Buscar
-
Departamento destacado: Facilities Engineering
When an appliance or fixture stops working at home, who do you contact? If your lights stop working, you call an electrician. Is your air conditioning unit out of order? Reach out to an HVAC (heating, ventilation and air conditioning) technician. What about if your sewer drains start backing up? Time to contact a plumber. And if your fire safety equipment needs servicing? Better call a fire safety technician. Regular maintenance and repairs on the inner workings of your household are always important, and when something goes wrong, it can be distressing and inconvenient to you and everyone living with you. You feel the need to get the issue resolved as quickly as possible, right? Now imagine that those needs are magnified – to the tune of hundreds of thousands of people every year. Who could potentially take on such a monumental task? Enter: Facilities Engineering at Renown Health. Crucial to ensuring our health system performs at its peak, these team members step in to make sure every patient, team member and visitor who walks through any of our doors are able to access the facilities they need and make their time with us as comfortable – and as successful – as possible. The Silent Heroes As our care teams move heroic mountains to save lives, another set of heroes emerge behind-the-scenes. As a strong backbone of our health system, the Facilities Engineering department plays a key role in maintaining the infrastructure that supports patient care, from ensuring the HVAC systems are functioning optimally to maintaining the plumbing and electrical systems that keep the lights on and the equipment running smoothly. Renown is fortunate to have some of the most dedicated journeymen in the business. This team boasts many experts, including: Plumbers Fire Safety Technicians Craftsmen HVAC Journeymen Electricians Boiler Operators Facilities Technicians As one can imagine, every day brings on a new challenge for our Facilities team members. “Each workday is always different; it could be water, power or HVAC issues or anything in between,” said Nhil Dado, Supervisor of Facilities Services. “We are proud of the services we provide for the needs of patients and employees.” “Every day, we have a variety of equipment to work on,” added Alfred Santos, HVAC Journeyman. “Whether it’s facility upkeep, plumbing, HVAC or electrical, we want to help,” added Brian McCarty, Facilities Technician. This department works around the clock to ensure that every aspect of our hospitals and outpatient care locations meets the highest standards of safety and efficiency, from routine maintenance and equipment improvements to emergency repairs. These are huge responsibilities – all of which they perform with pride. “As an HVAC journeyman, we are responsible for making sure the air circulating in the hospital is clean,” said Christopher Bobis, HVAC Journeyman. “It is also our job to make sure the air is positive and negative in isolation rooms and ensure patients are satisfied with the temperature in their rooms.” “In addition to performing regular maintenance tasks like changing air and water filters, we complete any random work order that may come up,” added Brett Courtney, Facilities Technician. “We also recently switched out our lighting at Renown South Meadows to LED lights, which helps with energy savings.” “I overlook the boiler house equipment and coordinate the fixing of maintenance issues reported by hospital staff,” added Arnt Utnes, Boiler Operator. “We also respond to every single alarm." It’s difficult for us to imagine what our health system would be like without the Facilities team providing us with the comfortable and safe environment our patients need and deserve. Luckily, we’re never alone in our efforts to keep us running, and this department expertly leads that charge. “Along with writing down the PSI readings in the gas rooms and answering calls from dispatch and the boiler rooms, I go through all the daily work orders and complete them,” said Ken Carrillo, Facilities Technician. “It always feels good to see when we complete all the work orders for the day, especially as the next shift arrives.” “We fix, replace and dispose of pieces that are no longer in service – bottom line, we help keep the building up and running,” added Alejandro Cardenas, Craftsman. But it doesn’t stop there – Facilities Engineering is currently in the midst of creating a whole new fleet vehicle program to improve the operations of our many on-site vehicles, including trucks, forklifts and more. “I am the point of contact for all things fleet,” said Michelle Bay, Administrative Assistant. “We are building a new fleet program and working closely with leadership to move the program forward. I am involved with setting up new fleet fuel cards and can set up the program in the best interest of our internal customers while looking to the future for growth.” It’s clear that the Facilities team is indispensable to Renown. Through their expertise, professionalism and commitment to quality, they stop at nothing to keep our health system functioning at its highest level.
Read More About Department Spotlight: Facilities Engineering
-
Departamento destacado: Float Pool
Ring in the New Year and the rest of the holiday season by celebrating Renown’s Float Pool team! After coming out of the COVID-19 pandemic, it's no mystery that healthcare across the country has shifted and adapted to the growing needs and new demands of our patient populations. Renown Health is no different. As the largest not-for-profit health system in the region, we are no stranger to change, even when change presents challenges. Who do we call on when a unit needs more team members in the eleventh hour? Who can help when our patient volume spikes up with seconds to spare? This is where the Float Pool at Renown comes to the rescue. Skilled in a wide variety of healthcare specialties, from acute care nursing and critical care to care aiding and patient safety, this is the team that can seamlessly step in to provide crucial patient care to the units that need it most, whether a team is understaffed for the day or needs extra all-hands-on-deck for a specific patient or procedure. Float Pool team members are equipped to work in virtually any clinical area at Renown, making a genuine difference with every patient they encounter. A Pool of Relief Teams across Renown can breathe a sigh of relief knowing that Float Pool has their back in times of need. As the backbone of our health system, these dedicated team members possess a wealth of clinical knowledge and the ability to navigate diverse medical environments. Their flexibility allows them to fill staffing gaps and provide essential support to many different units. “We fill in the gaps of staffing to make everyone's day better,” said Patti Crepps, Critical Care Float Pool RN. “A float nurse has to be flexible and able to adapt to different situations and places – basically, ‘go with the flow.’ Patient care is basically the same all over; we make patient care possible by being familiar with all the various specialties and providing the specific care needed depending on the population we are taking care of on that shift.” “Float Pool staff members are like healthcare chameleons, transitioning between different departments,” added Shelby Riach, Acute Float Pool RN. “We incorporate flexibility, teamwork and a commitment to ensuring patients receive the best care, regardless of the setting or circumstances.” This team thrives in uncertainty; in fact, no workday is the same in Float Pool – and that’s exactly the way they like it. Working with many different teams across a multitude of specialties, these Care Aides, RNs, Critical Care Techs, Patient Safety Assistants (PSAs), Certified Nurses Assistants (CNAs) and more enjoy facing change, while they all share a goal of providing the best patient care possible. “No day looks the same; since we are the Float Pool, we are assigned a different assignment on Smart Square every day, whether it be as a care aide, a patient safety assistant, a unit clerk or patient transport,” said Melina Castenada, Care Aide. “If we are assigned as a care aide on the floor, we help assist with call lights and help with whatever nurses and CNAs may need, including feeding, transporting, walking, helping patients use the restroom, etc. When we are assigned as a PSA ‘sitter,’ we sit for the patient to help keep them safe. If we are assigned as unit clerk, we help answer phones and direct patients appropriately, file paperwork, answer call lights if needed and assist with office work.” “I love that every day is a different floor with different tasks and a different atmosphere,” added Julia Chappell, Critical Care Technician. “I find out which floor that I will be on right before my shift starts and head to the floor to find out my assignment for the day. Depending on the specialty, such as the medical-surgical floor versus an intensive care unit (ICU), my daily job tasks can vary.” When it comes to high-risk patients, who require special attention, PSAs within Float Pool step in to help. “The PSA role within Float Pool largely consists of adverse event prevention for our high-risk patients, and being a Float Pool employee allows us to work wherever we are needed,” said Dimitri Macouin, Patient Safety Assistant. “Whether it be in the emergency department, neurology or pediatrics, the PSA will be the eyes and ears for the nurses working with this patient population.” “Great strides have been made to ensure that PSAs remain vigilant and are recognized as an integral part of the patients' care team rather than 'just a sitter,’” added Karla Phillips, Patient Safety Assistant. Float Pool also oversees our Discharge Lounge, which offers patients and their families a dedicated space to reconnect and prepare for their discharge from the hospital. “The increase in utilization of the Discharge Lounge is something we are very proud of,” said Kara Abshier, Care Aide. “We assist in discharging patients from all over the hospital to help the floor and get new patients into rooms.” Every day brings a new challenge for Float Pool. As these team members wake up with uncertainty, they are ready to embrace the diverse demands of caring for patients of all ages. “The fact that Float Pool exists is amazing,” said Hannah Luccshesi, Acute Float Pool RN. “We wake up with no clue as to whether we will be working with babies, children or adults and then fill in the needs of the hospital.”
-
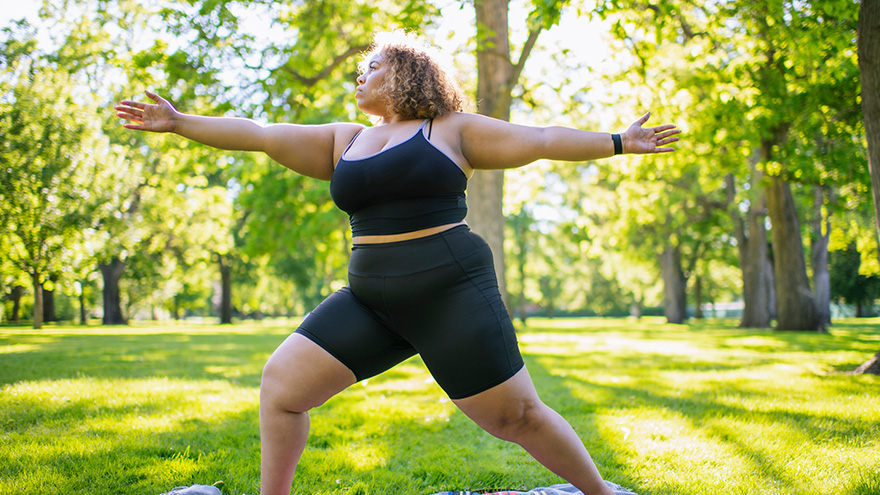
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Sepsis: Causes & Symptoms
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Departamento destacado: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Your Top 5 Questions about TAVR Answered
Your heart is the muscle in charge of pumping blood to your entire body. This vital organ is made up of chambers, valves and blood vessels. Your heart valves work similarly to a one-way door: they open and close, controlling blood flow in the correct direction through the heart chambers. For patients who have been diagnosed with a heart-related condition like aortic valve stenosis (narrowing), it is important to know treatment options. Most might think open-heart surgery is the only way to treat a heart valve, but many hospitals, including Renown, also offer a minimally invasive procedure called a Transcatheter Aortic Valve Replacement (TAVR). Dr. Abhilash Akinapelli of Renown Institute for Heart & Vascular Health shares his answers to the top five TAVR questions: 1. What causes aortic valve stenosis? Aortic valve stenosis can be caused by a variety of factors. The main reasons being wear and tear of the valve due to aging; genetically abnormal heart valve (bicuspid aortic valve); long-standing high blood pressure; and other reasons like radiation exposure. 2. Am I a candidate for TAVR? Renown’s heart care teams are made up of your primary care provider, cardiologist and cardio thoracic surgeon. They will evaluate if patients are a good candidate for the TAVR procedure by performing a variety of screenings and tests. Some of these include: Echocardiogram Electrocardiogram (ECG or EKG) Chest X-ray Exercise tests or stress tests Cardiac computerized tomography (CT) scan Cardiac catheterization 3. What are the advantages of the TAVR procedure? The Transcatheter Aortic Valve Replacement (TAVR) procedure is much less invasive than open heart surgery, otherwise known as a Surgical Aortic Valve Replacement (SAVR). Patients can typically return to their normal lifestyles within a week after leaving the hospital. During the TAVR procedure, a stent valve mounted on a balloon is advanced to the heart through the blood vessels in the groin without any incision. Once in position, the balloon will be inflated to firmly expand the new valve inside the diseased old valve, pushing it away to the sides. Once the new valve is in place, it begins working immediately and the deflated balloon is removed. The surgical procedure is approximately one hour long. Patients can get up and walk after four hours and will be discharged the following day if no complications arise. Compared to a SAVR, recovery time is much shorter and less risky for patients above the age of 75. A big advantage for anyone who fits under the criteria for a TAVR. 4. Is the procedure painful? The TAVR procedure is not surgery, but you will still be asleep during the procedure. Since no incision is made, it is essentially a painless procedure. Patients may experience slight discomfort such as aches and pains at the entry site of the catheter. 5. Can I have an MRI and X-rays done after having a TAVR valve? Yes, patients can have MRI scans and X-rays after TAVR. For further questions and information about the TAVR procedure, please consult with your Renown heart care team at 775-982-2452 or through MyChart.
-
Departamento destacado: Surgical Preadmission
Heading into surgery of any kind can bring along feelings of intimidation. With a best-in-class surgery team at Renown Health, patients rest assured that they are in the most capable hands for their entire procedure from start to finish – and while the physical preparation is vital, mental and emotional preparation is equally as important to ensure each patient has a smooth and comfortable experience. The Surgical Preadmission department (a.k.a. “preadmit”) at Renown Regional Medical Center and Renown South Meadows Medical Center is a dynamic and compassionate group of nurses, case managers, chart managers and more who are dedicated to guiding each patient through the surgical process. With extensive knowledge and expertise under their belt, the teams are equipped to make a genuine difference in the health and well-being of all patients, for all surgeries, at all times of the year. Surgery Starting Ground The Surgical Preadmission teams are crucial aspects in the successful outcome of every surgical procedure. Comprised of skilled healthcare professionals, this department is dedicated to providing comprehensive support and care before heading into the pre-operating room. “Our job is to prepare every patient for surgery, make sure all their pre-surgery testing is done, ensure they understand their fasting and medication instructions, have had their questions answered, have a ride home and know what to expect during surgery and after so their recovery can go smoothly and without complications,” said Debra Bennett, RN, Supervisor of Surgical Preadmission at Renown Regional. “Each patient is unique, so each experience is different.” Our preadmit nurses are the masters of communication, directing thorough assessments – including medications, tests and clearances – and addressing any questions or concerns patients may have, never missing the opportunity to inform them of exactly what they will expect in surgery. “I do a complete history on every patient while giving them detailed pre-operating instructions and helping them answer any questions to the best of my ability,” said Nancy Hilts, Surgical Preadmission RN at Renown Regional. “I am proud to be able to help allay their fears and concerns using my 30 years of pre-op experience. I offer an avenue for them to feel comfortable opening up to me.” “We always tell patients that they have great surgeons and a fantastic team that will be watching over them and taking care of them every step of the way,” added Jon Capallupo, Surgical Preadmission RN at Renown South Meadows. “We also give them plenty of educational handouts and video content, in addition to verbal instruction, to ensure they are as prepared as possible.” The nurses then pass the reigns onto the chart managers, who prepare the charts for surgery and ensure all documentation is up-to-date before sending them to the pre-operative team. The expert surgical case managers also step in to prepare a thorough discharge plan, along with reviewing pre-operation orders for status, consent, codes and more. The team does several of these initial visits virtually, and they are looking forward to soon phasing all preadmit case manager preliminary visits into a virtual model. From assisting the pre-op and post-anesthesia care unit (PACU) teams with discharge planning concerns to helping on the outpatient side with anything from oxygen equipment and catheters to transportation issues and those experiencing homelessness, our pre-admit case managers are always up to the challenge. "We are true patient advocates, alleviating concerns and fears along the way,” said Mary Carl, RN, Case Manager at Renown Regional. “Just to name a few things we do on a daily basis, we see our total joint and non-weight bearing patients during their preadmission appointment, so they are aware of the medical equipment they need and if it is covered by insurance; provide education for Aspira catheters and gastrostomy tubes; advocate to ensure tube feeding and dressing changes are set up for hospice and home health patients; and escalate concerns of patient safety to ensure a safe discharge.” In the midst of it all, there is never a dull moment in the preadmit teams. At Renown Regional alone, the preadmit professionals see more than 1,600 patients a month – and each one has a hyper-personalized experience with their very own preadmit team. “Many times, we are the first impression a patient has on our organization; after all, we touch more than 97 percent of patients that are scheduled for surgery, cardiac catheterization lab procedures or interventional radiology,” said Amy Schler, Surgical Preadmission RN at Renown Regional. “We also collaborate with many other departments in the hospital as well, from surgeons and anesthesiologists to case managers and nurse navigators. Our work in preadmit impacts the entire surgical process.” Holding a diverse array of experiences, our preadmit department plays an integral role in our commitment to providing the highest quality of care to every patient. Knowledge is Power Heading into surgery feeling fearful and worried is normal for any patient. However, how would you feel knowing that each individual member on your preadmit team has, on average, 23-25 years of experience in the field? This is the reality for our Surgical Preadmission department – and they put that vast knowledge to great use to bring a sense of calm to patients. “Our team members have worked in various departments within our organization, and they bring a wealth of knowledge that we share with each other, and most importantly, with our patients,” said Amy Schler, RN. “If you have hundreds of years of nursing experience, you can speak not only as a nurse but also as a patient. It allows you to give a more personal perspective on what patients can expect in their recovery. Being able to assess their emotions and provide feedback to our pre-op and PACU teams help the patient have a better experience.” “Many of our nurses have close to 40 years of experience each, and they have an extremely large knowledge base since we see patients from newborn to geriatric and from easy procedures to complex surgeries,” added Debra Bennett, RN. “Another great aspect of our team is the varied nursing backgrounds we all hold – surgery, pre- and post-op, labor and delivery, pediatric intensive care, cardiology, gastroenterology, urology, cardiac cath lab, home health and everything in between. Communication between departments is so important!” All members in this department, regardless of which clinical area they came from, surgical or non-surgical, can easily translate their skills into the work they do in preadmit – and they only continue to grow. “As a surgical preadmission nurse, I have used my years of experience as a nurse in surgical services,” said Terri Delatorre, Surgical Preadmission RN at Renown Regional. “I started as a floor nurse with orthopedics for 12 years, and then I worked with the PACU for 11 years. This has helped me give great understanding and care to our surgical patients.” “Because we have staff with such a vast knowledge base, we can rely on our years of working within our organization to help alleviate fears that the patient may have,” added Amy Schler, RN. We can prepare them for what to expect in pre-op and PACU and educate them on what to expect post-op, including any barriers they may face. For example, mastectomy patients may not realize they will not be able to raise their arms for 7-10 days post-op, and total knee patients have to navigate stairs and housing access. Helping patients think about barriers at home that they may not have thought about helps them prepare prior to surgery, enhances their healing and provides a better surgical experience.” The preadmit team works closely with our best-in-class surgeons and anesthesiologists, continuing to grow their expertise along the way while learning alongside our talented providers. For instance, when it comes to our Renown South Meadows preadmit department, anesthesiologist Nariman Rahimzadeh, MD provides excellent guidance for the entire team on state-of-the-art anesthesiology practices. “I am very proud of the work we do with Dr. Rahimzadeh,” said Lisa Closson, Surgical Preadmission RN at Renown South Meadows. “Together, we ensure patients are safe for both surgery and anesthesia.” Despite the challenges that come their way – whether it be changes to process and workflow to navigating support for patients after they leave the surgery floor – the preadmit team cleverly uses their collective wealth of knowledge to bring hope and comfort to all patients. “Our nurses are such warm, caring and compassionate humans that do their best to ease any fears and anxieties patients may have,” said Debra Bennett, RN. The Pride of Preadmission The pride of our preadmit team lies in their ability to make a positive impact on all patients they serve. To them, their work is not just a job – it's a calling. And they do it all while working together to elevate their team and performance. “Our team is most proud of the quality of care we provide to our patients and our abilities to troubleshoot difficult situations to ensure they have a great surgical experience here at Renown,” said Mary Carl, RN. The entire department supports each other by working collaboratively and relying on each other’s expertise to provide the best possible care for patients. They understand that their success as a team depends on their abilities to support and help each other. “Our team is awesome here at South Meadows,” said Jon Capallupo, RN. “We can turn to each other for support, and we all work very well with each other. I am glad to be a part of this team.” “I am proud of how well all of us in preadmit works with each other every day,” added Lisa Closson, RN. “We try to make patients feel comfortable from the moment they arrive to the time they leave the department.” The pride that our preadmit team expends goes beyond their departmental limits – these team members are also trusted teachers. They work closely with cancer nurse navigators to teach weekly classes for patients who have been newly diagnosed with breast cancer, coupled with lymphedema prevention and education classes. The team also encourages participation in Renown’s free smoking cessation programs to help their patients learn the risks and benefits of quitting smoking. When not serving patients or teaching classes, you can find many of these team members taking charge of multidisciplinary committees within our health system, including breast leadership, gastroenterology leadership, shared governance, infection control and recruitment and retention. On top of it all, this team certainly knows how to celebrate, with several of their members being a part of their own department-wide Celebration Committee, where they gather for retirement parties, baby showers and team get-togethers. Always active and never passing up a challenge, our preadmit department are shining examples of Renown’s Culture Commitments, especially Caring and Collaboration, and the pride in the vital work they do every day is limitless. “I am so happy my position in preadmit opened up for me at a time when I was really feeling challenged in my career,” said Nancy Hilts, RN. “The team that we have here is amazing. I am so grateful and thankful every day for the opportunity. It is an amazing place to work!”
-
Building a Better Birth Team
Giving birth expends as much energy as running a marathon. And just like you would only run a marathon with training beforehand, there are exercises you can do to prepare for birth. But instead of a coach, you'll have your birth team. Your birth team exists to help you navigate pregnancy and labor and support your choices. Let's say you've never put together a birth team before and are wondering where to start. Today we'll go over the three main positions to fill for your birth team's starting lineup. Birthing Person The birthing person is the leader of the team. After all, you can't have a birth team without someone giving birth. This person could be the baby's mother, gestational surrogate, birth parent before adoption, a transgender father or a non-binary parent. If you are not the birthing person, don't presume to know what the ideal labor and birth circumstances should be. And if you are the birthing person, don't allow anyone else to tell you what you want. This is your body and your birth; you are the boss in the birth room. Doula No birth team is complete without a doula, and although doulas have increased in popularity lately, many people still don't know what a doula is. Simply put, a doula is a birth professional – not a medical provider – who offers emotional, physical and informational support during pregnancy, labor and beyond. Most doulas' services include at least one prenatal visit and one postpartum visit, as well as continuous care throughout active labor. Some doulas provide more than one prenatal/postpartum visit, so be sure to ask what is included in their fee. Even if you have a partner who will support you during labor, studies have shown that a doula can significantly increase your likelihood of a positive birth outcome. Even the most supportive partner needs to rest, and a doula can ensure that you still get the care you need while your partner gets a break. Midwife or Obstetrician Finally, you'll want to choose the medical professional who will attend your birth. Many folks choose to give birth with the OB/GYN who does their annual check-ups, but there are many reasons someone might choose a different provider for their birth. The first step to finding the best attending provider for your birth is to decide which model of care aligns closest to your values and goals: the Midwifery Model of Care or the Medical Model of Care. .tg {border-collapse:collapse;border-spacing:0;} .tg td{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; overflow:hidden;padding:10px 5px;word-break:normal;} .tg th{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; font-weight:normal;overflow:hidden;padding:10px 5px;word-break:normal;} .tg .tg-gqvw{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-weight:bold; text-align:left;vertical-align:top} .tg .tg-8vim{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-size:18px; font-weight:bold;text-align:left;vertical-align:top} .tg .tg-qm8j{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;text-align:left; vertical-align:top} .tg {border-collapse:collapse;border-spacing:0;} .tg td{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; overflow:hidden;padding:10px 5px;word-break:normal;} .tg th{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; font-weight:normal;overflow:hidden;padding:10px 5px;word-break:normal;} .tg .tg-gqvw{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-weight:bold; text-align:left;vertical-align:top} .tg .tg-8vim{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-size:18px; font-weight:bold;text-align:left;vertical-align:top} .tg .tg-2rvk{background-color:#ffffff;color:#000000;font-family:Arial, Helvetica, sans-serif !important;text-align:left; vertical-align:top} Midwifery Model of Care Medical Model of Care Philosophy Birth is physiological. Birth is potentially pathological. Interventions Medical interventions can cause more complications, and therefore are only used as needed. Medical interventions should be used, even in non-emergency situations and sometimes as preventative measures. Decisions Birthing person is the key decision maker. Medical professional is the key decision maker. Provider’s Role Providers monitor labor and will intervene or transfer to hospital if needed. Providers assess and control the birthing process.
-
Your Ultimate Cold and Flu Survival Guide
While viruses can attack year-round, colds, flus and other respiratory illnesses are typically more prevalent during fall and winter. People spend more time indoors, which allows viruses to pass more easily from one person to another. The cold, dry air can also affect the respiratory system, making it more susceptible to germs. According to the CDC, flu activity in the U.S. often begins to increase in October and peaks between December and February. “Flu season” can last as late as May. When it comes to the cold and flu, prevention and preparation are key. Getting the flu shot and a COVID-19 vaccine is the first and most crucial step in protecting against these two respiratory illnesses. Preventative actions, such as washing your hands, covering your mouth and nose when coughing or sneezing and getting enough sleep can also help you avoid getting sick. However, despite your best prevention efforts, the time may come this winter when you start to feel a little scratch in your throat or a fever coming on. By taking steps ahead of time to assemble a cold and flu survival kit, you’ll be more prepared for whenever illness strikes, allowing you to stay home, rest and avoid spreading germs. Tips for Managing Symptoms Keep these tips in mind to ease your cold or flu symptoms: Stay home and rest Drink plenty of fluids Treat aches and fever with over-the-counter medication such as ibuprofen or acetaminophen Manage a cough with over-the-counter expectorants or suppressants Run a humidifier or sit in a steamy bathroom to ease congestion What to Stock in Your Flu Survival Kit Be ready when a cold or the flu strikes by having a flu survival kit filled with these get-well essentials stocked in your pantry, fridge and medicine cabinet: Over-the-Counter Medications: Take advantage of over-the-counter medications to make yourself feel better and ease most common flu symptoms of fever, headache, cough, muscle aches, sore throat, and runny or stuffy nose Pain relievers - Ibuprofen (Motrin and Advil) or Acetaminophen (Tylenol): for fever and aches Decongestants: for sniffles and congestion Cough expectorant (guaifenesin): for a “wet” cough to help clear secretions from the lungs Cough suppressant (dextromethorphan/DM): for a severe “dry” cough to block the cough reflex Cough syrups and drops Drinks: Water Herbal tea Low-sugar sports drinks Pedialyte Foods: Chicken soup Broth Vitamin C-containing fruits and vegetables Oatmeal Toast (add some avocado, honey or egg) Miscellaneous items: Tissues Lozenges Protective mask Thermometer Humidifier When to Seek Care and Where to Go Most healthy adults who have a cold, the flu, or other mild respiratory illnesses don’t need to see a care provider and will recover at home with self-care measures. Because these are viral illnesses, antibiotics won’t work against treating them. Your care provider may be able to prescribe an antiviral medication that can relieve your symptoms and shorten the duration and severity of your illness; however, this needs to be started within 48 hours of symptom onset and is often only prescribed to individuals at high risk for developing complications from the flu or those experience severe symptoms. Primary Care or Urgent Care Contact your primary care provider or visit an Urgent Care if you are at an increased risk, including those who: Are 65 years of age or older Have chronic medical conditions Are pregnant or recently gave birth Have a weakened immune system Find a primary care provider If you are otherwise healthy and not at increased risk of complications, seek medical advice if your flu symptoms are unusually severe, such as mild difficulty breathing, a severe sore throat, coughing that produces a lot of green or yellow mucus, or feeling faint. Emergency Care Go to the Emergency Department if you are experiencing emergency warning signs such as severe pain (chest, abdomen), concern for heart attack or stroke (slurred speech, new localized weakness), severe dehydration (needing IV fluids) or severe shortness of breath.
-
Excellence in Heart Care Changes a Patient's Life
Being diagnosed with a chronic heart condition like atrial fibrillation (A-fib) can shift the course of your entire life. Embracing heart medications and lifestyle changes become your norm, and thanks to advancements in medicine and medical technology, managing the condition can bring you to a new sense of normalcy. But what if a different option was possible – one that would make medications and activity limits a thing of the past? This became the reality for Renown Health patient Richard Preyer after receiving a hybrid catheter ablation. Thanks to the vigilant surgical care of Shining Sun, MD, a cardiologist at the Renown Institute for Heart & Vascular Health, and his compassionate team, Richard has a new lease on life. Minimally Invasive with Maximal Results An A-fib patient since 2010 who had been living with an unfinished ablation, the 59-year-old Carson City resident turned to the internet to look for alternate solutions. He had heard that the Renown Institute for Heart & Vascular Health was a top-tier location for cardiovascular care. “I changed health insurance plans through Nevada Health Link to ensure I could see a Renown cardiologist,” said Richard. Choosing a cardiologist was an even easier decision for Richard. Dr. Sun’s introductory Find a Doctor video on Renown’s YouTube channel, where he displayed his expertise and determination, was more than enough for Richard to choose him as his cardiac care leader. At his first visit, Dr. Sun reviewed Richard’s records, and noted his prior unfinished ablation. The nine-hour procedure had been performed several years ago. With the enhanced technologies at Dr. Sun's disposal, Richard was excited at the thought of his life potentially being changed for good – with a minimally-invasive solution. Dr. Sun collaborated closely with Richard’s previous and current care teams – including a surgeon who performed a maze operation on him right before his surgery at Renown, to ensure his hybrid ablation was tailored uniquely to him. “Dr. Sun is clearly a very powerful cardiologist with many connections, and the coordination between his team and my other doctors was great,” said Richard. After working on the exterior of the heart in the first phase of the surgery and the interior of the heart during the second phase, Richard’s hybrid ablation was successful, completing the unfinished portion of his previous ablation. “Fixing A-fib can take one to three ablations, and sometimes it never holds,” said Richard. “That is one of the largest reasons why I am so thankful for this procedure and how it ended up.” Life After A-fib Now comes the long, arduous healing process, right? Not for Richard. With only eight incisions (four on each side of his chest), he was able to remove his bandages after two days, and he healed completely in one week. “I was even back to taking three-mile walks within a week of my operation,” said Richard. No more blood thinners. No more activity limits. And most importantly for Richard, no more heart-stabilizing medications that came with side effects he didn’t enjoy. He attributes his enhanced life to Dr. Sun and his team. “I highly recommend Dr. Sun and everyone that works with him,” he said. “Everyone in the group, from the nurses and anesthesiologists going above-and-beyond to the schedulers who helped me navigate the appointment process, made me have a lot of confidence. Their calm demeanors made so much difference.” Today, Richard now enjoys elongated walks in the northern Nevada outdoors, exotic vacations with his wife and, as he describes, “feeling like I’m in my 40’s again.” Learn more about the region's leader in cardiac health, heart and vascular care here.
Read More About Excellence in Heart Care Changes a Patient's Life
-
Take a Stand Against Domestic Violence
October is Domestic Violence Awareness Month in the United States. We spoke with Renown Health experts and local domestic violence prevention organizations who gave us a deeper look into understanding the warning signs of abuse and the many proactive and reactive resources in our community that you can reach out to today. Domestic violence, also referred to as domestic abuse, is an everyone issue. Whether you identify as male or female, an adult or a child, single or partnered – domestic violence can affect anyone. In fact, it may be closer to home than you might think. According to the Nevada Quality Parenting Initiative, in Nevada, 43.8% of women and 32.8% of men experience domestic violence in their lifetime, and the risk of that figure rising is imminent. This year alone, the Domestic Violence Resource Center (DVRC) in Reno experienced a 55% increase in overnight emergency stays, according to the Reno Gazette-Journal. This problem also, unfortunately, extends to children. More than 5,000 children in Nevada were reportedly primary or secondary victims of domestic abuse in 2021, as stated by the Nevada Coalition to End Domestic and Sexual Violence. “Domestic violence can manifest in many different ways,” said Kami Price, Supervisor of Social Services for Renown Health. “Abuse isn’t always strictly physical. It can also be emotional, verbal, sexual and even digital. Understanding those differences can help you prepare accordingly and respond safely if you or a loved one are experiencing domestic violence.” Knowing what to look out for is crucial in protecting yourself and others against the effects of domestic abuse and taking action when warning signs appear. The National Domestic Violence Hotline shares the common signs of an abusive partner, no matter how old they are or what gender they identify as: Telling you that you never do anything right. Showing extreme jealousy of your friends or time spent away from them. Preventing or discouraging you from spending time with friends, family members or peers. Insulting, demeaning or shaming you, especially in front of other people. Preventing you from making your own decisions, including about working or attending school. Controlling finances, including taking your money or withholding money for needed expenses. Pressuring you to perform sexual acts you’re not comfortable with. Pressuring you to use drugs or alcohol. Intimidating you through threatening looks or actions. Threatening to harm or take away your children or pets. Intimidating you with weapons. Destroying your belongings or your home. "People experiencing domestic violence may feel as though they are trapped,” said Kami Price. “The reality is – this often couldn’t be further from the truth, especially with the resources we have at our disposal in northern Nevada.” Respected Resources Ending the Silence on Domestic Violence While these facts and figures might be staggering, those experiencing domestic violence at any age are not alone. There is hope at the end of the tunnel, especially here locally. Devoted to meeting the growing needs of the communities we serve, Renown Health proudly supports and sponsors several organizations in our community that are committed to educating children and adults on the signs and symptoms of domestic violence, along with what each child and family member can do today to prevent abuse in the household. These essential organizations are on the frontlines of shifting attitudes from “I don’t want to get involved” to “How can I help?” Serving children across northern Nevada, the Child Assault Prevention (CAP) Project offers “education and prevention programs designed to increase children’s safety from bullying, abuse and assault” and break the cycle of domestic abuse. During 2021 and the first half of 2022, CAP led about 500 different workshops, teaching 10,000 second-grade and fourth-grade children in Washoe, Storey, Lyon and Churchill Counties how to keep themselves safe from domestic violence. “As domestic violence is on the rise, open communication, early intervention and education are key to protecting children from the effects of domestic violence," said Rebecca LeBeau, Executive Director of the CAP Project. “That’s why I begin speaking about child assault prevention and stranger danger to kids as young as six years old. It's important to explain the true reality of domestic violence to both children and adults, tailoring language specifically to whatever age they are, and allowing them to process it. Kids of all ages will learn how to deal with extremely dangerous situations this way.” According to Rebecca, common symptoms of abuse to be on the lookout for at school include grades dropping, a lack of focus and feelings of not wanting to return home after the school day ends. If someone in a child’s home is being hurt or abused, children are always encouraged to speak with a trusted adult or school counselor. From there, organizations like the CAP Project develop a safety plan moving forward. Adults and family units aren’t alone either. The DVRC provides a wide variety of services to Washoe County residents experiencing domestic abuse. To date, the DVRC has helped more than 100,000 victims of domestic violence, and with the recent launch of their crisis text line, they are poised to serve many more. Like the CAP Project, the DVRC also believes that education is one of the first lines of defense against domestic violence. “Education on what domestic violence looks like is so much more than talking about physical violence,” said Aria Overli, Volunteer Coordinator at the DVRC. “Educating the community, and particularly youth, about what healthy relationships look like is a major factor in preventing abuse. Understanding the intersection of how other issues – such as race, mental illness and immigration status – affect domestic violence risk factors is key to addressing those issues.” The list doesn’t stop there. Renown Health Foundation has provided financial support for many more organizations that are dedicated to ending the silence on domestic violence, sexual violence and family abuse, including: The Children’s Cabinet – A child-focused organization offering many support services for youths and families, including Safe Place, a program that partners with local businesses to offer safe locations for children to seek help if they feel threatened at school or at home. The organization also provides free family counseling, providing a pathway to better communication for families experiencing a myriad of issues ranging from domestic violence to substance abuse. Awaken – A nonprofit committed to increasing awareness and education regarding sex trafficking and providing housing and healing to all survivors. Safe Embrace – The largest and most inclusive safe house in Reno-Sparks for survivors of domestic and sexual violence, offering a wide range of resources including counseling, emergency transportation, court support and more. Eddy House – A safe space for at-risk individuals aged 18-24 recovering from the effects of domestic abuse, unsafe housing conditions, homelessness and more. Being an advocate starts with us – if you see something, say something. Keeping a transparent line of communication is key to preventing, noticing and combating domestic violence. “The more you reach out and talk about the issues, the better,” closed Kami Price. “No one has to go through their struggles alone.”

.png?rev=fcd27802b7604a96bf1056b050ef90c5)