Buscar
-
Nourishing Your Loved One Through Cancer Treatment
Eating healthy is a daily challenge for many, but for those with cancer, it is an even harder struggle. A cancer diagnosis affects not only those diagnosed but family members and friends, too. One key area of concern is making sure your loved one stays well by eating healthy food every day. Here are some vital cancer nutrition tips from Jessica Blauenstein, a Board Certified Specialist in Oncology Nutrition and Registered Dietitian at Renown Health. Help to Prepare Meals and Snacks for Daily Cancer Nutrition Make it grab and go. Easy-to-make meals help reduce the burden of having to cook and prepare food. Having easy to grab snacks on the counter or in the fridge can help ensure your loved one has access to those nutrients when needed. Sit outside of the kitchen. This allows your loved one to avoid cooking smells which can make them feel sick as a side effect of cancer treatments. Also try serving them cold foods such as sandwiches, cheese and crackers, or shakes which have a mild scent. Try drinkable meals. Some people with cancer find it easier to sip their calories over the course of 30 minutes to an hour. Consider smoothies or supplemental shakes such as Ensure Complete, Fairlife shakes, Orgain shakes, or Boost Plus to name a few. A great foundation for a smoothie is a protein source (Greek yogurt, protein powder, nut butters or milk) with a carbohydrate (fruits, juice or berries). Add other ingredients as desired, such as spinach, kale, and ground flaxseed or chia seeds to give it more vitamins, minerals, and fiber. Snack Ideas for Those Undergoing Cancer Treatment The following ideas are both quick and easy to make for your loved one. Chicken or tuna salad with whole grain crackers or as a sandwich on whole grain bread Greek yogurt mixed with cereal, fruit and/or nuts Cottage cheese with banana, cinnamon and/or peanut butter Favorite fruit with 100% natural peanut or almond butter spread - Try peanut butter with bananas, apples, or even celery Their favorite veggies dipped in a salad dressing of your choice - For example, carrots with hummus, tahini, or ranch dressing Cheese and whole grain crackers - Add tomato slices with a small amount of avocado, and a dash of oregano on top for more flavor Eggs scrambled with cheese, vegetables and/or salsa Peanut butter and jelly sandwich on whole grain bread A baked sweet potato with some favorite toppings Hard boiled eggs and/or egg salad with whole grain crackers, or as a sandwich on whole grain bread Oatmeal or cream of wheat prepared with milk, fruit and/or nuts Sometimes your loved one may not feel like eating or refuse to eat. If treatment side effects are impacting your loved one’s ability to eat, please visit the websites below containing recipes tailored to treat side effects. Cook for Your Life ELLICSR Of course, you may also consult a registered dietitian and/or the patients care team, if you have more cancer nutrition concerns.
Read More About Nourishing Your Loved One Through Cancer Treatment
-
The Impactful Role of Renown Health Foundation's Board of Directors
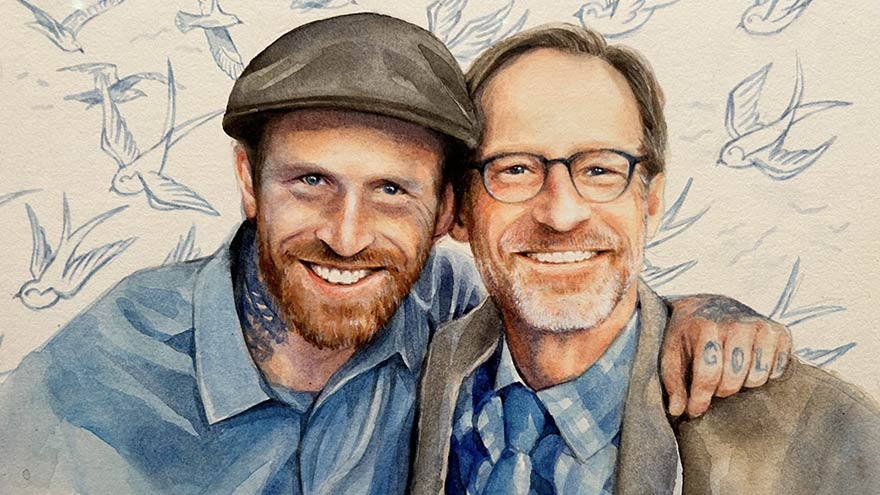
Above: Brian Cushard (left), Renown Health Foundation Board Chair, with his family At Renown Health Foundation, our mission is simple yet powerful – to raise funds that support Renown Health, the largest not-for-profit health system in northern Nevada. We are the driving force behind initiatives that bring state-of-the-art equipment, conduct groundbreaking research, enhance healthcare services, improve patient outcomes and contribute to the overall well-being of our community. Our Dedicated Board of Directors Our impactful work would not be possible without our Board of Directors – a fantastic team of 27 local volunteers. They bring diverse skills to the table, working together to create positive changes in healthcare for northern Nevada. Our board is at the core of our Foundation's success by guiding important decisions, sharing valuable insights and actively engaging in community relationships. Meet Brian Cushard – Renown Health Foundation’s Chair Brian Cushard took on the role of Foundation Board Chair at the beginning of 2024. Brian, who is the President of LP Insurance Services in Reno, will lead us for the next two years, bringing a wealth of experience and a deep commitment to community well-being. Since joining Renown Health Foundation’s Board in 2018, Brian has been instrumental in shaping our strategic direction. Brian’s Vision: Advocating for Renown Health’s Mission and Making a Difference We had the opportunity to sit down with Brian and explore his passion for healthcare philanthropy and the positive changes he envisions. Brian's 'why' is firmly rooted in the belief that a robust health system serves as the backbone of the community. His vision extends beyond fundraising; it's about inspiring the community by sharing remarkable stories of care and championing Renown's impactful contributions. Q: Why does Renown's mission matter to you, and how do you see your role making a difference? A: Renown's mission matters deeply to me because, without a highly functioning healthcare system, the economic structure of the community can be impacted. At LP Insurance, where I work, we see ourselves as guardians of our clients' hopes and dreams. This translates to my role on the Board as stewards for the health of others. Advocating for a highly functioning health system is crucial in supporting community members and clients alike. Surrounding ourselves with a solid network is essential. As advocates, our voices are integral in ensuring that everyone's voices are heard. Q: Can you share a moment that made you want to support healthcare causes? A: There are those stop-in-your-tracks healthcare moments that make you reassess life's priorities. I've had moments where life comes to a standstill, and what you once thought was important takes a backseat to the basics of life—getting better, one step at a time. In those vulnerable moments, you realize the importance of every person at the hospital. In desperate need, we rely on them. It's eye-opening and gives perspective on what's truly valuable in life. Q: Tell us about a time when you saw the positive impact of healthcare or philanthropy. How did that influence your decision to get involved? A: One impactful moment in philanthropy stands out — the Music and Miracles concert featuring the Beach Boys. LP Insurance was a major donor, contributing $100,000 to benefit Sophie’s Place, a music therapy room coming to Renown Children's Hospital. On the day of the event, my wife and I volunteered and saw the remarkable community support for Renown Children’s Hospital. The collective efforts that day raised over $1 million, specifically designated to establish Sophie’s Place. This experience inspired me to want to do more, as I recognized the profound positive impact that philanthropy can have on healthcare and the community. Note: Sophie’s Place, opening later this year, will offer vital care and healing experiences for young patients at Renown Children’s Hospital.
Read More About The Impactful Role of Renown Health Foundation's Board of Directors
-
Departamento destacado: Fundación de Renown Health
Kick off 2024 with us as we celebrate the team behind our very own Renown Health Foundation! When you visit Renown Health, you take a look around and can’t help but notice the robust programs in place. You look left and see our thriving Children’s Miracle Network Hospital at Renown, making a lasting impact on pediatric healthcare in our region. You look right and see the advanced William N. Pennington Cancer Institute, providing leading-edge treatments right here in our community. You look around you and notice an influx of smiling nurses from the Orvis School of Nursing at the University of Nevada, Reno (UNR) who receive tuition assistance, thanks to generous donations to the Gerald “Jerry” Smith Academic Practice Partnership. Then, you think to yourself: “These programs must need a lot of money and support. So, how on earth is this all possible?” What you may not know is that these programs are funded by the generosity of our community, all made possible by the work of Renown Health Foundation. As the largest not-for-profit health system in northern Nevada, our mission to make a genuine difference in the health and well-being of everyone we serve flourishes because of the donations, sponsorships, endowments and more that our Foundation brings in from philanthropists all over the region. Making It Happen The reach of Renown Health Foundation has proven to be virtually limitless, with a clear focus on supporting and raising funds for programs and initiatives that enhance the lives of our patients and their families, all for the betterment of our community for years to come. Under their growing umbrella, the dedicated team at the Foundation makes miracles happen through administering a wide range of philanthropic programs, including: Children’s Miracle Network Hospitals (CMNH), a nonprofit organization that supports the health of 10 million children in the U.S. and Canada every year. Renown Children’s Hospital is proudly recognized as a member of CMNH. Gerald "Jerry" Smith Academic Practice Partnership, a partnership between Renown Health and the UNR Orvis School of Nursing to provide 24 nursing students a year with full-ride tuition assistance and a guaranteed career in nursing at Renown. Fianna’s Healing Garden, a healing garden bringing serenity to all at Renown Regional Medical Center, built from the vision of Fianna Dickson Combs. Miracles at Montreux Golf Tournament, an annual golf tournament that takes place at Montreux Golf & Country Club and consistently raises hundreds of thousands of dollars for Renown Children’s Hospital. A full slate of individual giving programs, including Legacy Giving, Employee Giving and Leadership Giving. But it doesn’t stop there – the Foundation is helping our health system build more ways to care for our community by securing major gifts to fund advanced healthcare facilities and innovative healthcare solutions: William N. Pennington Cancer Institute, the premier oncology institute in the region providing a large array of personalized cancer care services, including Medical Oncology, Infusion Services, Clinical Research and more. Renown Institute for Robotic Surgery, offering the latest advancements in surgical technology with robotic-assisted surgeries, which ensure precision, faster recovery and improved outcomes. Sophie’s Place, a state-of-the-art music therapy room currently in construction at Renown Children’s Hospital. This new space will be specially designed for children and their loved ones to enjoy the healing power of music and engage in the arts. Conrad Breast Center, the latest addition to the planned Specialty Care Center at Renown South Meadows Medical Center which will include breast imaging, infusion and surgery services along with a wellness center. Jeanne and Raymond Conrad donated a $5 million lead gift to support this important project and the Foundation team is currently working to raise an additional $6 million in 2024. It may go without saying that a day-in-the-life of these spirited team members is never a dull one. Every day brings on a new challenge to face and a goal to meet. “A day at the Foundation is a day full of emails, calls and visits with friends of Renown,” said Abbey Stephenson, Planned Giving Officer. “Our main goal is to raise funds to support the mission of Renown, and most of our outreach efforts are to encourage philanthropy and donations. We have a very collaborative team, so we can often be found in each other’s offices strategizing about fundraising initiatives, communications and next steps with specific supporters.” “For me, a typical day involves making sure I have a donor scheduled for coffee or lunch, working on proposals that may need research and preparing presentations,” added Jerry Cail, Major Gifts Officer. “Staying connected, I send thank you notes for any donations-usually once a week and make at least three ‘Grateful Patient’ calls to set appointments. I always make sure I am ready to contribute to any meetings I have for the Foundation." While the scope of the Foundation’s charitable efforts goes beyond hospital walls, they also thrive right here in our own health system. Through our Grants Program, Renown’s departments and programs can leverage the connections and skills Renown Health Foundation has in order to secure funding from a multitude of grant sources. "Grant funds from foundations, and local, state and federal governments benefit the patients and communities we serve to further our mission, vision and values,” said Pam Citrynell, Development Officer. “Past grants have supported the purchase of state-of-the-art equipment, facility development, pandemic recovery, research and clinical trials, physician and researcher recruitment, community health programs and educational training for our healthcare professionals.” Every Foundation team member lives their passion every day while at work, frequently expressing gratitude for the immense impact they have the opportunity to make. “I love coming to work because I get a very real opportunity to make a genuine difference and meet some fantastic people who believe in and support our mission,” said Leah Nelson, Director of Community Giving. “I have had the honor of meeting donors and the families they support. I couldn't be prouder of what our team has accomplished over the years and am excited for what is to come.” The impact of the Foundation team’s tireless efforts extends far into the future, securing Renown’s lasting legacy in contributing to the continued health and well-being of our community. “Philanthropy is not only a financial science but a very specific methodology where connecting resources are paramount; it requires careful intelligent management coupled with lots of hard work, patience, and vision,” said Yvonne Murphy, Development Officer. “The work that the foundation does every day makes resources available to enhance the healthcare experience for all those who seek care at Renown. Our work impacts not only this present moment but in fact is a legacy that will bless this community beyond our lifetime.”
Read More About Department Spotlight: Renown Health Foundation
-
Departamento destacado: Float Pool
Ring in the New Year and the rest of the holiday season by celebrating Renown’s Float Pool team! After coming out of the COVID-19 pandemic, it's no mystery that healthcare across the country has shifted and adapted to the growing needs and new demands of our patient populations. Renown Health is no different. As the largest not-for-profit health system in the region, we are no stranger to change, even when change presents challenges. Who do we call on when a unit needs more team members in the eleventh hour? Who can help when our patient volume spikes up with seconds to spare? This is where the Float Pool at Renown comes to the rescue. Skilled in a wide variety of healthcare specialties, from acute care nursing and critical care to care aiding and patient safety, this is the team that can seamlessly step in to provide crucial patient care to the units that need it most, whether a team is understaffed for the day or needs extra all-hands-on-deck for a specific patient or procedure. Float Pool team members are equipped to work in virtually any clinical area at Renown, making a genuine difference with every patient they encounter. A Pool of Relief Teams across Renown can breathe a sigh of relief knowing that Float Pool has their back in times of need. As the backbone of our health system, these dedicated team members possess a wealth of clinical knowledge and the ability to navigate diverse medical environments. Their flexibility allows them to fill staffing gaps and provide essential support to many different units. “We fill in the gaps of staffing to make everyone's day better,” said Patti Crepps, Critical Care Float Pool RN. “A float nurse has to be flexible and able to adapt to different situations and places – basically, ‘go with the flow.’ Patient care is basically the same all over; we make patient care possible by being familiar with all the various specialties and providing the specific care needed depending on the population we are taking care of on that shift.” “Float Pool staff members are like healthcare chameleons, transitioning between different departments,” added Shelby Riach, Acute Float Pool RN. “We incorporate flexibility, teamwork and a commitment to ensuring patients receive the best care, regardless of the setting or circumstances.” This team thrives in uncertainty; in fact, no workday is the same in Float Pool – and that’s exactly the way they like it. Working with many different teams across a multitude of specialties, these Care Aides, RNs, Critical Care Techs, Patient Safety Assistants (PSAs), Certified Nurses Assistants (CNAs) and more enjoy facing change, while they all share a goal of providing the best patient care possible. “No day looks the same; since we are the Float Pool, we are assigned a different assignment on Smart Square every day, whether it be as a care aide, a patient safety assistant, a unit clerk or patient transport,” said Melina Castenada, Care Aide. “If we are assigned as a care aide on the floor, we help assist with call lights and help with whatever nurses and CNAs may need, including feeding, transporting, walking, helping patients use the restroom, etc. When we are assigned as a PSA ‘sitter,’ we sit for the patient to help keep them safe. If we are assigned as unit clerk, we help answer phones and direct patients appropriately, file paperwork, answer call lights if needed and assist with office work.” “I love that every day is a different floor with different tasks and a different atmosphere,” added Julia Chappell, Critical Care Technician. “I find out which floor that I will be on right before my shift starts and head to the floor to find out my assignment for the day. Depending on the specialty, such as the medical-surgical floor versus an intensive care unit (ICU), my daily job tasks can vary.” When it comes to high-risk patients, who require special attention, PSAs within Float Pool step in to help. “The PSA role within Float Pool largely consists of adverse event prevention for our high-risk patients, and being a Float Pool employee allows us to work wherever we are needed,” said Dimitri Macouin, Patient Safety Assistant. “Whether it be in the emergency department, neurology or pediatrics, the PSA will be the eyes and ears for the nurses working with this patient population.” “Great strides have been made to ensure that PSAs remain vigilant and are recognized as an integral part of the patients' care team rather than 'just a sitter,’” added Karla Phillips, Patient Safety Assistant. Float Pool also oversees our Discharge Lounge, which offers patients and their families a dedicated space to reconnect and prepare for their discharge from the hospital. “The increase in utilization of the Discharge Lounge is something we are very proud of,” said Kara Abshier, Care Aide. “We assist in discharging patients from all over the hospital to help the floor and get new patients into rooms.” Every day brings a new challenge for Float Pool. As these team members wake up with uncertainty, they are ready to embrace the diverse demands of caring for patients of all ages. “The fact that Float Pool exists is amazing,” said Hannah Luccshesi, Acute Float Pool RN. “We wake up with no clue as to whether we will be working with babies, children or adults and then fill in the needs of the hospital.”
-
A Token of Appreciation: Renown’s Employee Giving Program
Pictured above from left to right: Jessica Bajwa, Nancy Bell, Laurie Goodman and Troy Fernandez As we approach the holidays and the season of giving, we reflect on the generosity and kindness that our employees here at Renown embody. Since 2007, Renown employees have donated $2,931,018 through Renown’s Employee Giving Program. This program provides our staff with the opportunity to make a difference by funding advanced equipment, research, community health initiatives, professional training and more. Regardless of the dollar amount, every contribution has a meaningful impact and remains entirely within Renown to support our mission. Employees can participate in the program at any time of the year by signing up for recurring payroll deductions or by making a one-time donation of any dollar amount. They can donate to one of Renown’s top priority areas of support or a different fund of their choice. Meet Jessica, Nancy, Laurie and Troy Renown employees Jessica Bajwa, Nancy Bell, Laurie Goodman and Troy Fernandez all have their own reasons for participating in the Employee Giving Program, but they all share the same goal: To give back to their community. Jessica Bajwa has been working at Renown for about seven years. She was at an employee event five years ago and found out about the Employee Giving Program through Renown Health Foundation. They explained the different areas she could donate to and how to get signed up. When Jessica looked back on the comforting care and healing her daughter had received at Renown Children’s Hospital, she felt empowered to give back to other children and families staying at Renown, so she enrolled in recurring payroll deductions to donate to Healing Arts. “It’s so easy and convenient to sign up,” said Jessica. “It means a lot to me to give to this area where they provide a healing environment, especially for patients and families at Renown Children’s Hospital – My daughter still has a blanket they gave her when she was there,” Jessica said she likes that the Employee Giving Program allows employees to choose their area of support to donate to and donation amount. Nancy Bell said she’s proud to give back to Renown after having received a great amount of support from her coworkers during an incredibly difficult time when a family member of hers was being cared for in Renown’s ICU, just three weeks into her employment at Renown. “I had employees from not just my team but also across the organization reaching out to me and checking in to see how I was doing,” said Nancy. Nancy said she was positively impacted by that kind of support through her work family at Renown and decided to start giving back in 2011 by signing up for recurring payroll deductions to donate to the William N. Pennington Cancer Institute – to this day, she is still making donations to this area of support. When Laurie Goodman began working at Renown in 2013, Renown’s Human Resources team offered her different ways to give back as an employee. “At the time, I was often caring for foster children and seniors,” said Laurie. “My family and I have always wanted to help others in need.” Laurie had been taking care of an elderly woman who was a patient at the old Renown Skilled Nursing Facility and decided to enroll in payroll deductions to donate to this facility. When that facility closed, she received a letter asking which area she wanted to transfer her donations to, and she decided to begin donating to Renown Children’s Hospital to give back to kids in the community. “I’m fortunate for not only my employment at Renown, but my husband’s and daughter’s employment as well. As employees of Renown, we have such great jobs, benefits and opportunities, and I think we should all strive to give back to express our gratitude and appreciation.” At his employee orientation in 2012, Troy Fernandez heard about Renown’s Employee Giving Program and learned that funds were needed for individuals who needed financial support to pay for healthcare services at Renown. He knew his donations would go to a good cause and signed up for recurring payroll deductions to donate to the Greatest Need Fund. “It feels good to be able to give back to those who are less fortunate than us,” said Troy. “It was very easy to enroll in this program, and I’ve been donating to the same support area ever since.”
Read More About A Token of Appreciation: Renown’s Employee Giving Program
-
Why I Give: Dan’s Story
In the fall of 2020, Dan's world was suddenly shaken when he received a distressing call: his son, Jeremy, was admitted to Renown with complications from spinal meningitis. Without a second thought, Dan rushed from Southern California to be by Jeremy's side. For an agonizing 10 days, Dan remained in the ICU. He was overwhelmed with worry and helplessness as Jeremy fought for his life on a ventilator. During this time, Dan, an esteemed artist and professor, found comfort in the collection of artworks adorning the walls at Renown. With more than 2,000 pieces of original art, Renown has meticulously curated hospital rooms, hallways and various spaces to support those in need. Dan, who talks about art's magic every day as a professor, experienced its power in a new light.
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
Departamento destacado: Security
“Safety is Number One,” isn’t just a saying – it's a fact of life, especially at Renown Health. The safety of all patients, visitors, staff and volunteers is always the top priority, and our Security Department takes that commitment seriously. This team is devoted in their efforts to provide a safe environment for all, building cooperative and proactive security processes leveraging crime prevention techniques and state-of-the-art technology. Renown Security sets the safety and well-being bar high, and they continually exceed that standard day in, day out at all of our hospitals and urgent care, primary care and lab locations. Specially Trained, Continually Present Our Security Department isn’t staffed with your run-of-the-mill Security Officers; these team members surpass security and safety expectations. Think city and state police-level standards. You read that right – many of Renown’s Security Officers come from Nevada Highway Patrol, the Washoe County and Carson City Sheriff’s Offices, the state probation and parole board and more. This team fosters specialized training in a collaborative environment. Every member of the security team has extensive training in compassion, empathy and de-escalation techniques to provide the highest levels of safety and security. They implement this training in all their daily duties, whether they are saying a simple ‘hello’ to a patient passing by or preventing harm to a staff member. Before their shift begins, the team meets to debrief meeting to discuss major incidents that occurred on the previous shift. These meetings ensure the next shift is aware of situations to be on special alert for and individuals to look out for. After, the team members head off to their assignments. “The day could be as mellow as greeting someone at the welcome table, or it could be as chaotic as de-escalating someone in distress,” said Emmanuel Fernandez-Orozco, Supervisor of Security at Renown Regional. “Regardless of the day, every experience is rewarding in its own way. The only thing that is promised is that every day will be different.” While every Security Officer has varying experiences, one aspect of their job always stays the same: they are always on alert for any potential safety issue. Even on the “slowest” days, it is important for this team to stay vigilant in order to mitigate any potential risks. There are several security programs that the team uses to keep everyone at Renown safe and secure: Renown's security operations center team (also known as dispatch) monitors all cameras in real time, with security officers patrolling parking areas 24/7. Security escorts are always available for any employee, patient or guest at every Renown location. Security Officers can escort anyone to their designated site, check surroundings for danger and monitor the person until they safely leave for their next destination. Rescue officers are available for any Renown location where an employee feels unsafe. Security maintains a strong relationship with the Reno Police Department (RPD) and assists with reporting and providing information that aids RPD in pursuing and deterring criminal activity. “In security, we are a counselor, teacher and rule enforcement officer, all rolled into one,” said Bob Stone, Supervisor of Security for Renown Health. Talk about master multitaskers! Protection is only one part of the job. Through positive and meaningful interactions with guests, patients, community and staff, regardless of where they are posted, the Security Department continually helps Renown achieve its mission of making a difference for the people they serve. Devoted Dispatch Speaking of multitasking, no one does this better than the Security Dispatch Center. Security Dispatchers are the “eagle eyes in the sky” at Renown, keeping a close watch on everything that happens within every Renown location, as well as REMSA (including Care Flight). From overlooking the many cameras around campus and administering codes over the PA system to manning the radio and phones to ensure Security Officers are dispatched quickly, our dispatch team helps ensure every safety or security issue at Renown is immediately addressed. When a call comes in, dispatchers like Jessica Fernandez, Security Dispatcher for Renown Health, go through a quick discovery process (sometimes in seconds) to figure out the details of the situation or code and what level of security is needed to assess and de-escalate. According to Jessica, the ability to prioritize is something she values in her work. “80 percent of our duties are on the phone and the radios, and we are skilled in prioritizing concerns based on the sheer volume of calls we get,” she said. Jessica and her teammates are proud of the outcomes from their calls. Their attentiveness to every nook and cranny at Renown and their quick response times to make them not only a valued partner to the Security Department but also a necessity to our health system. Your In-House De-Escalation Experts Being in a hospital environment is undoubtedly stressful for any patient, and many factors can increase these emotions. The Security Department takes these feelings seriously and never hesitates to take appropriate action to ensure the safety of everyone at Renown. With the unfortunate rise of violence against healthcare workers, especially amid the pandemic, our first-rate security team has been crucial in countering violence with specialized de-escalation techniques. The key to de-escalating, according to the Security Department, is to put yourself in the shoes of whoever you are working with. As stated by Bob Stone, the team approaches each situation by asking themselves: How would I want to be treated if I was in the same circumstance? “Being empathetic to their situation and listening to what is going on in their lives is key to re-directing them accordingly,” said Bob. “Applying real-life experience to similar circumstances can make them feel like they are not alone. Educating people on hospital policies can also help them reduce their anxieties and solve the problems.” Jhorddy Lopez, Security Officer at Renown Regional, approaches each situation with the mindset of knowing that each person’s reactions are different. “Different techniques need to be implemented every time,” said Jhorddy. “You have to use your best judgment call.” Quick and effective judgment calls are a task that the Security Department has conquered. Rosie Garcia, Security Officer at Renown Regional, knows that using your best judgment means getting both sides of the story. “Whenever I need to step in and de-escalate a situation, I first speak with whoever is attending to the patient and gather information,” said Rosie. “Then, I always get the patient’s side as well. I want to understand how they’re feeling, so both the staff member and the patient can meet in the middle and come up with a collaborative solution.” An example of the heroism and advanced de-escalation displayed by our Security Officers takes us back to last spring. In the middle of the night, a Care Flight helicopter transporting a patient and their family was about to touch down on the landing pad outside of Renown Regional. Right as the helicopter was about to land, an individual jumped over the safety barricade and onto the landing pad. Alexander Pico, a former Security Officer Lead at Renown Regional (who recently joined the Carson City Sheriff’s Department) immediately communicated with the individual to leave the area. The individual then went under the rear blade, which is the most dangerous part of the helicopter. Knowing that he had to risk his own life at this point to save another, Alexander ran around the back of the helicopter and tackled the individual, preventing catastrophic injury or even death. Steve Perkins now uses this example of a swift judgment call, which was captured on dispatch cameras, as training material for new staff. Exceptional character, compassion and emotional intelligence are the attributes that every member of the Security Department holds. As noted by Steve Perkins, these attributes “allow for a quick assessment of each situation in order to de-escalate and move towards the best possible solution." Securing the Job The Security Department at Renown is actively hiring caring, dedicated team members who are ready to jump in and perform exceptional high-risk healthcare security services for our health system. “We seek people with the right combination of ability and demeanor,” said Steve Perkins. "The training and skills development we provide result in a high caliber of success.” Every team member in the Security Department is passionate about the same thing: helping others. And in a healthcare environment, this is important. “Working a healthcare security job is far different than working any other security job,” said Jhorddy Lopez. “At a hospital, you get the chance to interact with people one-on-one. I get to experience the feeling of, ‘I can make a difference in this person’s life.’” Any interaction can change the course of a person’s day, and the Security Department embraces this fact. “I really do love helping people so much, whether it be an elderly patient who needs help with their wheelchair or a situation where I need to step in and de-escalate,” said Rosie Garcia. In order to succeed in this fast-paced department, being a collaborative team member is crucial. “A good coworker is a team player – someone that loves to work in a team atmosphere,” said Emmanuel Fernandez-Orozco. Jhorddy Lopez reiterates this, adding that “communication and trust are also extremely important. Everyone has to have great communication skills and have each other’s backs.” For people like Bob Stone, having a special connection to Renown inspires him to serve. As someone who experienced two life-saving hospital stays here, he is proud to give back to the organization that gave so much to him. “It was only natural to return to a facility I was familiar with my entire life,” said Bob. “After serving as a paramedic and transporting patients into Renown from Plumas County, I knew I was not done giving back to the community. Renown was the place to do exactly that.” All Genders Welcome A common misconception about the security field is that it is strictly a “man’s job.” In Renown’s Security Department, that couldn’t be further from the truth. As a female Security Officer, Rosie Garcia is a prime example of proving that idea wrong. As a master patroller and de-escalation expert, she ensures everything is running smoothly and that everyone feels safe at all times. “When I first started here, I knew right away that nobody that works here is biased,” said Rosie. “Everyone is equal, and I am treated as an equal in this department. I know I can do the job as well as any man." Both Rosie and her counterparts in the Security Department firmly believe that this line of work is for everyone, and they continually lift each other up and support one another. “No matter your gender, as long as you have confidence and integrity, you will do well,” adds Rosie. The Bottom Line If you are passionate about creating a secure environment to ensure patients get the care they deserve and employees receive the safety they merit, the Security Department is your team to join. “I come into work with pride,” said Jhorddy Lopez. “Knowing that I can change someone’s life – that makes me proud to work here.” “You’re in good hands with us,” closes Steve Perkins.
-
What is Dry Drowning?
Whether you're a parent, grandparent, caregiver or sibling, you should know drowning is the second leading cause of death among children. Yet, while we are vigilant about protecting children from water accidents and drowning, a condition known as dry drowning or delayed drowning can go unnoticed. In fact, most people aren't even aware it exists. Dry drowning defined Dry drowning is a side-effect of a near-drowning experience and includes spasms of the vocal cords and larynx — known as a laryngospasm. This occurs when the body attempts to shut down the passage of any liquid into the lungs. Unfortunately, it can also shut down the passage of air into the lungs and force fluid into the stomach and lungs. Often the condition is not discovered until it's too late — severe cases can cause death within one to 24 hours after a water incident occurs. Who is susceptible? Novice or first-time swimmers are at increased risk, as are children with asthma and known breathing issues. In addition, children who have had pneumonia or experienced acute respiratory distress syndrome are also at greater risk. To reduce these factors, caregivers should be exceptionally watchful of inexperienced swimmers. According to Leland Sullivan, MD, of Northern Nevada Emergency Physicians, children under the age of 5 are most susceptible to drowning and often drown in residential swimming pools. Infants less than 1-year-old most often drown in bathtubs. What are the signs of a dry drowning episode? If your child has a near-drowning incident, a few moments of coughing until they calm down is normal. However, you should know the more severe signs and symptoms to watch for during the 24 hours following the incident, including: Persistent coughing Difficulty breathing and/or shortness of breath Chest pains Extreme fatigue and/or lethargy Change in typical behavior Face becomes pale What is the treatment and prognosis for dry drowning? Dr. Sullivan recommends that all victims of near-drowning incidents seek medical attention, even if they have no symptoms. If caught early, dry drowning can be treated. If you think your child is experiencing a dry drowning episode, go to the nearest emergency room as quickly as possible — do not attempt treatment at home. Healthcare professionals will work to supply oxygen to your child's lungs to restore and regulate breathing.
-
Enfrentar la amenaza de la violencia laboral en los hospitales
In recent years, workplace violence against healthcare workers has been on the rise. According to the Occupational Safety and Health Administration (OSHA), about 75 percent of nearly 25,000 reported annual workplace assaults occur in healthcare and social service settings. Those who don’t work in healthcare may be surprised to learn that violent altercations are so common in our field. Hospital settings can create fear and stress for patients and their families. Pain, mind-altering medications and drugs, and difficult prognoses can amplify these feelings. While inappropriate responses may be understandable, violence cannot be tolerated. As the leader of a health system, protecting our employees is an issue that I take seriously. Reporting Workplace Violence Unfortunately, sometimes employees don’t report dangerous incidents fearing they might be blamed, or not realizing it’s a reportable offense. At Renown Health, we take these events seriously. We have clear, mandatory policies and protocols for reporting and investigating violent incidents. Each incident is investigated to ensure follow through and accountability. We also teach de-escalation skills to our hospital security teams, clinicians, and other frontline employees. As an added layer of protection, Renown Health has a first-rate security team that closely monitors activity on our campuses, addressing potential issues before they escalate. Our organization values our partnerships with community organizations including local law enforcement agencies like the Washoe County Sheriff’s Office and the Reno Police Department. Renown Health maintains a close relationship with these partners, and we alert them when our care teams experience an increase in violent incidents. I also recognize that workplace violence is a national problem that demands collaborative solutions. That’s why I am also proud to serve as a member of the American Hospital Association’s Hospitals Against Violence Advisory Committee. Nurses, doctors, paramedics, and frontline health workers care for us every day. It’s our responsibility to support them by ensuring they feel safe at work.
Read More About Addressing the Threat of Workplace Violence in Hospitals
-
Cuidadores serviciales hacen realidad el sueño de una boda
A wedding is a big day for the wedding couple, but it’s also special for loved ones. A patient at Renown, Ken, got to take part in his daughter’s special day as her wedding plans changed to accommodate his medical condition. Grab some tissues and read how Renown’s team of compassionate caregivers and chaplains planned a wedding in Fianna’s Healing Garden. Ken was hospitalized at Renown Regional Medical Center where he was battling a lung problem – which was unrelated to COVID-19 – and his condition worsened rapidly on Wednesday, Aug. 12. His family made the decision to transition him to palliative care, which helps patients near the end of their lives remain comfortable, while supporting their dignity and quality of life. Ken’s medical condition altered wedding plans for his daughter, Chandra, and her fiancé, Tyler, who were planning to tie the knot later in 2020. Chandra wanted her father there, but knew he could not leave the hospital. That’s why Chandra’s sister, Heather, approached Ken’s care team with a request to have a small wedding ceremony at the hospital. Planning the Wedding A member of Ken’s care team, Amy Heston, registered nurse (RN), began planning how the wedding could be held outdoors in Fianna's Healing Garden in the E. L. Wiegand Pavilion, which was donated by the E. L. Wiegand Foundation. In 24 hours, Amy planned a wedding ceremony with the help of her colleague, Breyanna Aufiero, RN; the Renown Spiritual Care team; and nursing leaders on the coronary intensive care unit (ICU). Together, they decorated the aisle in the garden with flowers and battery-operated candles. They also made a sign for Ken’s hospital bed, which read, “Father of the Bride,” and crafted a bow tie for him to wear for the special occasion. With visitor restrictions in place at the hospital due to coronavirus (COVID-19), having the wedding outside in the Healing Garden allowed for more members of Ken’s family to attend including his wife, Charlotte, and his dog, Bella. Every step in planning the wedding required thoughtful and thorough care coordination so Ken could participate. His breathing was supported by oxygen and special arrangements were made to transport the oxygen tanks he needed to take part in his daughter’s wedding. Amy worked with respiratory technician, Kasey Benfield, and critical care technician, Ruben Duckworth, to ensure Ken’s oxygen needs were met using portable machines. Celebrating Love and Life Together Ken’s team of caregivers bathed him and shaved his face so he could look and feel his best for the ceremony. They put on his bow tie, covered his bed in decorations and his favorite blue, flannel blanket, and wheeled his bed outside for the ceremony. Renown associate chaplains Terri Domitrovich and Susan Palwick coordinated music and performed the ceremony for Chandra and Tyler on Thursday, Aug. 13, 2020. The bride and groom shared their first dance in the garden and Ken’s care team provided water and treats to give the family a full wedding experience. Shortly after the ceremony, Ken passed away. This wedding provided Ken and his family meaningful memories for their big life-changing moments as they celebrated and said goodbye. “Seeing Ken surrounded by family he never would have gotten to see again while in the hospital, watching him get to share a father-daughter dance with Chandra on her wedding day, and having him tell me that this day meant more to them than we would ever know were some of the most moving moments I’ve witnessed as a nurse,” Amy said. “I am so thankful for the team we have here. I know that this beautiful day wouldn’t have happened without the help of every single person who gave their time, money, creativity and passion to make it a day to remember.”
Read More About Helpful Caregivers Make a Wedding Dream Come True



.png?rev=fcd27802b7604a96bf1056b050ef90c5)