Buscar
-
How to Protect Your Kids from Heatstroke
Summer is around the corner, bringing heightened risks of heatstroke, especially for children who cannot regulate their body temperature as efficiently as adults. Infants are particularly vulnerable and may not express discomfort, so never leave a child unattended in a vehicle. Top Tips for Preventing Heatstroke Reduce the number of deaths from heatstroke by remembering to ACT. Avoid heatstroke-related injury and death by never leaving a child alone in a car, not even for a minute. And make sure to keep your car locked when you’re not inside so kids don’t get in on their own. Create reminders. Keep a stuffed animal or other memento in your child’s car seat when it’s empty, and move it to the front seat as a visual reminder when your child is in the back seat. Or place and secure your phone, briefcase or purse in the backseat when traveling with your child. Take action. If you see a child alone in a car, call 911. Emergency personnel want you to call. They are trained to respond to these situations Keeping Your Baby Cool in the Back Seat In hot weather, it is crucial to keep your baby cool and hydrated by using a car seat cover or towel over them to reflect the sun's rays. Dress your baby in lightweight clothing that covers their arms and legs. Keep an eye on your baby's skin color. Move them to a cooler place if they look too red or flushed. Keep the temperature at a comfortable temperature for you, not for your child. Keep the windows cracked open for ventilation and ensure nothing is blocking the airflow from entering or exiting the vehicle. Dress your infant appropriately for their environment, including appropriate head and neck coverings, to keep them cool and protected from sunburns. Ensure you have enough fluids to last an hour before getting out of the car or use bottled water if possible. Never leave your child unattended in a car. Steps to Follow if You Suspect Heatstroke Call 911 immediately. Cool the victim – Get the person to a shady area, remove restrictive clothing and cover skin with sheets soaked in ice-water, and place ice packs in the arm pits and groin. Have the victim drink cool fluids, preferably an electrolyte-containing sports drink. Monitor body temperature with a thermometer but stop cooling efforts after temperature has dropped to 102 Fahrenheit. Baby Safe Classes These classes help prepare parents for emergencies that may occur in baby’s first year. Safe Kids Worldwide Did you know heatstroke is the leading cause of non-crash related fatalities in children? “On average, every 10 days a child dies from heatstroke in a vehicle. In more than half of these deaths, the caregiver forgot the child was in the car.”
-
Top Safe Sleep Tips for Your Baby
Becoming a parent for the first time means lots of new unknowns – from learning to breastfeed and swaddle to buckling your newborn into the car seat for the first time. But when it comes to putting them to bed safely, it’s important to remember it really can mean life or death. It’s something we’re taught before our little one is even here: the correct way to put your baby to bed safely. Sadly though, the number of infant deaths continues to climb. The main culprit of sleep-related infant death continues to be all the items parents leave in the crib with their babies. According to the Center for Disease Control and Prevention, there are about 3,500 sleep-related deaths among babies each year. “The best advice is ‘bare is best.’ Keep your infant’s sleep space clutter free – no blankets, bumpers, toys or pillows,” said Karen Wagner, Pediatric Nurse Practitioner. Follow the ABCs for Safe Sleep Remembering the ABCs is an easy way to remember how to put your little one to bed safely. A: Alone No blankets, toys or pillows. “We do recommend using a sleep sack as a blanket alternative,” said Karen. “It prevents the risk of suffocation and keeps your baby warm.” Keep in mind, the greatest risk for suffocation happens when babies are under 1 year of age, so it’s best to save the toys, blankets and pillows for their “big kid bed,” or around 18 months old. B: Back The slogan “back is best” is another good reminder. Keeping your baby on their back until they’re old enough to rollover helps reduce the risk of Sudden Infant Death Syndrome (SIDS). C: Crib It is best to have your baby sleep alone in their crib. While co-sleeping may be enticing, especially after a late-night feed, it increases the risks of possible suffocation. However, “having your child in your room, in their own crib or bassinet, is protective for SIDS,” Karen said. “In fact, we think co-rooming reduces SIDS risk by almost 50 percent.” Co-rooming allows parents to keep new babies in close reach and helps parents oversee their baby’s sleep, just in case something happens.
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
Getting to Know Renown's Canine Companions
A slobbery kiss, a wagging tail, a judgement-free smile. There are few things better than the love and attention of a canine companion. At Renown Health, we have a loyal and playful group of pet therapy teams. This volunteer program uses animal-assisted interactions (AAI) and animal-assisted therapy (AAT) to provide comfort, reduce boredom, increase social interactions, improve mood, boost general well-being and – perhaps most importantly – bring smiles to our patients’ faces. Benefits of AAT & AAI: Lowers blood pressure and heart rate by relieving anxiety Helps in pain management Eases feelings of depression, loneliness, boredom and isolation Stimulates communication Encourages physical activity For more information about the program, a complete list of our teams or to get involved, click here. Meet Keno and Linda Linda, Keno’s human, has volunteered as one-half of a therapy dog team for more than 14 years. Keno is her third Newfoundland, and he is a sweet and cuddly 2-year-old pup, who, according to Linds, thinks is a lap dog. “My mother was in assisted living for almost 10 years, and I saw what an impact a therapy dog can have,” Linda said. When she moved to Reno from Portland six years ago, she immediately contacted Renown. A Memory the Stands Out: A patient in the ICU was not responsive because of oxygen deprivation due to almost drowning. Linda and Keno went into the patient’s room at his physical therapist’s request, and the therapist asked the patient to reach out and pet the dog. After the third request, he moved his hand toward the dog, and his mother burst into tears. It was the first time the patient had moved since his accident. Linda and Keno went back several days in a row, and soon the patient was talking, sitting up and eating on his own. Meet Madi and Clark Madi, Clark’s human, is an employee at Renown, and Clark made it a family affair by joining the team in Sept. 2021. Clark is a unique pup with an amazing demeanor who adores everyone as much as they adore him. He is a hardworking Goldendoodle who loves to be a goofball at home when he’s off the clock. Why They Became a Therapy Dog Team: Madi was inspired to get Clark trained as a therapy dog because, as an employee at Renown, she was always so happy to see dogs walking around, and she knew that I wanted to provide that same relief to others. Her favorite thing about being a Renown volunteer is the joy it spreads to those working and the patients they are caring for. Meet Richard and Raven Raven is a four old Belgian Malinois who has been working as a therapy dog for two and a half years. She is calm, friendly and loves having her tummy rubbed. “The therapy dog teams are just one little part of Fighting the Good Fight,” Raven’s human Richard said. A Memory that Stands Out: Raven and Richard were assigned to the Sierra oncology ward one shift and visited a woman who had a picture of her dog displayed next to her bed. Raven immediately went to the bedside and the patient started petting her. As she spent more time petting Raven, Richard could see the stress disappearing from her face. He later learned that it was the patient’s first chemotherapy infusion, and Raven gave her the peace and the strength she needed to face the chemotherapy head-on. Meet Savannah and Hallie Hallie and Savannah’s journey as a therapy dog team began in 2017 at the Morgan Stanley Children’s Hospital in New York and has also taken them to San Francisco General Hospital and Stanford Hospital. The duo moved to Reno in 2020 and immediately joined the Renown Pet Therapy Program. A friend, energetic and cuddly American Cocker Spaniel, Hallie especially loves spending time with the young children at the hospital. A Memory That Stands Out: Savannah remembers one visit to a patient in the Children’s Emergency Room who was struggling with suicidal thoughts. Having struggled with mental health herself, Savannah felt a deep connection to the patient and a need to help. She recalls placing Hallie on the patient’s bed a seeing a “very small hint of a smile.” Savannah later learned that the Renown nurses hadn’t seen the patient smile in days. It was that moment that made Savannah realize what a profound impact Hallie can have on patients. Meet Chivas and Donna Chivas was a McNab/Border Collie mix who volunteered at Renown with her human Donna for two years. With help from Donna, Chivas was a master at reading situations in the hospital and reacting accordingly. For example, if a patient was afraid of dogs, she would sit with her back to the person so she didn’t come off as threatening. Contrarily, she would lie down on the floor when playing with young children to let them pet her on their level. Why They Became a Pet Therapy Team: This dynamic duo started out as a member of a local pet therapy group. During the height of the COVID-19 shutdown, they participated in outdoor pet therapy parades for various hospitals in the area. Donna and Chivas met Renown Volunteer Coordinator Wendy Peuket at one of the parades and she inspired Donna to pursue becoming a registered therapy dog team for Renown's Therapy Dog Program. Chivas sadly passed away unexpectedly in early December 2021, and the world is a whole lot dimmer place without Chivas’ light shining brightly.
-
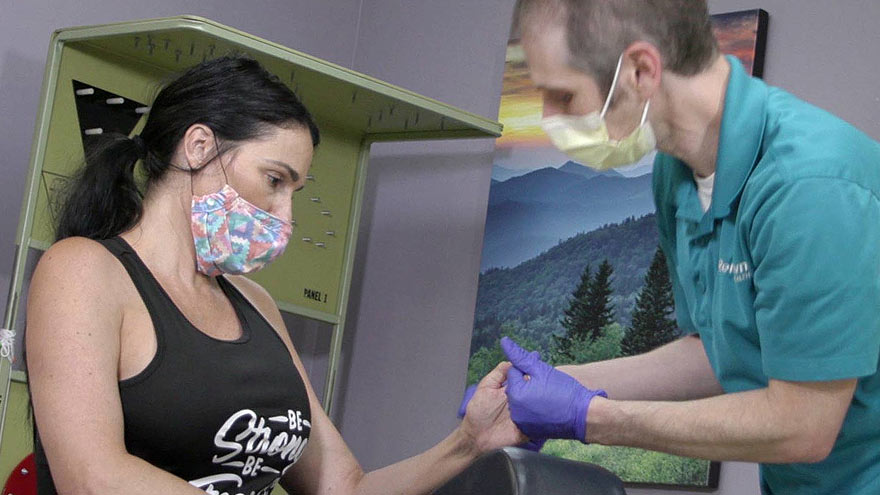
Cuidado confiable desde el hogar
Renown Health has always been on the frontlines of technological advancement, and that innovation remained unwavering during the COVID-19 pandemic. Our telehealth teams heeded the call to provide home monitoring for our patients, transforming how we provide care. The care providers at Renown successfully monitored lower acuity COVID-19 patients from the comfort of their own homes. Bernard Lee was diagnosed with COVID-19 and pneumonia, and was able to return home to continue his recovery with a home monitoring system. While at home, Bernard’s health took a turn for the worse while he was sleeping, but thanks to the continuous monitoring of Health at Home, his worsening vitals did not go unnoticed. “This monitoring system really saved my life,” Bernard said. “It was telling me that my sats were low, but I didn’t even feel the common COVID symptoms; I just felt tired.” Because of his low oxygen saturation (sats) and the continuous monitoring, he woke up to providers calling to check on him in the early morning. He was immediately transferred to the Renown Intensive Care Unit to be cared for and monitored by our expert care teams. Today Bernard is recovering, feeling great and continuously refers to the team and the home monitoring system as his guardian angels.
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
A Family's Legacy
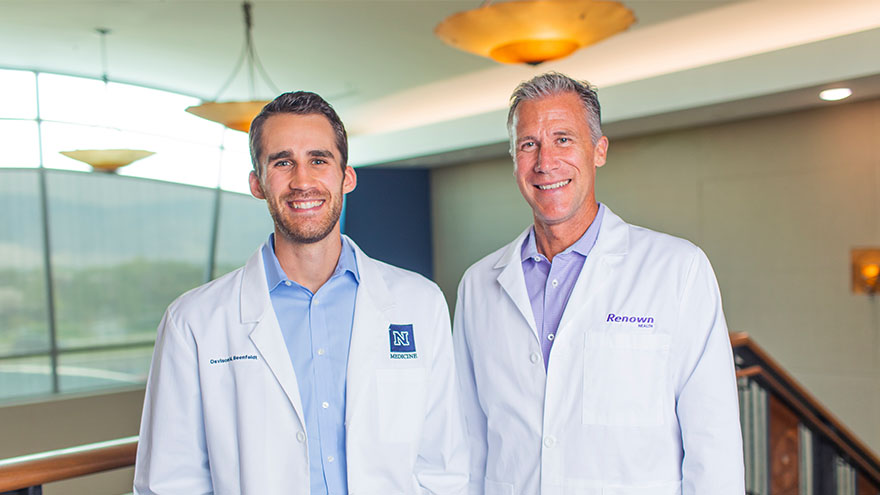
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school
-
Una guerrera que sobrevivió a un ataque cerebrovascular: la historia de Kimi
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Baby's Ears and Altitude Changes
One of the best things about living in the Reno area is the beautiful mountain range that surrounds our city. Many families take advantage of the activities the mountains have to offer or travel over them to visit friends and family in neighboring areas. However, for parents of infants there is often angst over your baby’s ears and altitude changes and the associated potential for ear pain and/or “popping.” Fortunately, there are things you can do to protect your infant’s ears the next time you drive over the mountain or hop on a plane with your little one. Baby’s Ears and Altitude Changes: What Causes Them to “Pop” The simple answer is pressure. The problem originates in the middle ear where there is an air pocket that is vulnerable to changes in pressure. The Eustachian tube, which runs behind the nose to the middle ear, is constantly absorbing and resupplying air to this pocket to keep it balanced. When the pressure is not balanced, your ears feel “clogged” or like they need to “pop.” In some cases this sensation can cause significant ear pain and even temporary hearing loss. Rapid changes in elevation or altitude, like driving over a mountain, or ascending or descending on an airplane, can cause rapid changes in pressure. In order to avoid problems, the Eustachian tube needs to open widely and frequently to equalize those pressure changes. The problem often intensifies during descents as you go from an area of lower atmospheric pressure to an area of higher atmospheric pressure. This is why you hear babies screaming on planes during descent or why your infant is wailing in the car seat as you head down the mountain. What can you do to make it a more comfortable trip for your child? First, be prepared. Babies cannot intentionally “pop” their ears like adults can, but we can help them by encouraging them to swallow. Offer your baby a pacifier or bottle while making ascents and descents. If possible, it may be helpful to have an adult ride in the back seat with baby if you’re in the car to ensure this can happen. Don’t let your baby sleep during descent on a plane. Help your little traveler out by offering him or her a pacifier during this process, as descent is the most likely time for pain associated with altitude changes. If your baby is congested prior to travel involving altitude changes, seek the advice of your pediatrician since they may have other solutions, including medications such as decongestants. If you return from a trip and notice your infant is still fussy and uncomfortable, contact your child’s doctor for a thorough ear evaluation. Safe travels!