Buscar
-
De la enfermera de la NICU de Renown a la madre de la NICU: El viaje inspirador de Mariah DaSilva
Located on the 5th floor of the Tahoe Tower, Renown’s newly updated Level III Neonatal Intensive Care Unit (NICU) is decorated with colorful artwork on the walls, the lights dim for the newborns resting, and parents conversing next to the bassinet with nurses on their baby’s journey to health. In the quiet, shuffling hallways stands Mariah DaSilva, a Renown NICU Nurse, whose own birth story showed her true compassion and professional dedication to what it means to care for the tiniest and most vulnerable patients. From the Medical Floor to the NICU Mariah started her nursing career on the medical floor at Renown; however, after a year, she was excited to see her dream job open in the NICU and helping to provide compassionate care for the most fragile patients. “I’ve always known that I wanted to work with babies so being a NICU nurse was a dream of mine,” said Mariah. “I truly love what I do, and I can’t imagine being anywhere else than the NICU.” A high-stakes environment, the NICU is where babies are transferred to after birth when they require medical intervention. They care for babies as young as 23 weeks gestation, up to full-term babies. Any babies born less than 35 weeks are automatically admitted into the NICU for treatment. Other than prematurity, babies can be admitted to the NICU for respiratory distress, low blood sugar (hypoglycemia), cardiac anomalies, birth defects, seizures and other medical conditions that need treatment or assessment. A Day in the NICU: The Heart of Care A typical day for Mariah starts with reviewing her assignments and receiving a detailed report from the night shift. Preparing for the day involves scrubbing in and wiping down patient care areas to maintain a clean environment. Once everything is set, she begins a series of scheduled care tasks, which include performing assessments, feeding, changing diapers and facilitating parent involvement in their baby’s care “There are so many exciting ‘firsts’ that happen in the NICU; parents holding their baby for the first time, parents' first time changing their baby’s diaper, bathing their baby for the first time, first time breast-feeding or bottle-feeding, the baby’s first time taking a full bottle, watching a baby breathe on their own without any respiratory support, etc.,” said Mariah. “There are so many big milestones that happen in the NICU that I am so incredibly lucky to be a part of.” The NICU nurses work closely with neonatologists, nurse practitioners, respiratory therapists, speech therapists, physical therapists, occupational therapists and other specialists to deliver comprehensive care. This teamwork and collaboration ensure that each baby receives the best care possible for their health journey. Mariah shared a reflection on her team: “Our NICU team is amazing. Being a part of a team that is so compassionate and collaborative is amazing. We all work closely together to ensure we’re providing the best care possible for every single baby that comes to the NICU. We are all very protective of the babies that we care for in the NICU and truly want the best outcomes for them and their families. Taking care of such a vulnerable population comes with a lot of responsibility and we take pride in what we do each day.” As with all healthcare professionals, NICU nurses require immense strength and compassion to care for the youngest patients in a highly sensitive environment. “More often than not, we have really good days in the NICU, but we also have really hard days that affect every single person in the NICU,” said Mariah. “The loss of a baby, delivering bad news to a parent, an extended NICU stay and a baby withdrawing from drugs are all situations that we unfortunately deal with in the NICU. These situations are all very challenging, but we have to stay strong for the babies and their families.”
Read More About From Renown NICU Nurse to NICU Mom: Mariah DaSilva’s Inspiring Journey
-
Un viaje de apoyo: Cómo las subvenciones de la Sociedad Americana contra el Cáncer afectan a los pacientes en Renown
For many cancer patients, a significant hurdle is simply getting to treatment. Patients from Nevada and California often face considerable financial and logistical challenges when traveling for care. Limited resources for transportation and lodging can result in missed appointments, treatment interruptions and delays in follow-up care. To address this crucial need, Renown Health Foundation partners with the American Cancer Society (ACS) to ensure our patients can access the care they need by reducing financial barriers many patients face ACS awarded $70,000 to Renown Health Foundation last year. These funds, distributed as gas cards and lodging support to qualifying patients, have proven to be a lifeline in assisting those in need. Fueling Hope with Gas Cards Through our partnership with ACS, Renown supported 128 cancer patients over the past year. This assistance provided 2,260 round trips, ensuring that patients from Nevada and California could attend their critical treatments at the William N. Pennington Cancer Institute at Renown. These patients, aged 15 to 94, traveled up to 320 miles, sometimes from remote areas such as Tonopah, Elko and Susanville, for their cancer care “We're deeply committed to supporting our patients through every step of their journey, and our partnership with the American Cancer Society is instrumental in making that happen,” said Jocelyn Mata, Oncology Social Worker at the Pennington Cancer Institute. “Without them, we wouldn't be able to provide the crucial financial assistance that many of our patients need.” Jocelyn works with qualifying patients to provide gas cards and accommodations at The Inn at Renown, a hotel at Renown Regional Medical Center. She ensures they can focus on their treatment without worrying about the financial burden. Lodging Support for Peace of Mind Along with transportation aid, we can provide safe and comfortable lodging for qualifying patients. "We encourage patients to rest and, if they have a long journey home, to stay overnight," said Dr. Max Coppes, Director of the William N. Pennington Cancer Institute. "Providing lodging support ensures they have a safe and comfortable place to recover before making the trip back." This assistance is crucial for those who travel far from home, allowing them to focus on healing without the added stress of finding and affording accommodation.
-
Las piezas del rompecabezas: Thonet LaBadie’s Breast Cancer Journey
“A breast cancer diagnosis begins much like a jigsaw puzzle to be worked through. It’s an overwhelming mess of scattered pieces that make no clear sense, poured out of the box into a crumbling pile of confusion. But slowly with persistence, focus, determination, a positive attitude and working through the challenges day by day and piece by piece, they in time both become whole and beautiful again.” – Thonet LaBadie On Feb. 13, 2015, Thonet’s life as she knew it took a drastic turn. In just one moment, everything shifted. The happy and healthy wife, mother of 17-year-old twins, former teacher and immunization specialist was about to face the fight for her life. That fateful day nearly a decade ago was when she received the unsettling news: she had breast cancer, and it had metastasized to her lymph nodes. Though she was faced with a daunting diagnosis, Thonet’s positive spirit and zest for life never wavered. Never did she think, “why me?” Nor did she think, “I’m not strong enough.” Her thought process was quite the opposite – “I am going to ride this rollercoaster until it stops, and I walk away cancer free.” With her loving family and friends rallying behind her, as well as her expert Cancer Care teams at Renown Health and Cancer Care Specialists (formerly known as Reno Oncology Consultants), Thonet knew that her journey would not be traveled alone, and she was determined to defeat cancer once and for all. She promised her daughter Jourdyn she would stay strong and not give up the fight. The Unexpected Discovery Thonet did everything she believed was right in her preventative healthcare journey. She lived an active lifestyle, she filled her life with love and happiness, she did not have any genetic markers for breast cancer and never missed a preventive check-up. Someone like her shouldn’t develop such a debilitating disease, right? As it turns out, she was told by professionals that with this disease, it’s become more often not about who develops breast cancer – but when. Breast cancer makes up for about 30% of cancer diagnoses in women across the U.S. So, when Thonet felt a lump in her breast in Nov. 2014, she knew she had better play it safe than sorry. She took her concerns to her doctors, who ran all the necessary tests. The unfortunate result: invasive ductal carcinoma (stage 2B), the most common form of breast cancer. Though Thonet was terrified, she was also tenacious. She was ready to Fight the Good Fight right then and there. Thonet chose to undergo a bilateral mastectomy. So that’s precisely what she did in April 2015 at Renown Regional Medical Center. Thonet was ready to put breast cancer behind her, but unfortunately, the trek was just beginning. During her mastectomy, her care team tested her lymph nodes. Four were removed. What came next was her most valiant fight of all: chemotherapy coupled with radiation, as well as more reconstructive breast surgeries along the way. Courageous Connections With 36 radiation treatments, 8 rounds of chemotherapy, 6 surgeries and 1 brave spirit, Thonet's healthcare journey has been nothing short of vigorous. Fortunately, she had an expert oncology team on her side every step of the way. And it goes even further – Thonet’s college acquaintance Dr. Jennifer Sutton, an oncology physician at the William N. Pennington Cancer Institute (formerly the Renown Institute for Cancer), was her radiation oncologist. She felt comfort knowing that a significant aspect of her care was in the hands of a trusted physician and a team of loving nurses, cancer care navigators and radiation therapists, whom she calls the “Renown Radiation Rockstars.” Thonet felt an immense connection not only to her warm and welcoming care team but also the other oncology patients she met along the journey. Patients facing cancer often receive radiation treatments several times a week, so Thonet had a chance to make close relationships with the other patients who were on a similar path as she was. Throughout her treatment process, Thonet participated in cancer support groups, which she believes are vital for anyone diagnosed with the disease. “Had it not been for my diagnosis, I would have never met all the amazing people I did at Renown and beyond,” she recalls. “At the end of my treatments, I knew I was going to miss them.” The love and support of Thonet’s care team, fellow patients, family, friends and community helped her remain positive throughout the entire process, always focusing on the positive – even during the most physically and emotionally tolling parts of treatment. Crossing the Finish Line Every day brought a new obstacle to overcome, whether it was a treatment, a side effect or an emotional response to the intense journey. Thonet’s motto throughout it all was “day by day, one foot in front of the other, from start to finish.” In Dec. 2016, Thonet finally made it to that finish line. With the completion of chemotherapy and radiation behind her, she walked out the front doors of the Pennington Cancer Institute, threw her fist in the air in excitement and finally got to revel in the fact that she had her health back. She had survived. Inspired by her journey and her breast cancer “sisters” she met while in treatment, Thonet wanted to give the same level of care and attention she received back to her fellow community members battling cancer. She proudly serves as a breast cancer “angel,” offering comfort and support to those who need it most. Thonet is also looking forward to the completion of the Pennington Cancer Institute’s Conrad Breast Center, currently under construction at Renown South Meadows Medical Center, noting how important it is for breast cancer patients to have expanded access to crucial cancer care in south Reno. Today, at nine years cancer-free, Thonet is thoroughly enjoying her life. She loves traveling, spending time with family and seeing her now-adult son and daughter thrive in their own lives. She also recently underwent hip replacement surgery and is proud to be back on her tandem bike with her loving husband of 33 years, Mike, who she credits for his never-ending support in sickness and in health. “No looking back – only forward to healthy living. Onward!” Thonet exclaims. And for anyone out there going through cancer treatments, Thonet has some words of wisdom to take to heart: “Cancer chose the wrong person when it tried to tackle us. Stay strong and fight on, day by day. On even the most difficult, darkest day, remember that you are stronger than you know.”
Read More About The Pieces of the Puzzle: Thonet LaBadie’s Breast Cancer Journey
-
Conozca a Haley Longfield: Un terapeuta de radiación y corredor de barril reconocido
Many Renown Health employees have deep roots in the northern Nevada community and Haley Longfield is one of them. She’s a fifth-generation northern Nevadan currently living in Fernley and commuting to Reno three days a week for her job as a Radiation Therapist for the William N. Pennington Cancer Institute at Renown Health. She’s also a wife, mother of a 1-year-old, and an avid horseback rider who enjoys the western way of life. This year, Haley is excited to compete in the Reno Rodeo for a second time. A Life-Long Passion Haley started riding horses in the fourth grade and quickly fell in love with it. A few years later, she started barrel racing and developed a profound love for the adrenaline-filled sport. “When I turned 18, my dad gave me all of the responsibility of owning a horse,” said Haley. “Ever since then, I’ve been paying for and taking care of my own horses.” As many who know and love horses would likely agree, Haley says they are therapeutic for the mind, body and soul. “Riding horses is a great way for me to use my brain and focus, or think about nothing at all,” said Haley. Recently, Haley qualified to compete in this year’s Reno Rodeo in barrel racing with her 7-year-old mare named Hershey. “The first time I competed in the Reno Rodeo was quite a few years ago with my high school rodeo horse, and Hershey is the granddaughter of that horse,” said Haley. “The thing that I’m most excited about in competing at this year’s Reno Rodeo is getting to ride a homegrown horse in my hometown rodeo – she’s gorgeous, easy-going and gives it her all.” Above: Haley Longfield on her horse Hershey at a barrel race Circle of Support Haley feels grateful to have the support of her family, friends and team at Renown. “In addition to my family and friends, I have an incredible team at Renown that cheers me on both in my professional and personal endeavors,” said Haley. “I couldn’t do it all without them.” Alongside qualifying for the Reno Rodeo, Haley also recently received her bachelor's degree in applied science with an emphasis in radiation therapy. Her career development goals consist of moving into leadership within her department. “My leader and team have been nothing but supportive of my goals. Our leader is invested in everyone’s personal development and aspirations, as well as our professional and career development,” said Haley. “I’m excited to one day follow in my leader’s footsteps and help employees in our department reach their own goals. I aspire to become a great leader like she’s been to us.”
Read More About Meet Haley Longfield: A Renown Radiation Therapist & Barrel Racer
-
20 Años de compasión y dedicación
When you meet Poeth Kilonzo, Director of Oncology Nursing at Renown Health, you are immediately greeted with a warm smile that puts your mind at ease. Within the William N. Pennington Cancer Institute, Poeth enjoys a strong reputation among her employees and patients as someone they can always rely on, no matter how rough the tides may flow. As an incredibly humble oncology professional, you may not realize that behind that smile is the power of a best-in-class nurse and leader holding a 20+ year career of diverse nursing experience and leadership excellence – dedicating the majority of her service to Renown Health. Join us as we dive into Poeth’s unique journey through Renown. Finding Her Passion Ever since she could remember, Poeth has been a “people person.” Above all else, she cared for people – and she cared a lot. What better place for her to be than healthcare? After moving to northern Nevada from Kenya, she began working in private patient care working with home health and dementia patients while taking classes at Truckee Meadows Community College (TMCC) in 2000. One day, a patient asked her a question that would change the course of her career journey: Did you ever think about becoming a nurse? Driven by not only the words of encouragement of her patients and supervisors in home health but also the rallying support from her family and friends, including her husband and high school friend, who both have decades of experience interacting with nurses in healthcare (with her husband spending many of those years at Renown), Poeth knew this was the path she was meant to take. “That was it; it was like a light switch had flipped,” said Poeth. “I switched to nursing overnight.” According to Poeth, TMCC’s nursing program offered her an incredibly supportive environment, which was especially important as she was a young mom at the time. Working in healthcare, going to nursing school and raising a family all at the same time is no easy task, but to Poeth, this was her calling. “Regardless of my path, I knew I wanted to be a nurse that was close to patients, sitting with them and holding their hand throughout their treatment,” said Poeth. During nursing school, Poeth completed clinicals at several hospitals in Reno – three of them were at Renown Health (known as Washoe Medical Center at the time). What immediately stood out to her was the passion of the pediatrics unit, especially in the neonatal intensive care unit (NICU). “While I knew that pediatrics wasn’t going to be my arena, some of the best times in my life were during my pediatrics clinical,” said Poeth. “It opened me up to how welcoming Renown is.” While doing her rotations, nursing leaders helped Poeth and her fellow classmates discover Renown’s Nurse Apprentice program, an apprenticeship designed exclusively for local northern Nevada nursing students. One of those leaders asked her, “have you considered doing a rotation in oncology?” And another light switch flipped. “Bingo. I am becoming an oncology nurse apprentice,” Poeth recalls. And that’s exactly what she did. After her four-month apprenticeship ended in February 2002, she walked into her interview with Joanna Gold, who would end up being her supervisor and one of her greatest mentors until she passed away in recent years. With her experience and enthusiastic spirit on her side, Poeth fervently expressed her passion and interest in working in oncology. And Joanna saw all of that and more. In June 2002, Poeth was presented with a two-year oncology RN contract, which she easily signed – however, she knew right then and there but she was not going anywhere. Renown was her home, and oncology ignited the fire within her. “The nurses in this unit are part of what kept me here,” Poeth remembers. “These nurses would really do anything for their patients. The commitment and love they all had for one another truly was like family. It inspired me to learn more and give even better care to my patients." To Poeth, it didn’t feel like she was coming to work just to do a job – she was following her dreams. “You don’t think about the work you do; you think about the service,” said Poeth. From there, Poeth spent three years on the floor as an oncology RN and became a night shift supervisor in 2005. She was thriving. But this part of her journey was only the beginning. When Opportunity Arises, Take It In March 2007, Poeth and her husband welcomed their third child – and for her, working a day shift position would serve her the best at her current stage of life. This revelation led her down to Renown South Meadows Medical Center, where she became a staff nurse in Medical Telemetry. It was in the telemetry unit where Poeth contributed to one of the largest digital transformations Renown would ever go through: transitioning from paper records to electronic records on EPIC. From there, Poeth was inspired to get back into leadership in 2012 as the Supervisor of Clinical Nursing overseeing nurses, clinical outcomes and payroll in the medical/telemetry unit and intensive care unit (ICU). The timing of her leadership role lined up perfectly with her decision to take her skills to the next level, achieving a bachelor’s degree from Nevada State College in 2016. The timing of her degree lined up perfectly with what was about to come; she embarked on her first leadership role at Renown This is where she would happily stay for 11 years, eventually becoming the Manager of Nursing in telemetry and the ICU, noting that Renown South Meadows felt like a second home to her. “I wore many hats at South Meadows,” Poeth recalls. “From piloting back coding and handling compliance work to being on the patient floor and heading up South Meadows’ first high school hospital volunteer program, I got very involved. We had seven years without having a single nurse traveler in our unit." It wasn’t long before Poeth was inspired to expand her education even further, and she graduated in January 2018 with a master’s degree in nursing clinical leadership from Western Governors University. Thanks to Renown’s educational assistance programs, our health system invested directly in Poeth’s education with tuition reimbursement and a $1,000 nursing scholarship. Soon after celebrating her achievement, Jennifer Allen Fleiner – who was the Director of Nursing at Renown South Meadows at the time – asked Poeth yet another question that would bring her to the precipice of another career detour: “Have you ever considered transferring from South Meadows to Renown Regional?” Moments later, Alicia Glassco, Director of Nursing for Renown Regional, asked her the same question, noting that the hospital’s neurosurgery unit needed the leadership of someone just like Poeth. “It took me a whole week to make a decision, because this was one of the toughest decisions I’ve ever made in my life,” said Poeth. “I truly loved South Meadows. After that week, my leader told me, ‘you know what, Poeth? You’ve reached your pinnacle. You need and deserve a new challenge. Learn from this new team and teach them something. I think you have a huge opportunity for growth.” So, Poeth decided to apply for the position and shadow the neurosurgery team, where unlike her unit, the majority of the team at the time were travelers. But this was a challenge Poeth was up to – so she was accepted into the role. “At the end of the day, these patients deserved consistent care,” Poeth emphasized. “I knew I had to take this position for the patients – they were the ones who sold me on this job. They are the reason why we are all here. It was important for me to be an advocate for them.” The big hills to climb didn’t slow down Poeth; in fact, the exact opposite happened. Within her first year in the neurosurgery unit, her team onboarded 18 new graduates and replaced travelers. “We were hiring like crazy,” said Poeth. “My standing agenda at all section meetings focused on hiring and our quality metrics. I started having a relationship with our doctors. Once we created a strong doctor/nurse collaboration, our nurses started staying with us longer.” Everything on the unit was going great. Then, COVID-19 hit. “Since we had private patient rooms, our unit became the first COVID unit at Renown Regional,” Poeth recalls. “My whole staff that I had built up had to be distributed elsewhere. I started caring for COVID patients. We relied on our Infection Prevention team a lot. And at the same time, I was worried about my family in Africa.” Despite the stressful nature that the pandemic brought upon health systems everywhere, according to Poeth, she knew she had to continue on. “The neurosurgery team ended up merging with orthopedic trauma, which was very difficult,” said Poeth. “We went from 28 beds to 58 beds. The key to success here was training. Nurses are very resilient, and through training, we were able to stabilize the unit.” Noticing the opportunity for virtual demonstrations that were previously offered only in-person, Poeth spearheaded online trainings for nursing, physical therapy, mobility, head injuries and more, allowing teams across Renown to upskill in safe spaces. These programs continued throughout the pandemic, and Poeth was proud to be a figurehead through it all, helping to stabilize the unit while creating strong relationships with the entire team, many of whom followed her from Renown South Meadows to Renown Regional. Then, she gets another visitor – her Chief Nursing Executive – in her office with yet another opportunity. Have You Considered... In September 2022, Chief Nursing Executive Melodie Osborn walked into Poeth’s office with those three words that Poeth has heard for decades: “Have you considered...” “Before Melodie could even finish, I thought, ‘I have considered A LOT in my career!’” said Poeth. Melodie told Poeth that the William N. Pennington Cancer Institute was looking for a Director of Oncology Nursing, noting that this could be yet another growth opportunity for her and a chance for her to go back to her roots. “I had just celebrated my twentieth year at Renown; I knew this was going to be a decision I really had to think about,” said Poeth. “Everyone believed in me. Alicia Glassco told me, ‘Poeth, you are ready for this. Go for it.’ Once I applied for the position and started getting my updated chemotherapy certifications, I thought, ‘they are right; I got this.’” At this point in her career, Poeth had been hyper-focused on inpatient care, and this role would be her first time caring for patients in the outpatient setting. After going through the interview process, however, Poeth knew that this was where she was meant to be yet again – and colleagues she hadn’t seen in years reaffirmed that commitment. “I felt the most excited about the job when I toured the facility,” Poeth recalls. “I’ll never forget what one of the infusion nurses told me on my tour. She told me, ‘I don’t know if you remember me, but I remember you; I came from Renown South Meadows, and you were so nice to me as I was precepting as a new nurse. Your kindness was unforgettable to me.’ The fact that people like her wanted me in the unit so badly inspired me to come back.” Soon enough, Poeth became the Director of Oncology Nursing, a position she still proudly holds to this day. Once she was hired, she immediately went into deep learning mode, mastering skills such as revenue integrity, credentialing and the insurance process. She attributes Supervisor of Infusion Kaitlin Hildebrand and Director of Radiation Oncology Services Susan Cox for helping her succeed. Shortly after assuming the position, Poeth noticed yet another opportunity for cross-training within the organization to combat short staffing – training nurses from the Float Pool to care for patients in Infusion Services. “Between May and July of this year, we trained six nurses from Float Pool to do infusion therapy services, which offered so much relief to my team; I am so thankful to Rendee Perry, the Manager of Nursing in our Float Pool unit, and her team for their support,” said Poeth. “My mission in outpatient oncology is to serve the staff and patient population and create those strong relationships." Poeth's efforts to circumvent nurse burnout go beyond cross-training – as a director, she is always there for her team members no matter what, leading with kindness every step of the way. “I never miss a 7:45 a.m. huddle unless I am in a ‘cannot miss’ commitment; I want my employees to always know that I am there for them and that they are cared for both on and off the job,” Poeth emphasizes. “I want them to feel like they are valued, their families are valued and their mental health is valued; after all, without my team, we cannot care for patients. It’s important for them to know that I am here to be a security blanket and that there is always something we can do to solve a problem." Today, Poeth enjoys a full team of core Renown staff members whom patients look forward to seeing – and the high patient satisfaction scores to prove it. “Our team is so established that patients feel comfort in knowing they are always going to know exactly who they are being treated by,” said Poeth. “We will always work to maintain that consistency.” Staying True to the Mission Renown’s mission of making a genuine difference in the health and well-being of our community resonates closely with Poeth. Before she arrives at the infusion unit every day, she asks herself: What can I do to make it easier for my team to deliver care? “It takes a village to deliver the care we do,” said Poeth. “Our nurses are priceless. You can’t place a monetary value on dealing with life and death every day. This is what inspires me. It’s all about helping each other out and keeping those relationships strong.” Maintaining those relationships on the floor, according to Poeth, requires one main ingredient: work-life balance. “I want my nurses to be able to balance sending their kids to kindergarten and giving their patients their first chemotherapy treatments,” Poeth emphasizes. “I genuinely care about their lives. It’s nice when you get to know your team’s children, grandkids, spouse and hobbies. I’m grateful that Renown has given us the autonomy to foster that flexible environment within our teams. It is so rewarding to have such a strong impact on these employees.” To Poeth, it’s all about doing and then duplicating. Luckily for her team and infusion patients in northern Nevada, a new infusion center at Renown South Meadows is planned to open in the coming years as part of our commitment to expanding care. Her team is excited to grow their expertise down to south Reno – Poeth's original home hospital. “I strongly believe that as nurses, we are meant to be where we are meant to be at the time,” said Poeth. “Be kind to yourself and remember your ‘why.’ Take advantage of the opportunity you have.” To all nurses (and future nurses) out there, Poeth wants you to know that you are welcomed and valued. You are saving lives every day, and to her, that is worth everything. “Always remain focused, even throughout all the challenges. Never forget why you got into nursing. And lastly, always stay true to your own mission,” closes Poeth.
-
Comprensión y manejo del asma infantil
Dr. Shipra Singh, a Pediatric Pulmonologist, outlines the challenges of diagnosing asthma in children due to symptoms resembling other respiratory issues. It's particularly difficult to identify in infants and young children, who may not clearly exhibit breathing difficulties. Asthma, often confused with bronchitis, croup, or allergies, is a significant chronic illness causing school absenteeism, as per the CDC. Risk factors include prenatal smoking and family history of allergies or asthma. Infants and toddlers are more susceptible due to smaller airways and respiratory viruses, which can exacerbate conditions like colds and bronchitis. How can I tell if my child has asthma? Unfortunately small children are unable to describe their symptoms, making asthma difficult to diagnose. Your child may even be active, playing and smiling, although they are experiencing chest tightness or labored breathing. Observe your child and let the child’s doctor know if: Your child’s breathing behavior has changed (coughing, wheezing, rapid breathing) Your child’s breathing pattern changes (day vs. night, with rest or activity, inside vs. outside) You have a family history of asthma or allergies Your child’s breathing is triggered by any foods or allergies With your help, your child’s doctor can make the best diagnosis to determine if your child has asthma. A pediatric pulmonologist (lung specialist) or pediatric allergist may also have to be consulted for special testing. Tests may include lung function testing, allergy tests, blood tests and X-rays for an accurate diagnosis. What is the treatment for infants and toddlers? Young children can use many of the same medications as older children and adults, although the way they take them and the dosage will differ. A nebulizer (or breathing machine) creating a medicated mist for your child to breathe through a mask may be used. An inhaler with a small spacer tube connected to a mask is also common to help your child breath medication into their lungs. Either of these options are effective. Asthma in children is treated with both fast-acting and long-term medicines to open up airways quickly for easy breathing and also to lessen asthma symptoms over time. Communicate with your child’s medical providers to create a personalized asthma management plan for them. How can I manage my child’s asthma? Recognize your child’s breathing habits and be aware of worsening symptoms. Consult with your child’s doctor on a daily asthma action plan to recognize worsening symptoms and track medications. Here’s an example of an asthma action plan provided by the U.S. Department of Health and Human Services’ National Institutes of Health). Be consistent with the plan and talk to your doctor before changing it. Have an emergency plan in case of a serious asthma attack. Know where the closest ER is and know who can take care of your other children. Also know what the medical treatment coverage is under your insurance plan. Dr. Singh explains, "Discussing asthma with your child may be difficult. Some kids find the subject frightening or confusing. Others, especially the older kids, may resent the treatment and may not be interested in doing it. Talk to your doctor about advice to build an open and trusting relationship regarding your child's asthma care."
-
Departamento destacado: Atención respiratoria
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Blog del empleado: Equipo reconocido en el Orgullo del Norte de Nevada
It’s July 23, 2022, and I am arriving in Downtown Reno to walk in my first-ever Pride Parade. Even more amazing, I am going to be walking with a group of my coworkers, announcing to our entire community that our employer supports us being our full and truest selves. I arrived alone, but in the staging area I met new people who worked in other departments of Renown, coworkers I might never have met if not for Pride. I even took a selfie with one of these new friends. Someone passed around flags for us to hand out to the audience as we marched by. I took a rainbow-striped temporary tattoo in the shape of the Renown “R” and used my water bottle to apply it. There was an overwhelming atmosphere of excitement and joy that can only come from gathering with other human beings who are overflowing with love. We started the Parade waving handfuls of Pride flags high and gave those flags out to the audience as we passed. By the time we were done walking, our hands were empty, but our hearts were full. I couldn’t have stopped smiling if I’d tried. I’d joined the parade as a single person, but as we walked, I became part of a community. Not only the Renown community, but a community of Proud queer people across northern Nevada. And by extension, the LGBTQIA+ community all around the world – past, present and future. With the multiple recent state laws proposing to strip away the rights of LGBTQIA+ people, many of us have felt a noticeable decline in our mental health and feelings of personal safety. As a member of the queer community, I have felt these mental health effects too. I am fortunate and privileged enough to not have experienced workplace discrimination in my current position. But before Renown, I – like so many others in the LGBTQIA+ community – had a negative experience at a previous job, and afterwards I was hesitant to share my full self while at work. To be able to walk in a Pride Parade with my current employer, healed a little bit of that past pain inflicted by my former employer. When our liberties are under attack, Pride is more important than ever. We must remind ourselves, especially when others cannot seem to remember, that we are loved and worthy of love. I am grateful to work for an organization that is willing and able to fight this good fight with us. I will certainly be back to walk in this year’s Pride Parade, and I sincerely hope to see you there too! Be sure to wear comfortable walking shoes, sunglasses and of course keep your skin safe with sunscreen. Whether you’re part of the LGBTQIA+ community, or just an ally, you are welcome.
Read More About Employee Blog: Team Renown at Northern Nevada Pride
-
¿Vive con EPOC? Cómo maximizar su experiencia de verano
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
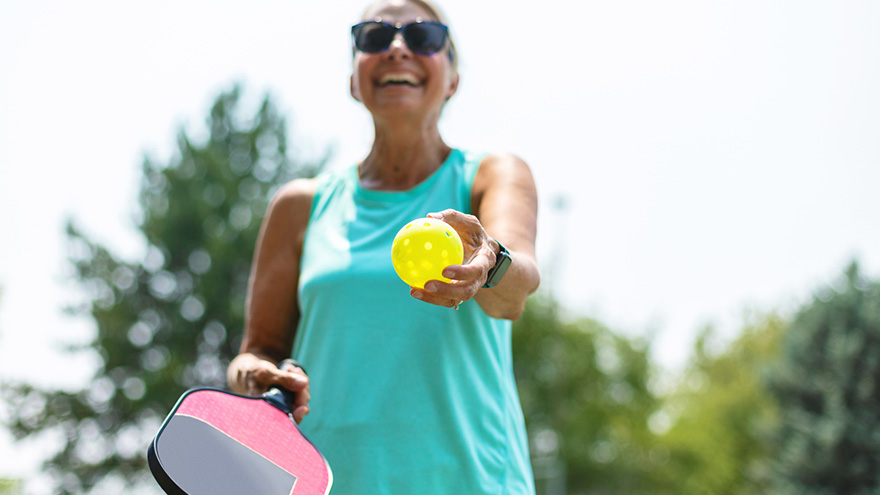
Los 5 principales beneficios para la salud de Pickleball
Over the past couple of years, pickleball has become the fastest-growing sport among people of all ages. It’s a combination of tennis, ping-pong and badminton that originated in 1965. This sport can be played indoors or outdoors on a pickleball court where two players (singles) or four (doubles) hit a perforated hollow plastic ball over a 36-inch-high net using solid-faced paddles. A pickleball court is the same size as a double’s badminton court and measures 20×44 feet. Pickleball is a fun, low-impact game that keeps people healthy and active. Kaitlyn Jacobson, Physician Assistant at Renown Urgent Care – Ryland, plays pickleball herself and is a big fan of the sport. Here she shares the top five health benefits of playing pickleball.
-
Ruta de Zarah desde el viajero hasta el enfermero del quirófano
As many nurses can attest, the journey they have taken to arrive at where they are today is full of twists and turns. For Zarah Jayco, an operating room nurse at Renown Regional Medical Center, her journey is nothing short of a fulfilling and exciting one. Zarah is no stranger to taking detours to find what truly makes her feel the bursts of passion she had been looking for her entire life. She found that passion in the operating room – and travel nursing led her to Renown Health. Today, she is a firm believer that she is exactly where she is supposed to be. “I Just Want to Help People” Throughout her life, Zarah knew she was destined for a meaningful career – but didn’t exactly know what. One day, she sat down with her mom, a nurse herself, where she asked the question that would ignite Zarah’s curiosity: What is important to you? “That’s when I told my mom: ‘honestly, I just want to help people.’” It was at that moment that she realized nursing could be a fit for her. Everything about venturing into the nursing field started to make sense. So, that’s precisely what she did. Zarah went to nursing school. When she stepped into the OR during her clinical rotation, she was immediately inspired. Zarah’s core values as a nurse were rooted from caring for her 90-year-old grandmother while she was in hospice. Her grandmother gave her some powerful lessons and words as she set off on her career: “You are in the right place.” Upon completion of her perioperative program, Zarah the OR Nurse we know and love started her journey. She began her trek as a travel nurse, going up and down California to do exactly what she was meant to do: care for surgical patients. “I Traded the Ocean Waves for the Mountains” As Zarah continued to travel and find different locations for new assignments, her husband received an opportunity for work to transfer to the Biggest Little City. The duo packed up their California lives and moved to northern Nevada, where Zarah signed up for a night shift OR nurse position at Renown Regional Medical Center. But the traveler’s mindset wouldn’t last long. Renown embraced Zarah with open arms, and she was immediately drawn into the community-feel that our health system offered. She felt welcomed and surrounded by “loving, hardworking people” across her department and all other teams she encountered. As Renown cares for patients across 100,000 square miles, Zarah was especially impressed with how rooted Renown is in northern Nevada, noting how it “truly feels like we are caring for the community” with our health system’s wide reach. She was inspired to live up to that mission and more. “Reno and Renown really reeled me in, and I fell in love with the city and everything it has to offer,” said Zarah. “I traded the ocean waves for the mountains, and the more we got to know Reno, the more we realized that this change of pace and lifestyle was definitely a good fit for us.” Zarah the OR Travel Nurse became Zarah the Renown OR Core Staff Charge Nurse. And she knew she made the right decision. Working in the OR, according to Zarah, is challenging in the best way possible. At night, all surgery cases at Renown are emergencies. The team springs into action to answer one vital question: How do we provide the best care for this patient? “It is essential for us to anticipate potential outcomes,” said Zarah. “When we book a surgical case, we look at everything to make sure we are absolutely prepared and ready.” Staying at Renown was an easy choice for Zarah. To her, there is nothing like being a part of a core team that inspires her every day and ‘has each others’ back,’” Zarah stated. “During the course of my assignment at Renown, the culture harnessed a kind of environment that felt like a hardworking family. This was the hook that reeled me into considering being part of core staff. I am incredibly grateful for the opportunity to build relationships that I hold in the highest esteem.”
-
Su mejor guía de supervivencia para el resfriado y la gripe
While viruses can attack year-round, colds, flus and other respiratory illnesses are typically more prevalent during fall and winter. People spend more time indoors, which allows viruses to pass more easily from one person to another. The cold, dry air can also affect the respiratory system, making it more susceptible to germs. According to the CDC, flu activity in the U.S. often begins to increase in October and peaks between December and February. “Flu season” can last as late as May. When it comes to the cold and flu, prevention and preparation are key. Getting the flu shot and a COVID-19 vaccine is the first and most crucial step in protecting against these two respiratory illnesses. Preventative actions, such as washing your hands, covering your mouth and nose when coughing or sneezing and getting enough sleep can also help you avoid getting sick. However, despite your best prevention efforts, the time may come this winter when you start to feel a little scratch in your throat or a fever coming on. By taking steps ahead of time to assemble a cold and flu survival kit, you’ll be more prepared for whenever illness strikes, allowing you to stay home, rest and avoid spreading germs. Tips for Managing Symptoms Keep these tips in mind to ease your cold or flu symptoms: Stay home and rest Drink plenty of fluids Treat aches and fever with over-the-counter medication such as ibuprofen or acetaminophen Manage a cough with over-the-counter expectorants or suppressants Run a humidifier or sit in a steamy bathroom to ease congestion What to Stock in Your Flu Survival Kit Be ready when a cold or the flu strikes by having a flu survival kit filled with these get-well essentials stocked in your pantry, fridge and medicine cabinet: Over-the-Counter Medications: Take advantage of over-the-counter medications to make yourself feel better and ease most common flu symptoms of fever, headache, cough, muscle aches, sore throat, and runny or stuffy nose Pain relievers - Ibuprofen (Motrin and Advil) or Acetaminophen (Tylenol): for fever and aches Decongestants: for sniffles and congestion Cough expectorant (guaifenesin): for a “wet” cough to help clear secretions from the lungs Cough suppressant (dextromethorphan/DM): for a severe “dry” cough to block the cough reflex Cough syrups and drops Drinks: Water Herbal tea Low-sugar sports drinks Pedialyte Foods: Chicken soup Broth Vitamin C-containing fruits and vegetables Oatmeal Toast (add some avocado, honey or egg) Miscellaneous items: Tissues Lozenges Protective mask Thermometer Humidifier When to Seek Care and Where to Go Most healthy adults who have a cold, the flu, or other mild respiratory illnesses don’t need to see a care provider and will recover at home with self-care measures. Because these are viral illnesses, antibiotics won’t work against treating them. Your care provider may be able to prescribe an antiviral medication that can relieve your symptoms and shorten the duration and severity of your illness; however, this needs to be started within 48 hours of symptom onset and is often only prescribed to individuals at high risk for developing complications from the flu or those experience severe symptoms. Primary Care or Urgent Care Contact your primary care provider or visit an Urgent Care if you are at an increased risk, including those who: Are 65 years of age or older Have chronic medical conditions Are pregnant or recently gave birth Have a weakened immune system Find a primary care provider If you are otherwise healthy and not at increased risk of complications, seek medical advice if your flu symptoms are unusually severe, such as mild difficulty breathing, a severe sore throat, coughing that produces a lot of green or yellow mucus, or feeling faint. Emergency Care Go to the Emergency Department if you are experiencing emergency warning signs such as severe pain (chest, abdomen), concern for heart attack or stroke (slurred speech, new localized weakness), severe dehydration (needing IV fluids) or severe shortness of breath.