Buscar
-
Departamento destacado: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Your Ultimate Cold and Flu Survival Guide
While viruses can attack year-round, colds, flus and other respiratory illnesses are typically more prevalent during fall and winter. People spend more time indoors, which allows viruses to pass more easily from one person to another. The cold, dry air can also affect the respiratory system, making it more susceptible to germs. According to the CDC, flu activity in the U.S. often begins to increase in October and peaks between December and February. “Flu season” can last as late as May. When it comes to the cold and flu, prevention and preparation are key. Getting the flu shot and a COVID-19 vaccine is the first and most crucial step in protecting against these two respiratory illnesses. Preventative actions, such as washing your hands, covering your mouth and nose when coughing or sneezing and getting enough sleep can also help you avoid getting sick. However, despite your best prevention efforts, the time may come this winter when you start to feel a little scratch in your throat or a fever coming on. By taking steps ahead of time to assemble a cold and flu survival kit, you’ll be more prepared for whenever illness strikes, allowing you to stay home, rest and avoid spreading germs. Tips for Managing Symptoms Keep these tips in mind to ease your cold or flu symptoms: Stay home and rest Drink plenty of fluids Treat aches and fever with over-the-counter medication such as ibuprofen or acetaminophen Manage a cough with over-the-counter expectorants or suppressants Run a humidifier or sit in a steamy bathroom to ease congestion What to Stock in Your Flu Survival Kit Be ready when a cold or the flu strikes by having a flu survival kit filled with these get-well essentials stocked in your pantry, fridge and medicine cabinet: Over-the-Counter Medications: Take advantage of over-the-counter medications to make yourself feel better and ease most common flu symptoms of fever, headache, cough, muscle aches, sore throat, and runny or stuffy nose Pain relievers - Ibuprofen (Motrin and Advil) or Acetaminophen (Tylenol): for fever and aches Decongestants: for sniffles and congestion Cough expectorant (guaifenesin): for a “wet” cough to help clear secretions from the lungs Cough suppressant (dextromethorphan/DM): for a severe “dry” cough to block the cough reflex Cough syrups and drops Drinks: Water Herbal tea Low-sugar sports drinks Pedialyte Foods: Chicken soup Broth Vitamin C-containing fruits and vegetables Oatmeal Toast (add some avocado, honey or egg) Miscellaneous items: Tissues Lozenges Protective mask Thermometer Humidifier When to Seek Care and Where to Go Most healthy adults who have a cold, the flu, or other mild respiratory illnesses don’t need to see a care provider and will recover at home with self-care measures. Because these are viral illnesses, antibiotics won’t work against treating them. Your care provider may be able to prescribe an antiviral medication that can relieve your symptoms and shorten the duration and severity of your illness; however, this needs to be started within 48 hours of symptom onset and is often only prescribed to individuals at high risk for developing complications from the flu or those experience severe symptoms. Primary Care or Urgent Care Contact your primary care provider or visit an Urgent Care if you are at an increased risk, including those who: Are 65 years of age or older Have chronic medical conditions Are pregnant or recently gave birth Have a weakened immune system Find a primary care provider If you are otherwise healthy and not at increased risk of complications, seek medical advice if your flu symptoms are unusually severe, such as mild difficulty breathing, a severe sore throat, coughing that produces a lot of green or yellow mucus, or feeling faint. Emergency Care Go to the Emergency Department if you are experiencing emergency warning signs such as severe pain (chest, abdomen), concern for heart attack or stroke (slurred speech, new localized weakness), severe dehydration (needing IV fluids) or severe shortness of breath.
-
Top Safe Sleep Tips for Your Baby
Becoming a parent for the first time means lots of new unknowns – from learning to breastfeed and swaddle to buckling your newborn into the car seat for the first time. But when it comes to putting them to bed safely, it’s important to remember it really can mean life or death. It’s something we’re taught before our little one is even here: the correct way to put your baby to bed safely. Sadly though, the number of infant deaths continues to climb. The main culprit of sleep-related infant death continues to be all the items parents leave in the crib with their babies. According to the Center for Disease Control and Prevention, there are about 3,500 sleep-related deaths among babies each year. “The best advice is ‘bare is best.’ Keep your infant’s sleep space clutter free – no blankets, bumpers, toys or pillows,” said Karen Wagner, Pediatric Nurse Practitioner. Follow the ABCs for Safe Sleep Remembering the ABCs is an easy way to remember how to put your little one to bed safely. A: Alone No blankets, toys or pillows. “We do recommend using a sleep sack as a blanket alternative,” said Karen. “It prevents the risk of suffocation and keeps your baby warm.” Keep in mind, the greatest risk for suffocation happens when babies are under 1 year of age, so it’s best to save the toys, blankets and pillows for their “big kid bed,” or around 18 months old. B: Back The slogan “back is best” is another good reminder. Keeping your baby on their back until they’re old enough to rollover helps reduce the risk of Sudden Infant Death Syndrome (SIDS). C: Crib It is best to have your baby sleep alone in their crib. While co-sleeping may be enticing, especially after a late-night feed, it increases the risks of possible suffocation. However, “having your child in your room, in their own crib or bassinet, is protective for SIDS,” Karen said. “In fact, we think co-rooming reduces SIDS risk by almost 50 percent.” Co-rooming allows parents to keep new babies in close reach and helps parents oversee their baby’s sleep, just in case something happens.
-
What Foods to Eat and What to Avoid When Pregnant
Eating a well-balanced and nutritious diet when pregnant is one of the more essential things you can do for your baby and yourself. The basic principles of what to eat when pregnant are quite similar to how we should be eating all the time. This includes focusing on fruits, vegetables, whole grains, lean protein and healthy fats. Of course, there are a few areas that you should pay close attention to when you’re pregnant and a few foods you should avoid. We consulted Renown Health’s Caitlin Bus, RD, LD, CDE to learn more about pregnancy nutrition. Foods to Eat Regularly: Veggies Vegetables of all kinds -- and in all forms -- are beneficial for you and your baby during pregnancy. Veggies ensure your body is getting the fiber, vitamins and minerals it needs. However, fresh or frozen veggies are considered best, but if you choose to eat canned veggies, make sure you choose a low sodium product. The more greens, the better! If you have an aversion to vegetables, especially in the first trimester, try sneaking them into smoothies. Healthy Proteins Protein-rich foods support your baby's growth while giving your body the nutrients to build and repair tissues, including your muscles, hair, skin and nails. Although protein requirements vary from person to person, a pregnant woman needs additional protein for her baby's growth, especially in the second and third trimesters. Regularly eating high protein foods -- like fish, chicken, turkey, eggs, peanut butter, nuts and beans –– promotes your baby's healthy brain and heart development. Grains Food like brown rice, quinoa, whole-wheat pasta and oatmeal are great to eat while pregnant. They are rich in fiber, iron, B vitamins and folic acid, which are all beneficial to physical development. Grains also help alleviate constipation and hemorrhoids. Fruits Fruit can help satisfy any sugar cravings you have when pregnant while also supplying your baby with nutrients – it's a win-win. Some people advise against fruit consumption while pregnant, but this is a myth. Like with all foods, moderation is key. Fruit can be high in sugar, so it is important to be aware of your intake. Also, make sure you are mindful of your preparation – thoroughly rinse produce under running water for 30 seconds to help avoid foodborne illness. Pasteurized Dairy Dairy products like milk, cheese and yogurt can be great sources of protein and calcium needed for the healthy development of a baby's bones, teeth and muscles. These foods also help with ensuring healthy heart function and nerve transmission. When buying these products, make sure to choose pasteurized products to avoid exposing your body to germs and bacteria. The American College of Obstetrics and Gynecology recommends 1,000mg of calcium per day for pregnant and lactating women. This equates to 4 servings of dairy or calcium-rich foods such as leafy greens, broccoli, tofu, almonds or dried figs. DHA Omega-3 Fats Omega-3s like DHA help support the health of a baby's brain and parts of their eyes. Women who are pregnant or breastfeeding should eat at least 8 ounces and up to 12 ounces of seafood each week. Ideally, food sources that offer DHA omega-3 and that are lower in mercury should be emphasized in your diet, including fish like salmon, sardines and anchovies. If you do not eat fish or omega-3 fortified foods, a DHA omega-3 supplement is recommended. Choline Did you know that 92% of pregnant women fail to meet the daily choline recommendation? Choline is crucial for an infant's brain and central nervous system development. One egg supplies 33% of the recommended daily intake. Although choline is often absent or low in prenatal vitamins, the best food sources include eggs, meats, fish, dairy, navy beans, Brussels sprouts, broccoli and spinach. Iron and Folic Acid Iron is the most common nutrient deficiency during pregnancy. Foods with high and moderate amounts of iron include red meat, chicken, fish, fortified cereals, spinach and beans. Folic acid is used to make the extra blood your body needs during pregnancy. Consuming adequate folic acid early in pregnancy reduces the risk of birth defects that affect the spinal cord. It is recommended to consume 400 micrograms (mcg) per day for pregnant women. This amount is included in your prenatal vitamins. Water Staying hydrated is one of the best things you can do for yourself and your baby when pregnant. In addition to just being good for you, hydration alleviates morning sickness and nausea, while dehydration can lead to contractions and even pre-term labor. Aim for 10 cups of fluids per day, on top of the water naturally occurring in foods. Foods to Avoid: Raw Fish and Fish with High Mercury Content Sorry sushi fans, according to the Center for Disease Control and Prevention, pregnant women are 10 times more likely to get infected by Listeria, a bacteria found in raw or undercooked fish. Also, avoid fish often found to be high in mercury, including swordfish, king mackerel, tuna and marlin. Processed or Raw Meat Similar to eating raw fish, eating undercooked or raw meat increases your risk of infection while pregnant. Hot dogs and lunch meats should also be avoided, unless they have been reheated to be steaming hot (for example, in a microwave). Alcohol Drinking alcohol when pregnant can impact your baby’s brain development and increases your risk of premature birth, low birth weight or miscarriage. Just don’t do it! Minimize Caffeine High caffeine intake during pregnancy can restrict your baby’s growth; therefore, it is recommended that pregnant people limit their caffeine intake to less than 200 mg per day – that’s roughly two cups (16 fl oz) of coffee per day. Runny Eggs Eating raw or runny eggs when pregnant increases your risk of Salmonella, which can cause fever, nausea, vomiting, stomach cramps and diarrhea. Always make sure your eggs are cooked through or use pasteurized eggs.
Read More About What Foods to Eat and What to Avoid When Pregnant
-
La lactancia no tiene por qué significar dolor en los pezones
If you think sore nipples are just a normal part of breastfeeding, think again. Robin Hollen, APRN, and Breastfeeding Medicine Specialist, says that nursing can be an enjoyable experience for mom and baby without pain and discomfort. A top concern of nursing moms within the first week after delivery is how to prevent sore nipples. Even moms who’ve nursed before struggle with this common issue. While many women think it is a regular part of the nursing experience, it is actually a sign that something isn’t quite right. “Nursing your baby should be enjoyable,” says Robin Hollen, Breastfeeding Medicine Specialist with Renown Health. For over 30 years Robin has been supporting moms to breastfeed. Below she shares some valuable information and tips, helping you create a happy and healthy breastfeeding experience for you and your baby. What causes sore nipples? The most common cause of sore nipples involves incorrect latching. For a proper latch, a baby’s mouth takes in the entire nipple and some of the breast, so that the nipple rests at the back of the mouth where the palate is soft. With an improper latch, the mouth may slip down to the tip of the nipple while the baby nurses. This constant pressure on your sensitive skin may cause discomfort and pain. A board-certified lactation consultant can help assess if your baby is latched correctly and troubleshoot your breastfeeding concerns. Less common causes of sore nipples include: • Improper tongue placement of baby • Clenching • Incorrect breast pump use How can a mother prevent sore nipples from an improper latch? Breastfeeding is a learning experience for both mom and baby. Ask for help with the latch so your baby learns it correctly and maintains its depth. In the past, new mothers were surrounded by a community of women — their own mothers, grandmothers, or other family and friends — to provide assistance and guidance with every latch at the beginning of an infant’s life. In today’s culture, new moms can find themselves on their own with no extended family to lend their knowledge. Nurses, pediatricians and lactation consultants now fill that role; they are the eyes and hands along with the much-needed experience to guide new mothers. Our Breastfeeding Medicine experts assist nursing moms with latch every day. Even a single visit with a lactation consultant observing your breastfeeding baby can provide valuable insight on achieving, and maintaining, the proper latch - preventing future nipple soreness and discomfort. How to heal sore nipples from breastfeeding To heal sore nipples, you must first fix the cause, and correcting the latch prevents further damage. A lactation consultant can also help you address the pain. Below are some breast healing tips: • Your own expressed breast milk is excellent to rub into the nipple for anti-bacterial protection. • For those moms who need more lubricant or fat than breast milk offers, use a lanolin or a cream that is labeled safe for the baby. • Soothies are a gel pads providing comfort in between feedings, but should not be used with lanolin products. • Breast shells, not to be confused with shields, can guard the nipples from irritation or pressure in between feedings. If you have more questions about preventing and healing sore nipples or general breastfeeding concerns, talk to your pediatrician or a Renown Health Breastfeeding Medicine specialist at 775-982-6365.
Read More About Breast Feeding Doesn't Have To Mean Sore Nipples
-
4 Consejos sobre la lactancia para nuevas mamás
While breastfeeding is natural, it's not always easy. We asked Certified Lactation Counselor Sarah Mitchell for some tips to help make the process easier for mom and baby. From increased infant immunity to improved maternal health and well-being, the benefits of breastfeeding are many. Still, only 60 percent of U.S. moms in the United States continue to breastfeed past their baby's first six months. There are for many reasons for why moms stop, including the mother's their need to return to work. We reached out spoke to Sarah Mitchell, a certified lactation counselor at The Lactation Connection at Renown, for some expert advice. Tip 1 At first, it's normal to expect obstacles. Even in cultures where close to 100 percent of moms breastfeed, they can experience issues, including getting the baby to "latch on," sore nipples, and milk production. In addition, it sometimes can take several weeks for mom and baby to get comfortable. Tip 2 Line up a coach, even before the baby is born. This can be a professional lactation coach, family member, or friend who is experienced and encouraging. While online videos can be helpful, most new moms need the one-on-one guidance that a coach can provide. Renown offers outstanding resources in its Lactation Connection center, including expert consultants, products, and support. Tip 3 Well ahead of the due date, set up a support network of friends, family members, or community groups such as La Leche League. Women historically have relied on extended support systems to help them with raising children, and breastfeeding is one of those areas that, while natural, still needs encouragement from the women who’ve been there. Tip 4 Don’t get discouraged if you need to supplement at times with formula. This, too, as it turns out, is not uncommon in other cultures. In other parts of the world, babies are given beverages and foods such as tea, broth, soup, juice, mashed bananas, and papaya. The American Academy of Pediatrics recommends supplementation only with approved formula -- but the point is, it’s ok to supplement if you need to. Finally, don’t forget the importance of breastfeeding for connecting with your baby. It’s essential to maintain breastfeeding over the weekends, preferably “on-demand,.” and will keep that special bond strong after you have returned to your job.
-
Tips for Coping with Smoke-Related Health Problems
Millions of people across the west live in areas where air pollution can cause serious health problems. In addition, local air quality can affect our daily lives. Who is Affected? Kouros Farro, MD, a physician with Renown Urgent Care, advises that certain people are more likely to be affected when fine particle pollution reaches an unhealthy level. People who have asthma or other breathing conditions like chronic obstructive pulmonary disease (COPD). People who have heart disease or high blood pressure. Children and older adults. People of all ages who are doing extended or heavy physical activity like playing sports or working outdoors. “Everyone should take precautions when the air quality is unhealthy. Air pollution can aggravate heart and cardiovascular disease as well as lung diseases like asthma and COPD. When the air quality is unhealthy, people with these conditions may experience symptoms like chest pain, shortness of breath, wheezing, coughing, or fatigue. If you are experiencing any of these symptoms, use your inhalers as directed and contact your health care provider,” says Dr. Farro, who is board certified in family medicine and practices at Renown Urgent Care at 975 Ryland St. in Reno. “If you do not have a health care provider, there is a Renown Urgent Care office on almost every corner, with providers ready to see you.” Dr. Farro advises the following: Take it easy and listen to your body. Limit, change or postpone your physical activity level. If possible, stay away from local sources of air pollution like busy roads and wood fires. If you have asthma or other breathing conditions like COPD, make sure you have your relief/rescue inhaler with you. People with asthma should review and follow the direction in their written asthma action plan. Make an appointment to see your health provider to be sure you have an asthma action plan. Getting Same-Day Care Renown Urgent Care provides same-day treatment for a wide range of minor injuries, illnesses and medical concerns that are urgent but not life-threatening. Avoid the long wait times and high emergency room prices at 11 convenient sites, including Reno, Sparks, Carson City, USA Parkway, Fallon and Fernley. You can walk in or book ahead online. Make an Urgent Care Appointment Community Health Resources The Washoe County Health District offers online health information on its Smoke Smart website, including fire information, daily air quality information, fire and smoke maps and how to protect yourself. In addition, an online subscription page allows you to sign up for EnviroFlash, notifying you about air quality.
Read More About Tips for Coping with Smoke-Related Health Problems
-
Renown Regional Medical Center Recognized Among Nations Top Hospitals In Critical Care
The region’s only trauma center receives top honors from Healthgrades What is Healthgrades? Healthgrades, a leading national resource for trusted information about physicians and hospitals, recently announced the recipients of their 2021 Specialty Excellence Awards. These awards recognize hospitals with superior performance and have selected Renown Regional Medical Center in Reno, Nv. as northern Nevada’s top hospital for critical care. Hospitals in this ranking demonstrate excellent patient clinical outcomes in treating pulmonary embolism, respiratory system failure, sepsis, and diabetic emergencies. Health grades further distinguishes hospitals that stand out as America’s 100 Best Hospitals for Specialty Care™, with Renown Regional Medical Center identified as Nevada’s only critical care hospital to be bestowed with this honor. What this Award Means To Us “At Renown, I am honored to work beside dedicated healthcare heroes who are working tirelessly to make a genuine difference in the health and well-being of every patient and family we serve,” says Tony Slonim, MD, D.Ph., FACHE, president and CEO of Renown. “Having trained and served as a pediatric intensive care physician, this honor from Healthgrades does so much to recognize the compassion, skill, and determination of this incredible team. I join with our community in saluting the Renown Regional Medical Center’s critical care team as one of the best critical care hospitals in the nation.” “As the only accredited trauma center between Sacramento and Salt Lake City, we receive and care for critically-injured patients from over 100,000 square miles. Our communities depend on Renown Regional Medical Center for outstanding critical care,” says Dawn D. Ahner, DSc, FACHE, Chief Operating Officer, Acute Services. “Our multi-disciplinary critical care and intensive care healthcare teams are specially-staffed, equipped and designed to care for, closely monitor, and comprehensively care for patients with life-threatening conditions.” “Having a specialty-trained team of physicians, nurses, respiratory therapists, care managers, physical and occupational therapists around the clock, every day ensures that, no matter the illness or injury, a patient will be treated with the highest degree of care right away,” says Paul Sierzenski, MD, MSHQS, CPE, FACEP, Chief Medical Officer, Acute Services. “What it comes down to is this; the quicker and more accurately you get treated, the better your outcome will be. That's what makes being one of the most respected critical care teams in the country, so vital to all of us.” “At Renown, we have done so much over the years, to prepare to meet the need for rapid surges in critically ill or injured patients. Through this pandemic, many patients suffering from complications of COVID-19 have needed intensive care services,” says Erik Olson, MHA, Chief Executive Officer of Renown Regional Medical Center. “As the demand for critical care and intensive care continues to increase, the ratio of ICU beds to hospital beds will continue to rise as the ICU occupies an ever-larger role at the center of acute hospital care. We appreciate the recognition from Healthgrades demonstrating the Renown team’s unwavering commitment to the highest level of patient care and safety.” About Renown Health Renown Health is the region’s largest, locally owned and governed, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe, and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination, and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group, an urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health. Renown’s institute model addresses social determinants of health and includes Child Health, Behavioral Health & Addiction, Healthy Aging, and Health Innovation. Clinical institutes include Cancer, Heart, and Vascular Heath, Neurosciences, and Robotic Surgery. Renown is currently enrolling participants in the world’s largest community-based genetic population health study, the Healthy Nevada Project®. For more information, visit renown.org. About Healthgrades Healthgrades is dedicated to empowering stronger and more meaningful connections between patients and their healthcare providers. At Healthgrades, we help millions of consumers each month find and schedule appointments with their provider of choice. With our scheduling solutions and advanced analytics applications, we help our health system and life sciences clients cultivate new patient relationships, improve patient access, and build customer loyalty. At Healthgrades, better health gets a head start.
-
Renown Neuro Diagnostic Laboratory Nationally Recognized
Earning its third five-year accreditation, Renown’s neuro-diagnostic lab remains Nevada’s only accredited ABRET facility. The Renown Institute for Neurosciences is pleased to announce that the neuro-diagnostic lab at Renown Regional Medical Center has been re-accredited by the American Board of Registration of Electroencephalographic and Evoked Potential Technologists (ABRET). ABRET’s lab accreditation process evaluates technical standards, the quality of a laboratory’s output, and lab management. “Renown Health is a leader and a destination for health in treating neurological disorders and advancing innovations in neurology. The specialists at the Renown Institute for Neurosciences provide comprehensive brain, nerve and surgical support along with a full range of diagnostic and additional procedures and a disease-specific, patient-focused approach to care,” says Tony Slonim, MD, DrPH, FACHE, President and CEO, Renown Health. “This prestigious honor from ABRET means Renown’s Electroencephalogram (EEG) Laboratory has met strict standards and is recognized as a place where patients and physicians can confidently receive quality diagnostics.” “In addition to re-accreditation from ABRET, the Institute for Neurosciences has earned a Gold Seal of Approval by the Joint Commission and offers advanced treatment options including t-PA (Tissue Plasminogen Activator) and biplane angiography. The Level III accredited Epilepsy laboratory implements some of the newest treatments available,” said Renown’s Chief Medical Officer, Paul Sierzenski, MD, MSHQS, CPE, FACEP. “Renown patients also have access to the most promising new therapies through national clinical trials, which have been shown to significantly improve patients’ health and well-being.” “I am proud to recognize our dedicated team of caregivers for their continued passion and excellence in maintaining the highest standards in patient care,” said Renown Institute for Neurosciences’ Division Chief, Dr. Rolando Ania. “It is all thanks to their tremendous efforts that we remain the only ABRET accredited laboratory, as well as the only nationally accredited epilepsy center (NAEC Level III), in the state of Nevada.” Using a collaborative approach, specialists at the Renown Institute for Neurosciences use leading-edge diagnostic tools to identify neurological conditions and treat patients with the most effective techniques available. What is a Neuro-diagnostic Lab? A neuro-diagnostic lab allows care teams the technology to evaluate how a patient’s peripheral, autonomic, and central nervous systems function, and aid in diagnosing and treating conditions such as epilepsy, multiple sclerosis, Parkinson’s disease, stroke, and other diseases of the nervous system. What is an Electroencephalogram (EEG)? An Electroencephalogram (EEG) is a test that measures and records the electrical activity of the brain. During the test, special sensors called electrodes are attached to the patient’s head and hooked by wires to a computer. The computer then records the brain’s electrical activity on the screen. Using a collaborative approach, specialists at the Renown Institute for Neurosciences use leading-edge diagnostic tools to identify neurological conditions and treat patients with the most effective techniques available. Renown Health hospitals are ranked as Nevada’s top hospitals by U.S. News & World Report.
Read More About Renown Neuro Diagnostic Laboratory Nationally Recognized
-
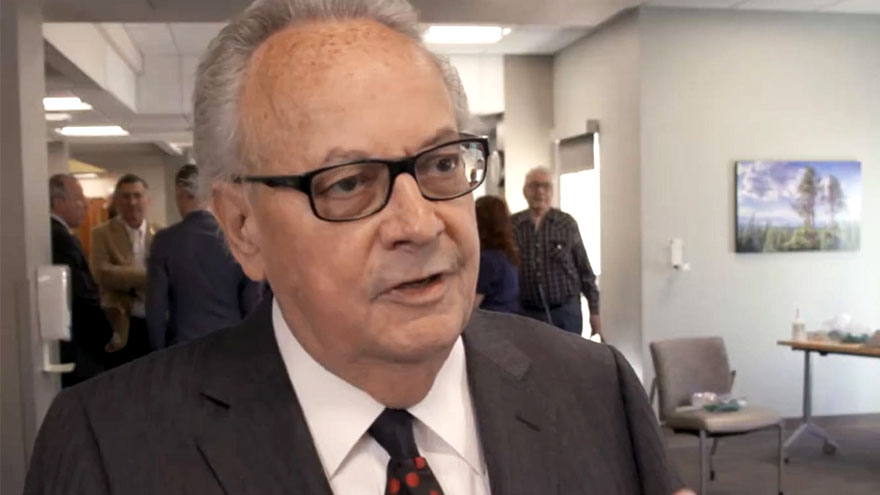
Thomas S Dolan Pulmonary Rehabilitation Program
The program becomes first of its kind to be accredited in Nevada Renown Health is pleased to announce the certification of the Thomas S. Dolan Pulmonary Rehabilitation program at Renown South Meadows Medical Center by the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). AACVPR certification demonstrates that an organization's Pulmonary Rehabilitation Program is aligned with current guidelines set by the American Association of Cardiovascular and Pulmonary Rehabilitation for appropriate and effective early outpatient care of patients with cardiac or pulmonary issues. Certification offers peace of mind, so that patients can feel confident in knowing that staff has the experience and skills necessary to coordinate the many issues faced by people receiving a life-changing cardiac or pulmonary diagnosis. Pulmonary rehabilitation programs help people with health issues such as asthma, chronic bronchitis, pulmonary fibrosis, or chronic obstructive pulmonary disease (COPD) recover faster and live healthier. “Having access to quality pulmonary rehabilitation services so close to home, staffed by a highly skilled group of compassionate care providers, truly is a gift to our community,” said Tony Slonim,MD, D.Ph., president and CEO of Renown. “We are extremely proud of the work being done in our pulmonary rehabilitation program, and also forever grateful for Tom Dolan’s donation to the program in 2019, which empowers Nevadans to improve both their health and quality of life.” “Thomas S. Dolan Pulmonary Rehabilitation is the only accredited pulmonary rehabilitation program in the state of Nevada,” said Renown South Meadows Medical Center and Rehabilitation Hospital Vice President Chris Nicholas. “We take pride in this distinguished honor from the AACVPR as it acknowledges and amplifies the life-changing work happening here. Our dedicated caregivers provide support to our patients every step of the way, helping them lead vibrant and fulfilling lives despite their health conditions.” The comprehensive pulmonary rehabilitation program at Renown South Meadows Medical Center offers treadmills, stationary bicycles, strength training and an education classroom to help patients achieve health goals. To earn accreditation, Renown’s pulmonary rehabilitation program participated in an application process requiring extensive documentation of the program’s practices. AACVPR Program Certification is the only peer-review accreditation process designed to review individual programs for adherence to standards and guidelines developed and published by AACVPR and other related professional societies. In November 2019, Tom Dolan, owner and founder of Dolan Auto Group, donated to the Pulmonary Rehabilitation at Renown South Meadows Medical Center after his personal experience thriving in pulmonary rehabilitation brought northern Nevada’s capabilities, and needs to his attention. His generous donation has allowed Renown to double the number of patients who receive treatment and increase the access to pulmonary rehab in our community. “As a former patient myself, I found so much benefit in my pulmonary rehab,” said Dolan. “I have always wanted to support this program and increase the number of people it serves. It’s great to see that we now have the only certified pulmonary rehab in Nevada. “The most essential component of lung health is breaking the cycle of inactivity associated with lung disease,” said Lung Critical Care Physician Dr. Farah Madhani-Lovely. “Our community is fortunate to have an accredited program like this to empower our patients.” About AACVPR Founded in 1985, the American Association of Cardiovascular and Pulmonary Rehabilitation is a multidisciplinary organization dedicated to the mission of reducing morbidity, mortality and disability from cardiovascular and pulmonary disease through education, prevention, rehabilitation, research and disease management. Central to the core mission is improving the quality of life for patients and their families. Learn more about AACVPR at www.aacvpr.org.
Read More About Thomas S Dolan Pulmonary Rehabilitation Program
-
South Meadows Medical Center Named Number 1 Hospital
U.S. News & World Report recently released their 2020-21 Best Hospitals rankings naming Renown South Meadows Medical Center as the number one hospital in Nevada. U.S. News looked at 4,554 hospitals, which represent nearly all U.S. facilities providing inpatient care. Hospitals are evaluated across a wide range of conditions and procedures, including 16 medical specialty areas of care. “We are committed to be among the best in the nation for quality, safety and patient experience,” said Tony Slonim, MD, D.Ph., FACHE, president and CEO of Renown. “This ranking confirms what Renown has always been dedicated to — providing the best patient care possible. Quality and safety are the responsibility of every employee and physician at Renown, and we are proud that Renown South Meadows has been chosen as the best in the state and among the best in the nation.” “We thank the incredible physicians, nurses and employees at Renown South Meadows Medical Center and across Renown for their dedication to excellent patient care – our employees, patients and our community are the true award winners,” said Chris Nicholas, Vice President & Administrator, Renown South Meadows & Renown Rehabilitation Hospital. “We applaud them as being not only the best in the state, but among the best in the nation.” “We are proud that Renown South Meadows is one of Nevada’s highest rated hospitals, and it’s exciting to have that recognition. Over the last year both our acute care hospitals – South Meadows and Renown Regional Medical Center, have made substantial improvements. We are working every day to ensure we are delivering the highest quality, safest care to our patients and our community,” said Dawn D. Ahner, DSc, FACHE, Chief Operating Officer — Acute Services for Renown. Renown South Meadows has been recognized by several national organizations for excellence and quality, including the Joint Commission, Leapfrog and Health Insight. Renown South Meadows Medical Center is an Accredited Chest Pain Center, and a Pathway Designated hospital for nursing excellence. Renown South Meadows provides an emergency department staffed 24/7 with board-certified emergency physicians, a wide range of services including primary and urgent care medical offices, a lab and health improvement programs. Renown is currently recruiting outstanding employees at https://careers.renown.org/.
Read More About South Meadows Medical Center Named Number 1 Hospital