaken for typical aging signs, like shortness of breath and coughing. While smoking and pollution can contribute to its development, lifestyle changes and medications can help manage its progression. Diagnosis typically involves lung function tests, chest X-rays, or CT scans, with treatments available through a pulmonologist or primary care provider. Renown’s Pulmonary Rehabilitation Program offers insights into living with COPD. What is COPD? According to the COPD Foundation, it is an umbrella term used to describe progressive lung diseases including: Emphysema: Damage to the small air sacs in the lungs (alveoli). Chronic Bronchitis: Irritation and swelling of bronchial tubes, causing shortness of breath and coughing for long periods of time. Asthma (non-reversible): When asthma medications cannot reduce swelling in the airways. COPD Risk Factors Smoking is the most significant COPD risk factor, and the American Lung Association (ALA) says it accounts for nearly 90 percent of cases. If you are a smoker, it is essential to seek help and quit. Other COPD risk factors include: Air pollution Genetics Second-hand smoke Chemical, fumes or dust in the workplace How Can You Protect Yourself? Stop smoking Renown Health provides support offering 4-week Smoking Cessation Virtual Classes, free of charge! Sign up today. Use natural cleaning products Many household chemicals, especially those containing bleach, can irritate the lungs – a condition called, chemical pneumonitis. Stay away from all types of smoke This includes smoke from fireplaces. Likewise, plan to stay indoors when it is smoky outside, or air quality is poor. Get active Of course, it’s never too late to start an exercise program. When exercising your heart pumps, circulating your blood and sending oxygen to every part of your body. Notably it strengthens your lungs, making it easier to breath. Talk to your doctor to see if you are healthy enough to begin exercising. Eat a healthy diet Surprisingly what you eat can affect your breathing. The American Lung Association encourages those with COPD to watch their sodium intake, eat smaller, more frequent meals (instead of three large ones), limit high fat foods and drink plenty of water. Avoid scented products Perfumes, aerosol sprays and plug-in air fresheners can trigger flare-ups. Get a flu shot Did you know chronic lung conditions, as well as, heart disease, cancer and diabetes, can be made even worse by the flu? Now is the time to get your flu shot for the season if you haven’t already. Renown’s Pulmonary Rehab staff is certified through the American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR). Recently, Renown Regional Medical Center successfully completed a disease specific COPD certification survey by The Joint Commission. For two accreditation cycles in a row, the COPD Program has had zero findings during the rigorous survey.
Read More About COPD Explained: Protecting Your Lungs and Managing Symptoms
-
Celebrating World Lung Day in Northern Nevada
In the United States, electronic cigarettes are the most popular form of tobacco product used among high school students. Approximately 21% of Washoe County area high schoolers report current use of e-cigarettes, higher than the national average of 14% reported in the most recent national data. While often viewed as a safer alternative to traditional cigarette use, e-cigarette use, commonly referred to as vaping, exposes users to nicotine and harmful chemicals that stunt brain development, results in lung damage and harms overall health. In partnership with Reno area school principals and nurses, the Renown Health – UNR Med Clinical Research Office was able to provide this year’s World Lung Day Anti-Vaping Program to Galena High School, Robert McQueen High School and Sage Ridge School, reaching hundreds of high school students.
Read More About Celebrating World Lung Day in Northern Nevada
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Department Spotlight Clinical Research
May 20 is National Clinical Trials Day. Celebrate with us by recognizing the Clinical Research team at Renown Health! The root of every medication, treatment and procedure in healthcare can be traced back to research. From the beginning of the history of medicine, research has always played a crucial role in improving the lives of patients around the world, leaving a permanent mark on how we expand our medical capabilities to this day. Renown Health’s Clinical Research team, in partnership with the University of Nevada, Reno School of Medicine (UNR Med), are leading that effort in our very own community. As our in-house leaders of clinical trials, this team is dedicated to advancing the science of medicine to help further our bottom line of making a genuine difference in the health and well-being of the patients they serve. Trial by (Medical) Jury Every day looks different for the Clinical Research team, especially when it comes to interacting with patients, providers and “sponsors,” which are the organizations providing the treatment for the study. One fact always remains true: communication and collaboration are key, especially among the team who act as the face of this process. Meet Lisa English (pictured above on the far right in a blue shirt), a Lead Clinical Research Coordinator at Renown who serves as the study "project manager." One aspect of Lisa’s day-to-day is seeing patients through their clinical trials from start to finish. It all begins with the setup. “Before we can launch a study, there is a lot of back-and-forth dialogue between everyone involved to ensure the best fit,” said Lisa. “Sponsors will come to us with novel treatments, such as medications or devices, and the inclusion criteria that patients need to meet in order to qualify for the study. We then immediately jump into working with the providers, looking closely at the science and comparing the treatments to what is on the market already.” From there, Lisa coordinates conversations between the providers, sponsors and study teams to gauge everyone’s capacity based on the length of the study, ensuring everyone involved has the time to dedicate to the process. Next, the providers identify patients that meet the criteria for the study, and together, the team decides where the patient visits will happen and discusses any potential barriers that may affect patient retention. The budget is clearly defined at this stage, set up to make sure no patient is ever billed for medical costs incurred as a result of the study. Often, research participants are seen within the specialty clinics throughout the health system, while other times the Clinical Research Coordinators see patients at the recently centralized Clinical Research Office at Renown Regional Medical Center. This location provides an essential public-facing space for the community to learn more about clinical trials and demonstrates the breadth of resources available at Renown to sponsors to strengthen external partnerships and research funding opportunities. Once the study officially begins, team members like Lisa will set patients up for a “screening/qualifying visit.” During this appointment, she makes sure patients get scheduled for their lab work, imaging scans and anything else the provider may need to make an executive decision on whether or not the patient is a good candidate for the study. “I build it all in Epic,” said Lisa. “The study information, directions, requirements and next steps are all loaded in Epic for easy tracking. We are also required to input any notes in the sponsor’s electronic data capture website. All the information I track is inputted without protected health information (PHI), so every patient is completely anonymous.” After the patient officially qualifies, the study goes full steam ahead. Team members like Lisa and the providers receive continual updates from sponsors on the status of the study. “Throughout the entire process, I make sure patients get scheduled for everything that meets the requirements for the study,” said Lisa. “I meet with patients one-on-one to discuss their needs and concerns and ask questions about the study, organize their appointments and charts and deal with any issues or pivots that may arise. It’s very important that every patient fully understands what is going to happen with their care.” The Clinical Research department strives to serve as a care partner to patients, providers and clinics they work with. The majority of our Clinical Research Coordinators are trained phlebotomists and medical assistants, performing their own assessments such as lab draws and electrocardiograms (ECGs) to streamline the research visit process and reduce resource constraints on the clinics and health system. Lisa typically sees a couple of patients per week, depending on the study and where patients are in the cycle. Depending on the complexity of the trial, patients may see the research team only one time or several times over many years. Typically, clinical trial patients are seen in clinic every 2-4 weeks. There are many tasks required before, during and after a research visit to ensure everything runs smoothly, so Clinical Research Coordinators dedicate an average of 5-11 hours of work per patient, per visit. Regardless of patient load, each employee in the Clinical Research department – as well as participating teams across Renown and UNR Med – always step in to help each other out. According to Lisa, the environment is immensely supportive. “We have a program here at Renown to train employees who have never done clinical trials,” said Lisa. “We love seeing people get more engaged with the important work we do, and every department has been great at collaborating with us. Everyone brings a different perspective.” At the end of the study, Lisa gathers all the information and collects notes into a zip drive or paper binder for archiving. The sponsor lets the Clinical Research team, providers and patients know whether they are on the trial drug or on the placebo. The teams use the data gathered during the study to publish a report or present at conferences, promoting the critical research done to better the lives of patients in our community, and potentially, the world. “I appreciate the time everyone gives us to make sure our research is successful,” said Lisa. “It feels great to work together to make a difference, improve healthcare quality and save lives.” Behind-the-Scenes, Yet on the Frontlines The impact of research studies transcends hospital walls, and this can all be attributed to the dedication of our Clinical Research department. The constant collaboration between this team, lab science, medical assistants and providers, cardiology technologists, sonographers, finance teams and our partners at UNR Med is crucial to safeguarding the success of the studies. Devoted to keeping research close to home, Renown and UNR Med teamed up to form the Clinical Research Office (CRO) in 2021. With the strength of northern Nevada's largest not-for-profit health system and Nevada’s first medical school, this team is dedicated to giving our community access to the latest care innovations. “At UNR Med, we are working with students, residents and academic faculty; on the Renown side, we are working with clinicians and community participants,” said Amber Emerson, Manager for Community Outreach and Research Engagement for UNR Med. “Everything we do is data-driven,” added Kristen Gurnea, Manager of Clinical Research for Renown. “Our main goal is to optimize our impact and provide a community benefit for our patients. The scope of our roles in the Clinical Research office is very diverse.” To help meet the growing need locally for healthcare and cutting-edge treatment solutions, the CRO has continued to grow, expanding its research capabilities and helping bring new medications, medical devices and more to patients across northern Nevada and northeastern California. “Once upon a time, our team had only six members; today we have grown to a team of 25,” added Diana Torres, Research Resource Analyst for Renown. “We used to be considered one department, including Medical Education, and we have since branched off into our own cost center. We branched off even further and created a separate Genetics department that runs the Healthy Nevada Project. Throughout this process, the Clinical Research department was always the main point of the umbrella.” “We participate in hospital-wide outreach and marketing, and we feel this has really helped us get the word out about our department,” added Raul Arellano, Research Resource Analyst for Renown. “In fact, we doubled our clinical trial portfolio from last year.” The CRO currently operates over 100 clinical trials locally in cardiology, endocrinology, infectious disease, neurology, pediatric and adult oncology, pediatric sub-specialties and pulmonology. Behind the curtains of in-person research, the CRO is home to several experts who help turn our research studies into a reality, from budgeting and billing to barrier-breaking and building relationships. “I help with barriers patients and Clinical Research Coordinators are facing, building connections and relationships inside and outside of our health system,” said Kristen Gurnea. “I enjoy handling all the supporting pieces that are required for studies to happen.” “My role changes every day,” added Jenna Berger, Administrative Assistant for the CRO at Renown. “Some days, I’ll be helping coordinate patient stipends and going through document management to ensure we have all necessary signatures. Other days, I will be planning events – like Clinical Trials Week – for our department and creating marketing materials and fliers.” “Our day-to-day involves going over anything related to research financials,” added Diana Torres. “We handle sponsor billings, process efficiency and collecting revenue for research contracts, and we collaborate closely with our Finance department and Revenue Integrity in order to accomplish this. It’s important for us to make sure all billing on both the sponsor and patient side is taken care of, especially because patients should never receive a bill for medical services they receive for the trial. A year and a half ago, we started doing budget negotiations for research contracts,” said Diana Torres. “We are proud to help clinical teams with any training they may need on these negotiations as well as billing reviews and allocations.” Seeing patients progress during a study and transform before their eyes inspires the CRO team to continue doing what they do every day. “I’ve been here for many years, first working on the floor as an oncology nurse and transitioning to oncology research in 2005,” said Anna Winchell, Cancer Protocol Nurse for Renown. “I love getting to know the patients and seeing them progress into a healthy lifestyle.” Medical students and residents at UNR Med also play a significant role in the research process, advancing medicine by exploring causes and novel treatments for a wide range of conditions, including HIV, muscular dystrophy, gastrointestinal disorders, infectious diseases and more. Medical research at UNR Med is headed by committed research coordinators, community outreach managers, grants managers, pharmacists and physicians. “I oversee scientific review and help the physicians that come to us for those resources,” said Amil Trujillo-King, Medical Research Coordinator at UNR Med. “I guide medical students in their research protocols and help with different projects to improve research activities for both students and medical residents.” It takes a village to make clinical research happen. Because of that, the ACRO cannot thank the following teams enough for moving mountains for the future of medicine: Renown Health and UNR Med leadership for demonstrating the integrated health system’s commitment to expanding access to clinical research in our community within both the Renown / UNR Med affiliation and Renown active strategic plans. Renown Pharmacy especially Research Clinical Pharmacist Tim Morton, who supports all clinical trial medication dispensing and patient education across all clinical trials at Renown. Accounts Payable for having a huge impact on patient and employee reimbursement. Renown Medical Group for their participating providers, especially in oncology, cardiology, pulmonology, pediatrics, endocrinology and neurology, who are involved in research year after year. Marketing and Communications for helping with printed materials and raising awareness for clinical research at Renown and UNR Med. An Affiliation to Last Through the Ages A collective, shared vision of exploring community health – that is the impetus behind the affiliation between Renown and UNR Med. By leveraging resources across both institutions, the CRO has maximized their impact, giving the people of northern Nevada greater access to new interventions and treatments and promoting an impassioned culture with patients, providers, residents and medical students. “Community-based research always sat well with me,” said Amber Emerson. “As Renown and UNR Med, we have this unique opportunity to shape clinical research here in northern Nevada. We always make sure we present research in a meaningful way that speaks to the work we produce and demonstrates the opportunities we offer. After all, participating in clinical research doesn’t mean our patients are ‘guinea pigs’ – quite the opposite! They are partners in their health care, and we support them through providing access to novel treatments.” “Research is my passion, and my career has spanned broadly from grants administration to study coordination,” added Valerie Smith, Clinical Research Center Administrative Manager at UNR Med. “I am excited to be at the forefront of research frontiers in northern Nevada.” Through robust engagement and collaboration with healthcare providers, department administrators, internal research team members and leadership, the strength of this affiliation is unmeasurable. The CRO’s ultimate goal is to have clinical trials be the standard of care for every condition that Renown and UNR Med treats. Clinical research participation is all about patient autonomy, shared decision-making between patients and their providers and advancing medicine to save lives. From their beginnings as a small group of passionate researchers to their present reality as a leader in the research space in northern Nevada, their efforts do not go unnoticed. “The success of our department is inspiring,” said Amil Trujillo-King. “Renown and UNR Med supports the wellbeing of all employees and contributes directly to the growth of the department.” “When I first joined Renown in Patient Access, I didn’t realize that we had a research department; with a strong healthcare background in my family, I knew I wanted to grow in my career, and our expanding Clinical Research office was that next step,” said Raul Arellano. “With our affiliation with UNR Med, it’s especially inspiring to be able to apply what I learned as a Patient Access Representative to help further outcomes for our patients through managing our finances.” Through their unwavering commitment to research excellence and patient-centered care, the CRO will continue to pave the way for groundbreaking medical discoveries and improved outcomes for patients for years to come. “Fundamentally, we’re working to build a culture of research in our community because we believe it is the right thing to do. Our community deserves to have access to clinical trials and novel care close to home with a dedicated team to support them every step of the way,” closes Kristen Gurnea.
-
How to Talk to Your Children About Vaping
According to the Centers for Disease Control (CDC), e-cigarette use isn’t just up among adults, but it has also tripled in usage for teens. Dr. Jose Cucalon Calderon, a Pediatrics Physician at Renown Health and an Assistant Professor of Pediatrics at the University of Nevada, Reno School of Medicine, provides helpful insight into e-cigarettes and the dangers it poses to kids and teens. What Are E-Cigarettes? E-cigarettes are electronic nicotine delivery devices. e-cigarettes use liquid nicotine as an alternative to traditional smoked cigarettes. e-cigarettes contain nicotine which is an addictive substance with known toxic side effects that, when released in very high doses, that can have health consequences and causes addiction. Nicotine is described as “toxic,” but the most "toxic" part of e-cigarettes' is everything else within the E-juice. Nicotine mainly keeps people coming back for more. According to the CDC, e-cigarettes are also advertised using the same themes and tactics that have been shown to increase youth use of other tobacco products, including cigarettes. In 2021, approximately 76% of students reported exposure to tobacco product marketing through traditional sources, and approximately 74% of students who used social media had seen e-cigarette–related content. What Does This Mean for the Health My Teen? We know that nicotine can affect brain development in kids and teens, so it is important to educate your teen on the risks of exposure. If you have young children in the home, it is important to be vigilant as well. One teaspoonful of liquid nicotine can be fatal for a young child. How Do I Monitor My Teen for E-Cigarette Use? Monitoring your children can be tricky for parents. E-cigarettes can be harder to detect, unlike traditional cigarettes that were easy to detect by smell and residual odor. E-cigarette use, or “vaping,” is often associated with a dry cough or chronic throat/mouth irritation. Overall, increasing research shows strong links between mental health conditions and posterior combustible tobacco use along with increased risk of marijuana use. Nicotine is addictive, but it does not cause altered mental status like the other drugs of abuse can. All parents are strongly encouraged to talk to their children about the potential dangers of e-cigarettes. What are the health risks of vaping? Vaping devices have been on the market for a relatively short period of time, with evidence-based health effects and complications still being discovered. Vaping effects poses many harmful risks to children and teens. The risks of vaping include: Chest pain Difficulty breathing Dizziness Headaches Impaired response to infection in the airway Inflammatory problems of the airway Nausea Nicotine addiction Seizures Vomiting For more information for both parents and teens about quitting smoking or vaping, you can click here. Parents can also use this tip sheet from the U.S. Surgeon General to talk to their child about vaping. The Substance Abuse and Mental Health Services Administration free national helpline number is 1-800-662-4357 (HELP). It is available 24/7, 365 days a year offering confidential treatment referral and information (in English and Spanish). If you or someone you know is facing a substance (or mental health) problem, please reach out to them.
-
Celebrating Renown Health's Nursing Excellence Conference
Renown Health recently wrapped up the twentieth annual Nursing Excellence and Excellence in Critical Care Conferences, the conference theme was the Courageous Calling and over 400 nurses from specialty fields across the region attended to learn, reflect, build relationships and obtain continuing education units (CEUs). Celebrating The Courageous Calling During the first day of the Nursing Excellence Conference, local and national leaders presented topics including redefining resilience, documentation liability, transgender healthcare and caring for the homeless population. Among the list of impressive speakers were Chief Nurse Executive at Renown Health, Melodie Osborn, and Nora McInerny, writer and host of the "Terrible Thanks for Asking" podcast. On day two,speakers focused on the critical care specialties within nursing, including intensive care, emergency room, pediatric intensive care and neonatal intensive care. Topics covered included post-COVID-19 pulmonology with Dr. Graham, traumatic brain injuries with Dr. Demers, COVID-19 reflections with Anicia Beckwith, a discussion about "Mis C” with Dr. Healy, innovations in imaging with Dr. Rangaswamy and cardiology with Dr. Danaf. Thank you to our sponsors and raffle donors for making this event possible: Erik Olson and Larry Duncan, Jana Elliott, Melodie Osborn, Becky Haase, Lori Tuntland, Dr. Akbar, Dr. Lous, Mel Morris, Grand Sierra Resort, Renown Health Gift Shops, Renown Health Directors of Nursing, Renown Health Marketing & Communications Department, Renown Health Dermatology, Laser, & Skin Care and Renown Health Foundation. Learn more about finding purpose in the health of our community when working at Renown Health here.
Read More About Celebrating Renown Health's Nursing Excellence Conference
-
¿Está en riesgo de sufrir un derrame cerebral?
Did you know an estimated 1.9 million neurons and 14 billion synapses are lost per minute during a stroke? That’s why every second counts. Anyone can have a stroke, but your chances increase if you have certain risk factors. That’s why the best way to protect yourself or your loved ones from a stroke is to know the risks and how to manage them. You can make changes to your lifestyle to lower your risk of stroke by asking yourself the following questions: 1. Is my blood pressure normal? High blood pressure is the leading cause of stroke and the most important controllable risk factor. If you’ve had a stroke, lowering your blood pressure can help prevent future strokes. 2. Can I quit smoking? Smoking damages blood vessels, clogs arteries and raises blood pressure — doubling your risk of stroke. If you want to reduce your risk of stroke and heart attack, quitting smoking is the first step — and Renown can help you with this. Learn more: Renown Health Quit Tobacco Program. 3. Do I make time to exercise 30 minutes a day? Many studies link consistent exercise habits with lower stroke risk. Also, being overweight contributes to high cholesterol, high blood pressure, heart disease and diabetes, all increasing your stroke risk. You don’t need to run a marathon — just commit to making time to move each day. 4. Do I regularly eat processed food and sugar? Eating less cholesterol and fat, especially saturated and trans fats, may reduce the fatty deposits (plaque) in your arteries. Also, eating five or more servings of fruits and vegetables per day may reduce your stroke risk. If you are diabetic, follow recommendations to get your diabetes under control.
-
Cuidado confiable desde el hogar
Renown Health has always been on the frontlines of technological advancement, and that innovation remained unwavering during the COVID-19 pandemic. Our telehealth teams heeded the call to provide home monitoring for our patients, transforming how we provide care. The care providers at Renown successfully monitored lower acuity COVID-19 patients from the comfort of their own homes. Bernard Lee was diagnosed with COVID-19 and pneumonia, and was able to return home to continue his recovery with a home monitoring system. While at home, Bernard’s health took a turn for the worse while he was sleeping, but thanks to the continuous monitoring of Health at Home, his worsening vitals did not go unnoticed. “This monitoring system really saved my life,” Bernard said. “It was telling me that my sats were low, but I didn’t even feel the common COVID symptoms; I just felt tired.” Because of his low oxygen saturation (sats) and the continuous monitoring, he woke up to providers calling to check on him in the early morning. He was immediately transferred to the Renown Intensive Care Unit to be cared for and monitored by our expert care teams. Today Bernard is recovering, feeling great and continuously refers to the team and the home monitoring system as his guardian angels.
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
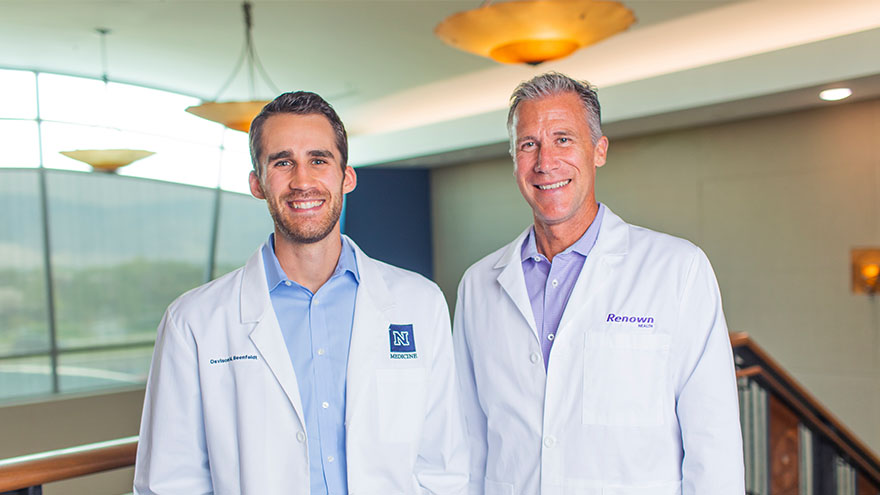
A Family's Legacy
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school
-
El camino hacia la recuperación cerca del hogar
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.