Buscar
-
Why Childhood Immunizations Are So Important
Immunizations save thousands of lives each year by preventing serious illnesses, hospitalizations, and deaths. They also protect those who can't be vaccinated, like young children and the elderly, through herd immunity. Dr. Vanessa Slots highlights the crucial role of vaccines. Immunizations Your Child Needs (and when) Birth to 6 Months Hepatitis B: Shortly after birth, first vaccine dose Diphtheria, Tetanus, and Pertussis (DTaP), Polio, Haemophilus Influenza (HiB), Pneumonia, Hepatitis B and Rotavirus: Ages 2, 4 and 6 months, boosters and vaccines One Year to 18 Months MMR and Varicella (chickenpox) vaccine: Age 1, first vaccine dose Hepatitis A, HiB and Pneumonia: Age 1, booster DTaP: 15 months, fourth vaccine dose Hepatitis, second dose: 18 months Flu Vaccine: 6 months and older, annually* *In the year after receiving their first dose, an infant will need a booster one month later. Four Years Old MMRV, DTaP and Polio, final dose: Four years of age Pre-Teen and Beyond Tdap and Meningitis: Before starting middle school, children receive these vaccines. They are also old enough to start the HPV vaccine, an essential vaccine for all young adults to protect against cancer, genital warts and cervical dysplasia.
Read More About Why Childhood Immunizations Are So Important
-
What You Need to Know About RSV
Respiratory syncytial virus, also known as RSV, is a common respiratory virus that impacts the lungs and breathing pathways. The virus can be dangerous for infants and young children and is also concerning for older adults. While most older kids and adults only experience cold-like systems and recover in a week or two, an estimated 58,000-80,000 children younger than 5 years old are hospitalized due to RSV each year, and in 2022 healthcare organizations across the country are experiencing higher infection rates than in years past. "We are experiencing a strong RSV season and do not expect it to go away anytime soon," said Dr. Kris Wilson, Division Chief of Renown Children's Primary Care. "Infants who are infected with RSV almost always show symptoms of runny noses and cough. Call your healthcare provider immediately if your child is having difficulty breathing, is not drinking enough fluids, or is experiencing any worsening of these symptoms.” Symptoms of RSV: Runny nose Decrease in appetite/inability to drink Dry diapers, an indication of dehydration Cough, which may progress to wheezing or difficulty breathing Irritability (most common in very young infants) Decreased activity (most common in very young infants) Decreased appetite (most common in very young infants) Apnea, pauses in breathing for more than 10 seconds (most common in very young infants) What to do if you think your child has RSV: Call your pediatrician! If you suspect your child might have RSV, consulting their healthcare provider is the best first line of defense. From here they will help you build an appropriate treatment plan for child. Keep in mind that many pediatrician offices offer 24/7 call lines. If your child is experiencing retracted breathing (when the area between the ribs and in the neck sinks in when a person attempts to inhale), dehydration (not drinking and decrease in wet diapers) or apnea (pauses in breathing for more than 10 seconds) please call 911 or go to the closest emergency room.
-
Perfect Peanut Butter and Pumpkin Puppy Treats
This holiday season, sprinkle some extra joy for your favorite furry pals by whipping up these easy, AKC-approved dog treats. With simple ingredients and quick baking times, they're the perfect last-minute surprise to show your pet some love. Turn it into a delightful gift by snagging some adorable, budget-friendly canisters (easily found at dollar or thrift stores) and fill them to the brim with these homemade goodies. It's a merry, tail-wagging gift that's sure to make this season the most pet-friendly one yet! 🎄🐾🍪
Read More About Perfect Peanut Butter and Pumpkin Puppy Treats
-
6 Healthcare Action Items for the LGBTQIA+ Community
© Niyazz via Canva.com Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
Departamento destacado: Renown Transfer and Operations Center
Stepping into the Renown Transfer and Operations Center (RTOC) means stepping into a transformative hub of excellence where lives are saved and healthcare is reimagined. As a cornerstone of Renown Health's commitment to exceptional patient care, the RTOC serves as a dynamic nerve center that seamlessly coordinates medical resources, ambulance rides, hospital bed space, remote home systems, hospital transfers and emergency preparedness. In this best-in-class facility, the boundaries of what is possible in healthcare are constantly pushed, and new horizons of patient care are discovered. Staffed with a dedicated team of skilled professionals, the RTOC harnesses the power of advanced technology and compassionate expertise to ensure that patients receive the highest level of care and support, no matter where they are. Through a synchronized network of communication, coordination, and compassionate care, the RTOC team ensures that patients receive the critical support they need when it matters most, working tirelessly to redefine what it means to deliver world-class healthcare. A National Standard Charged with the goal of overseeing the placement and transportation for every patient, the RTOC officially launched in 2021 as northern Nevada’s first and only transfer center of its kind and a nationally celebrated facility. As Renown’s highly coordinated care logistics system, this team uses the cutting-edge technology at their fingertips to customize healthcare to the needs of every patient, manage patient flow and drive healthcare innovation. “Compared to where we’ve started to where we are now, it’s a 180-degree difference,” said Kelli McDonnell, Manager of RTOC. “When we first started building our facility right before the pandemic happened, we took what was six conference rooms and classrooms and turned it into a command center that organizations across the country admire and come to Reno to see what we do. Mel Morris, the Director of RTOC, was recruited exclusively to build our facility with her history of building successful hospital command centers. Many people didn’t realize what a transfer center was or that Renown was the only center in the region – and we only continue to grow.” This best-in-class facility, and the masterful team behind it, handles: Coordinating all incoming patients transferred from neighboring hospitals and 27 counties across northern Nevada, Lake Tahoe, northeast California and neighboring states. Matching patients to the most appropriate bed placement using diagnostic, triage and Epic electronic medical record clinical information in conjunction with medical staff expertise to outline a plan of care that determines the best bed assignment given the patient’s needs. Coordinating video-enabled Telehealth monitoring capabilities for Renown’s four Intensive Care Units (ICUs), as well as Renown patient Telehealth and virtual visits. Monitoring Remote Home systems with Masimo during the COVID-19 pandemic, where some patients received hospital-level care in the comfort of their own homes while Renown clinicians monitored and evaluated their data and plan of care. Serving emergency and disaster management for area hospitals, first-responders and the community with local, regional and statewide emergency and disaster management for sudden-onset emergencies. The RTOC is home to many different critical roles for our health system, including Transfer Center Nurses, Ride Line Coordinators, RTOC Coordinators and more, many duties of which each team member cross-trains on to be able to fill in whenever needed. While their roles may differ, their commitment to their patients remains the same – and they all work together to achieve the same outcome: delivering the right care, at the right time and place. “As an RTOC Coordinator, we do a variety of different things,” said Anna Schaffer, RTOC Coordinator. “We do triage coordination to help our nurses and hospitalists get patients in the emergency department admitted, and we also do bed control to find patients appropriate bed placement. Communication is important, so we always make sure to stay closely connected with the charge nurses on those floors.” “We start with a basic ‘need to know’ and place patients accordingly,” added Karly Brown, RTOC Coordinator. “We get surgery numbers, ICU capacity and discharges and find beds for all patients as quickly as possible. We have the advantage of being able to see the entire hospital.” “I primarily schedule transportation for patients at the hospital who are either going home or going to a skilled nursing facility,” said Sarah Clark, Ride Line Coordinator. “I get requests from case managers to schedule rides, and I work with REMSA and other ambulance services to schedule them. It relies a lot on appropriate and efficient communication and critical thinking.” Patients in facilities across northern Nevada and northeastern California, especially the rural communities, look to the RTOC to help guide ambulances, bed coordinators and hospital staff in finding care for our rural patients. “As a transfer center nurse, I facilitate incoming patients from rural facilities in Nevada and surrounding areas in California,” added Meg Myles, Transfer Center Nurse Specialist. “There are days we may take up to 30 direct admissions from these areas.” “We are the point of contact for inter-facility transfers, whether we are sending patients out or bringing them into Renown,” said Lisa Lac, Transfer Center Nurse Specialist. “We take phone calls from those rural areas, identify what services are needed, connect them to the appropriate provider and coordinate any transfers.” “Simply put, we are the bed wizards,” said Addison Rittenhouse, RTOC Coordinator. The RTOC team continues to break barriers and push the boundaries of medical excellence through leveraging the technology at their fingertips and their unwavering dedication to the health of our community. Inspiring a new era of medical possibilities, these team members have achieved a multitude of accomplishments for both their department and their patients since the birth of the center. “We have significantly reduced the time it takes to get patient admit orders in, thanks in part to the new Triage Coordinator role, and we provide easier access for patients to transfer to us from other facilities,” said Beth Rios, RTOC Coordinator. “We have taken a bigger role in helping the smaller hospitals in our area in caring for patients and improve patient throughput.” “As a team, we’ve done a lot of work in creating an engaging and positive environment, and our internal morale committee has been a huge help with that,” said Kelli McDonnell. “We’ve been working tremendously over the last year and taking all the feedback that we received from the Employee Engagement Survey to make improvements. We had 100 percent survey participation within five days, which is incredible.” “I am so proud of our escalation and problem-solving skills,” said Becca Dietrich, RTOC Coordinator. “When an issue is raised to us, we will always find a timely solution on our end so our care teams can focus on the issue in front of them. We are the eyes in the sky, seeing movement everywhere.” Each day in the life of our RTOC team members is a testament to their commitment, resilience and timework, making a profound impact on countless lives.
Read More About Department Spotlight: Renown Transfer and Operations Center
-
Department Spotlight Clinical Research
May 20 is National Clinical Trials Day. Celebrate with us by recognizing the Clinical Research team at Renown Health! The root of every medication, treatment and procedure in healthcare can be traced back to research. From the beginning of the history of medicine, research has always played a crucial role in improving the lives of patients around the world, leaving a permanent mark on how we expand our medical capabilities to this day. Renown Health’s Clinical Research team, in partnership with the University of Nevada, Reno School of Medicine (UNR Med), are leading that effort in our very own community. As our in-house leaders of clinical trials, this team is dedicated to advancing the science of medicine to help further our bottom line of making a genuine difference in the health and well-being of the patients they serve. Trial by (Medical) Jury Every day looks different for the Clinical Research team, especially when it comes to interacting with patients, providers and “sponsors,” which are the organizations providing the treatment for the study. One fact always remains true: communication and collaboration are key, especially among the team who act as the face of this process. Meet Lisa English (pictured above on the far right in a blue shirt), a Lead Clinical Research Coordinator at Renown who serves as the study "project manager." One aspect of Lisa’s day-to-day is seeing patients through their clinical trials from start to finish. It all begins with the setup. “Before we can launch a study, there is a lot of back-and-forth dialogue between everyone involved to ensure the best fit,” said Lisa. “Sponsors will come to us with novel treatments, such as medications or devices, and the inclusion criteria that patients need to meet in order to qualify for the study. We then immediately jump into working with the providers, looking closely at the science and comparing the treatments to what is on the market already.” From there, Lisa coordinates conversations between the providers, sponsors and study teams to gauge everyone’s capacity based on the length of the study, ensuring everyone involved has the time to dedicate to the process. Next, the providers identify patients that meet the criteria for the study, and together, the team decides where the patient visits will happen and discusses any potential barriers that may affect patient retention. The budget is clearly defined at this stage, set up to make sure no patient is ever billed for medical costs incurred as a result of the study. Often, research participants are seen within the specialty clinics throughout the health system, while other times the Clinical Research Coordinators see patients at the recently centralized Clinical Research Office at Renown Regional Medical Center. This location provides an essential public-facing space for the community to learn more about clinical trials and demonstrates the breadth of resources available at Renown to sponsors to strengthen external partnerships and research funding opportunities. Once the study officially begins, team members like Lisa will set patients up for a “screening/qualifying visit.” During this appointment, she makes sure patients get scheduled for their lab work, imaging scans and anything else the provider may need to make an executive decision on whether or not the patient is a good candidate for the study. “I build it all in Epic,” said Lisa. “The study information, directions, requirements and next steps are all loaded in Epic for easy tracking. We are also required to input any notes in the sponsor’s electronic data capture website. All the information I track is inputted without protected health information (PHI), so every patient is completely anonymous.” After the patient officially qualifies, the study goes full steam ahead. Team members like Lisa and the providers receive continual updates from sponsors on the status of the study. “Throughout the entire process, I make sure patients get scheduled for everything that meets the requirements for the study,” said Lisa. “I meet with patients one-on-one to discuss their needs and concerns and ask questions about the study, organize their appointments and charts and deal with any issues or pivots that may arise. It’s very important that every patient fully understands what is going to happen with their care.” The Clinical Research department strives to serve as a care partner to patients, providers and clinics they work with. The majority of our Clinical Research Coordinators are trained phlebotomists and medical assistants, performing their own assessments such as lab draws and electrocardiograms (ECGs) to streamline the research visit process and reduce resource constraints on the clinics and health system. Lisa typically sees a couple of patients per week, depending on the study and where patients are in the cycle. Depending on the complexity of the trial, patients may see the research team only one time or several times over many years. Typically, clinical trial patients are seen in clinic every 2-4 weeks. There are many tasks required before, during and after a research visit to ensure everything runs smoothly, so Clinical Research Coordinators dedicate an average of 5-11 hours of work per patient, per visit. Regardless of patient load, each employee in the Clinical Research department – as well as participating teams across Renown and UNR Med – always step in to help each other out. According to Lisa, the environment is immensely supportive. “We have a program here at Renown to train employees who have never done clinical trials,” said Lisa. “We love seeing people get more engaged with the important work we do, and every department has been great at collaborating with us. Everyone brings a different perspective.” At the end of the study, Lisa gathers all the information and collects notes into a zip drive or paper binder for archiving. The sponsor lets the Clinical Research team, providers and patients know whether they are on the trial drug or on the placebo. The teams use the data gathered during the study to publish a report or present at conferences, promoting the critical research done to better the lives of patients in our community, and potentially, the world. “I appreciate the time everyone gives us to make sure our research is successful,” said Lisa. “It feels great to work together to make a difference, improve healthcare quality and save lives.” Behind-the-Scenes, Yet on the Frontlines The impact of research studies transcends hospital walls, and this can all be attributed to the dedication of our Clinical Research department. The constant collaboration between this team, lab science, medical assistants and providers, cardiology technologists, sonographers, finance teams and our partners at UNR Med is crucial to safeguarding the success of the studies. Devoted to keeping research close to home, Renown and UNR Med teamed up to form the Clinical Research Office (CRO) in 2021. With the strength of northern Nevada's largest not-for-profit health system and Nevada’s first medical school, this team is dedicated to giving our community access to the latest care innovations. “At UNR Med, we are working with students, residents and academic faculty; on the Renown side, we are working with clinicians and community participants,” said Amber Emerson, Manager for Community Outreach and Research Engagement for UNR Med. “Everything we do is data-driven,” added Kristen Gurnea, Manager of Clinical Research for Renown. “Our main goal is to optimize our impact and provide a community benefit for our patients. The scope of our roles in the Clinical Research office is very diverse.” To help meet the growing need locally for healthcare and cutting-edge treatment solutions, the CRO has continued to grow, expanding its research capabilities and helping bring new medications, medical devices and more to patients across northern Nevada and northeastern California. “Once upon a time, our team had only six members; today we have grown to a team of 25,” added Diana Torres, Research Resource Analyst for Renown. “We used to be considered one department, including Medical Education, and we have since branched off into our own cost center. We branched off even further and created a separate Genetics department that runs the Healthy Nevada Project. Throughout this process, the Clinical Research department was always the main point of the umbrella.” “We participate in hospital-wide outreach and marketing, and we feel this has really helped us get the word out about our department,” added Raul Arellano, Research Resource Analyst for Renown. “In fact, we doubled our clinical trial portfolio from last year.” The CRO currently operates over 100 clinical trials locally in cardiology, endocrinology, infectious disease, neurology, pediatric and adult oncology, pediatric sub-specialties and pulmonology. Behind the curtains of in-person research, the CRO is home to several experts who help turn our research studies into a reality, from budgeting and billing to barrier-breaking and building relationships. “I help with barriers patients and Clinical Research Coordinators are facing, building connections and relationships inside and outside of our health system,” said Kristen Gurnea. “I enjoy handling all the supporting pieces that are required for studies to happen.” “My role changes every day,” added Jenna Berger, Administrative Assistant for the CRO at Renown. “Some days, I’ll be helping coordinate patient stipends and going through document management to ensure we have all necessary signatures. Other days, I will be planning events – like Clinical Trials Week – for our department and creating marketing materials and fliers.” “Our day-to-day involves going over anything related to research financials,” added Diana Torres. “We handle sponsor billings, process efficiency and collecting revenue for research contracts, and we collaborate closely with our Finance department and Revenue Integrity in order to accomplish this. It’s important for us to make sure all billing on both the sponsor and patient side is taken care of, especially because patients should never receive a bill for medical services they receive for the trial. A year and a half ago, we started doing budget negotiations for research contracts,” said Diana Torres. “We are proud to help clinical teams with any training they may need on these negotiations as well as billing reviews and allocations.” Seeing patients progress during a study and transform before their eyes inspires the CRO team to continue doing what they do every day. “I’ve been here for many years, first working on the floor as an oncology nurse and transitioning to oncology research in 2005,” said Anna Winchell, Cancer Protocol Nurse for Renown. “I love getting to know the patients and seeing them progress into a healthy lifestyle.” Medical students and residents at UNR Med also play a significant role in the research process, advancing medicine by exploring causes and novel treatments for a wide range of conditions, including HIV, muscular dystrophy, gastrointestinal disorders, infectious diseases and more. Medical research at UNR Med is headed by committed research coordinators, community outreach managers, grants managers, pharmacists and physicians. “I oversee scientific review and help the physicians that come to us for those resources,” said Amil Trujillo-King, Medical Research Coordinator at UNR Med. “I guide medical students in their research protocols and help with different projects to improve research activities for both students and medical residents.” It takes a village to make clinical research happen. Because of that, the ACRO cannot thank the following teams enough for moving mountains for the future of medicine: Renown Health and UNR Med leadership for demonstrating the integrated health system’s commitment to expanding access to clinical research in our community within both the Renown / UNR Med affiliation and Renown active strategic plans. Renown Pharmacy especially Research Clinical Pharmacist Tim Morton, who supports all clinical trial medication dispensing and patient education across all clinical trials at Renown. Accounts Payable for having a huge impact on patient and employee reimbursement. Renown Medical Group for their participating providers, especially in oncology, cardiology, pulmonology, pediatrics, endocrinology and neurology, who are involved in research year after year. Marketing and Communications for helping with printed materials and raising awareness for clinical research at Renown and UNR Med. An Affiliation to Last Through the Ages A collective, shared vision of exploring community health – that is the impetus behind the affiliation between Renown and UNR Med. By leveraging resources across both institutions, the CRO has maximized their impact, giving the people of northern Nevada greater access to new interventions and treatments and promoting an impassioned culture with patients, providers, residents and medical students. “Community-based research always sat well with me,” said Amber Emerson. “As Renown and UNR Med, we have this unique opportunity to shape clinical research here in northern Nevada. We always make sure we present research in a meaningful way that speaks to the work we produce and demonstrates the opportunities we offer. After all, participating in clinical research doesn’t mean our patients are ‘guinea pigs’ – quite the opposite! They are partners in their health care, and we support them through providing access to novel treatments.” “Research is my passion, and my career has spanned broadly from grants administration to study coordination,” added Valerie Smith, Clinical Research Center Administrative Manager at UNR Med. “I am excited to be at the forefront of research frontiers in northern Nevada.” Through robust engagement and collaboration with healthcare providers, department administrators, internal research team members and leadership, the strength of this affiliation is unmeasurable. The CRO’s ultimate goal is to have clinical trials be the standard of care for every condition that Renown and UNR Med treats. Clinical research participation is all about patient autonomy, shared decision-making between patients and their providers and advancing medicine to save lives. From their beginnings as a small group of passionate researchers to their present reality as a leader in the research space in northern Nevada, their efforts do not go unnoticed. “The success of our department is inspiring,” said Amil Trujillo-King. “Renown and UNR Med supports the wellbeing of all employees and contributes directly to the growth of the department.” “When I first joined Renown in Patient Access, I didn’t realize that we had a research department; with a strong healthcare background in my family, I knew I wanted to grow in my career, and our expanding Clinical Research office was that next step,” said Raul Arellano. “With our affiliation with UNR Med, it’s especially inspiring to be able to apply what I learned as a Patient Access Representative to help further outcomes for our patients through managing our finances.” Through their unwavering commitment to research excellence and patient-centered care, the CRO will continue to pave the way for groundbreaking medical discoveries and improved outcomes for patients for years to come. “Fundamentally, we’re working to build a culture of research in our community because we believe it is the right thing to do. Our community deserves to have access to clinical trials and novel care close to home with a dedicated team to support them every step of the way,” closes Kristen Gurnea.
-
Meet Raven: A Renown Therapy Dog
If you’ve ever spent time at Renown, you may have noticed there are some four-legged volunteers roaming the halls greeting patients, visitors, and staff. Since 1997, Renown has been fortunate enough to have its very own therapy dog program. As of today, there are 43 dogs in the program, and each of them have gone through countless hours of training to offer healing, comfort and support to those seeking treatment within our health system. Each of these therapy dogs have their own special personalities, but they all share the same mission: to make a paws-itive impact on everyone they meet. One therapy dog that has touched many lives at Renown is Raven, a five-year old Belgian Malinois mix. Raven's Story In March of 2019, Reno residents Richard and Vickie Lange rescued Raven from an animal shelter in Portola, California. When the Langes made Raven part of their family, they immediately started her in obedience training. After seeing her do so well, they thought of an idea that would not only help Raven reach her full potential but also allow them to give back to others – they decided to train Raven to be a therapy dog.
-
A Renown Anesthesiologist's Unique Journey
Dr. Nariman Rahimzadeh’s career path has been anything but typical. From humble beginnings as a shuttle bus driver for Renown Regional Medical Center, then named Washoe Medical Center, to his service as Chief of Staff for Renown South Meadows Medical Center, the steps and detours he took along the way – and the strong support from his colleagues and family members – make up a tale of perseverance, conviction, compassion and inspiration. However, his healthcare career journey began several years before he even joined Washoe Medical Center in the 1990s. It all began 7,446 miles away in Iran. This is Dr. Rahimzadeh’s story. Defining Moments The moment Dr. Rahimzadeh knew he wanted to dedicate his career to the healthcare field started during his childhood. Growing up in Iran during the midst of the Iranian Revolution, a thought that often came to mind was, “Who is helping all the people injured in the war?” The answer? The doctors. “In Iranian society, doctors are extremely valued, as they are the first to help people in need,” said Dr. Rahimzadeh. “I knew I wanted to give back to society in some way, and I see my time in Iran as very formative in my future career. I just didn’t know it yet.” After immigrating to the U.S. with his family during his preteen years, he only had one mission: to support his family. “My desires were to help my family not fall behind,” he said. “I didn’t have career aspirations at the time. All I knew is that I wanted to help my family and my community, which immediately opened its arms up to us, as well as be a good student and a good ambassador for Iran.” Dr. Rahimzadeh remembers several influential people that helped solidify his aspiration from “helping people” to “helping people as a healthcare professional.” Their family physician and other medical professionals in the family’s lives were monumental in helping him make this decision. Coupled with his natural love for the sciences, the decision to become a doctor became clear. But the question remained, “How do I get started in the healthcare field?” No Links to Healthcare? No Problem With no physicians in his immediate family and no direct connections to healthcare, Dr. Rahimzadeh set off to follow the advice he received from the influential people in his life: get a job at a healthcare facility, regardless of what the job title is. Some of his friends had recently joined Washoe Medical Center as patient transporters and mentioned job openings that were available. He sprang into action and headed to Washoe Medical Center to apply. Just one problem – he didn’t have the EMT certification requirement. Enter Barry O’Sullivan, who would be Dr. Rahimzadeh’s first supervisor at Washoe Medical Center (and a friend he still speaks with to this day). Barry saw promise in Dr. Rahimzadeh immediately. As a result, Barry made a suggestion to him that would ultimately set him on the course towards medicine. “Barry told me that he had an open position that I could work while completing the senior year of my undergraduate degree and studying for my EMT certification and eventually becoming a patient transporter. He told me Washoe Medical Center would support me in this endeavor. So, I asked what the job was and learned it was driving a shuttle bus.” Without hesitation, Dr. Rahimzadeh responded, “I’ll take it.” And so, his fulfilling journey with Washoe Medical Center, and eventually Renown Health, began. While he finished up the last few months of his degree at the University of Nevada, Reno, (UNR) Dr. Rahimzadeh proudly drove the shuttle bus a few days a week. The job not only helped him pay for his degree and put food on the table, but it also allowed him to begin living out his passion for helping people in the healthcare field. Dr. Rahimzadeh graduated with his bachelor's degree in Pre-Medicine from UNR and finished his EMT certification program. Sure enough, Barry and Washoe Medical Center lived up to their promises and helped him secure his first direct healthcare job as an EMT and Patient Transporter with REMSA. But he didn’t stop there – after several years as a ground transporter, his career literally took flight. He joined REMSA Ground Ambulance and eventually Care Flight as a Flight EMT II, caring for patients that were flying to Washoe Medical Center from nearby communities that needed lifesaving medical care. Helping save lives every day as a member of the emergency medical team is an ultimate feat, especially when it comes to Dr. Rahimzadeh. And he didn’t stop there. Valuing One-on-One Connections In the 1990s, as it is today, the U.S. experienced a significant primary care provider shortage which resulted in many medical schools encouraging students to complete their residencies in a primary care specialty, like internal medicine – which is precisely what Dr. Rahimzadeh set out to do at the University of Connecticut. However, his mind would soon change about the course of his career. “I had a deep, introspective conversation with my residency program director, openly and honestly chatting about my future,” Dr. Rahimzadeh said. “I ended up taking a week off of my residency and wrote a long pros and cons list about what I wanted to do with my life in the medical field.” Eventually he decided on anesthesiology because of the opportunity to have a one-on-one relationship with every surgery patient, regardless of their procedure. “Even though it’s for a short duration of time, it is a very impactful relationship,” he said. “I feel I am making a difference in the outcomes and lives of patients every day.” Dr. Rahimzadeh finished his internal medicine residency in three years and passed his board exam, and he went on to do the same thing for anesthesiology. He then ventured back home to Reno. Career Progression at Its Finest Dr. Rahimzadeh knows that people don’t always get to settle down in a place that influenced their upbringing, care and dream, yet he was able to make that vision a reality for himself. “I feel like Renown Health and myself have this intertwined relationship that led to my growth as a person and as a physician,” he said. “For that, I feel very blessed." Upon his arrival back to Reno with two residencies under his belt, Dr. Rahimzadeh was quickly hired at one of the two anesthesiology groups in town at the time. He started his career with Sierra Anesthesia and after working for the group for several years, he joined Associated Anesthesiologists of Reno in 2014, which went on to become one of the largest anesthesiology groups in northern Nevada. The group continuously worked very closely with Renown, taking care of all of its surgical patient needs and eventually becoming Renown Medical Group employees as of April 1, 2022, with Dr. Rahimzadeh setting up his home base at the Renown South Meadows campus. Today, Dr. Rahimzadeh wears three “hats” at Renown. As a medical professional first and foremost, his largest “hat” is his general anesthesiologist role, where he cares for patients in the operating room. Another significant “hat” is his role as the Medical Director for Surgical Services, where he reviews surgical patient charges alongside his dedicated team of nurses and ensures optimal patient outcomes by verifying they have had the appropriate workup to proceed with surgery in a safe manner. To round out his immense responsibilities with Renown, he serves as Chief of Staff for Renown South Meadows, where he makes connections with colleagues and collaborates with leaders to review protocols, policies and address concerns that arise. Outside of Renown, Dr. Rahimzadeh is still a contributor within his own anesthesiology practice. He also is the current President of the Nevada State Society of Anesthesiologists and the Director to the Board of Directors of the American Society of Anesthesiologists, helping bridge the gap in anesthesia concerns between his northern and southern Nevada colleagues. He reflects on the opportunities Renown and our local community have extended to him by saying, “If you can dream big enough and continue to chase your dreams, you can make it happen right here.” On the COVID-19 Frontlines Nothing could prepare us for the dire situation hospitals on the east coast – especially those in Livingston, New Jersey – were experiencing at the beginning of the pandemic. Livingston was known as the “second hardest hit area” by COVID-19 in April of 2020. Hospitals were overwhelmed with patients in the ICU fighting for their lives. They needed help, and they needed help now. Unable and unwilling to sit idly by, Dr. Rahimzadeh and six of his colleagues from his practice traveled to Livingston to help. They jumped in on the frontlines alongside other anesthesiologists and intensivists to offset the sudden influx of COVID-19 patients. Many lives were saved, and Dr. Rahimzadeh was a direct part of that. “When you care and work with people that also care, you can move the needle a lot – it doesn’t matter where you're from,” he said. Home Means Nevada – and Renown Renown Health is deeply rooted in the northern Nevada community. Dr. Rahimzadeh is proud to be among a diverse team who have taken responsibility for its community for generations. "We live in a very passionate and caring community, which is often underestimated,” he said. “It’s clear to me that Renown refuses to settle. Renown is incredibly progressive in providing the best for the community. We never remain stagnant, we keep moving forward and we take care of your loved ones. This health system has never been able to sit still and settle for the status quo. That stands out to me.” One story especially sticks out to Dr. Rahimzadeh as the moment when he knew that Renown was home. In 1997 while working as a patient transporter, his grandmother passed away on the sixth floor of the Sierra Tower at what is now Renown Regional Medical Center. At the funeral, a huge bouquet of flowers arrived. Not being especially close to anyone in Reno yet, Dr. Rahimzadeh's family had no idea who sent the beautiful arrangement. Turns out, it was Rod Callahan, the Chief Operating Officer (COO) of Washoe Medical Center at the time. “At that point, I knew I wasn’t just a part of a workforce with thousands of employees,” said Dr. Rahimzadeh. “The COO cared so much about me that he felt compelled to send such a wonderful gift during a tragic time. That’s the value of a local, community-focused hospital; the people here know you and care about you. There’s a reason why people stay at Renown for so long – we feel that connection.” Dr. Rahimzadeh also reflected on how far Renown South Meadows has come, from the time he immigrated to the U.S. to today. “Growing up, Renown South Meadows was kind of a ‘mom and pop shop’ primarily serving senior citizens in one wing and surgical patients in the other,” he said. “Now, I am so proud to see how far it has come. It really made its niche in the community in a great way. The future is bright!” It’s clear that Dr. Rahimzadeh is leaving a lasting legacy with his family, from the local community to global medicine. His son is a senior at Baylor University in Texas with a strong desire to go into medicine, just like his dad. His daughter is a junior at Bishop Manogue Catholic High School in Reno and enjoys being involved in her community. His loving wife is a speech therapist in the area. The Rahimzadeh family is thriving together, and they all share the same conviction about northern Nevada and Renown: “This is home.”
-
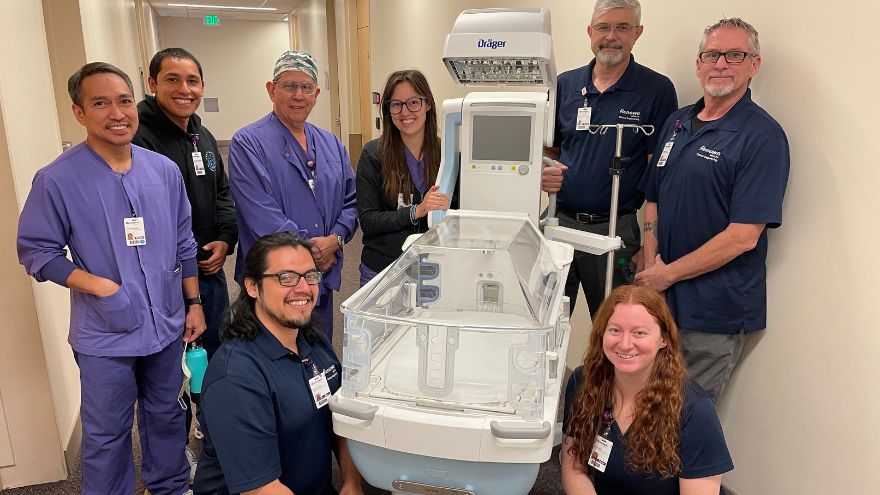
Departamento destacado: Clinical Engineering
Renown Health strongly supports and advocates for innovative medical technology. Our diverse lineup of medical equipment enables our care leaders to provide quality care to every patient. But what if a piece of technology breaks down? What happens when our care teams are ready for technological upgrades? Where do employees go when they have a question about a complicated piece of equipment? Enter the Clinical Engineering department. This sophisticated team is staffed with intelligent, science-minded individuals who are ready to jump in and help at any given second. From newborn incubators to robots that clean the hospital floors, these team members are the med-tech masters that keep our health system running. Equipment Experts Upon entering the Clinical Engineering department’s workshop, you are welcomed with an abundance of high-tech equipment undergoing repairs and upgrades. The department takes care of more than 26,000 pieces of equipment throughout the entire healthcare network, including the technologies at the University of Nevada, Reno School of Medicine, which they just took over this past year. To the average person, this may seem overwhelming; however, for this team, this is the exact environment they thrive in to make the technology magic happen. “I am motivated and engaged every day at work,” said Tony Martinez, Supervisor of Clinical Engineering for Renown. “Our department is fast-paced and rewarding, and that’s a big plus.” While some team members enter the department as equipment generalists, this team offers training to develop their skills on certain pieces of equipment, eventually becoming specialists. “Every month, we encourage our colleagues to undergo specific training on more delicate equipment,” said Tony. “Once we get to that point in their training, we assign different equipment to our team members every month. They pick up the experience very quickly.” As a Clinical Engineering Technician for Renown, Rylie Nickerson took advantage of the training and educational opportunities offered to her and is now a ventilator specialist especially for Renown’s neonatal intensive care unit (NICU). “Regardless of whether I’m working on ventilators or on another piece of equipment I’m assigned to, I’m always thinking about how I can help the patients, nurses and doctors,” said Rylie. Raul Hernandez, a Clinical Engineering Specialist for Renown, is the go-to person for anesthesia, heart-lung bypass, red cell saver and life support equipment. He embraces the fact that, regardless of whether you are a specialist or a generalist, there is no typical day working in this department. “Every day brings different challenges,” said Raul. “I really enjoy the mental exercises I do every day. They keep me grounded and focused.” On top of their day-to-day work and any special projects or emergencies that come up, the team is on an ongoing preventative maintenance schedule. Think of this work like your car’s oil change – routine maintenance to prevent something from breaking down in the future. “At any point, we might have 100-200 extra pieces of equipment to handle during preventative maintenance,” said Taylor Gray, a Clinical Engineering Technician for Renown. “We are always helping each other through any issues.” Our Clinical Engineering team shows exactly what it means to be collaborative. Even though their to-do lists are ever-growing, this team never feels alone. They know they can always lean on each other for support, regardless of the workload. “We always have each other’s backs,” said Taylor. “I feel so happy and satisfied in my job, and my coworkers are a large part of that.” Celebrating the Genuine Difference The Clinical Engineering department is driven by their desire to help and take care of the entire health system, and in turn, make a genuine difference for the communities we serve, from the medical staff to the patients. “The satisfaction you get in our field when we impact patients’ lives and their healing process is so motivating and engaging,” said Tony Martinez. “It’s a great feeling.” The team knows the common saying ‘Walk a mile in someone’s shoes’ very well; so well, in fact, that they take it to the next level, doing everything they can to prevent frustrations and extended down times. “We try to walk a mile in someone’s shoes before they get angry,” said Reagan Jordan, Director of Clinical Engineering for Renown. “Your satisfaction is our mission, and our team continually works to improve their outcomes every day.” This department is where the entrepreneurial spirit and science-focused mind meet. For people like Raul Hernandez, who came from a business background as well as decades of medical technology experience, Renown helps him bring both his personal and business skills into focus. “This environment is very beneficial for Renown, me, and of course, the patients,” added Raul. Being members of a team that is committed to excellence and purpose inspires them to reach new heights in patient care. “I am constantly reminded of the positive impact we have by witnessing the individual experiences we have and hearing the enthusiasm and thankfulness in their voices,” said Raul. “It gives me a great sense of pride to work at Renown.” "There is a strong feeling of mutual respect here,” added Ed Trejo, a Clinical Engineering Technician at Renown. “We are always here to help.” The proof is in the data. The Clinical Engineering team scored as one of the top departments in the recent Renown employee engagement survey, with their results sitting at more than 94 percent. “This speaks to not only our department leadership but also the team as a whole,” said Reagan. “I am extremely proud of them. Despite the pandemic, they are knocking it out of the park.” For this department, coming to Renown is easy; staying at Renown is even easier. “Staying at Renown is the easy choice,” said Raul. “And this team is only going to grow.” Workflow Whizzes and Kindness Champions “Rolling with the punches,” as Tony Martinez says, comes naturally to the Clinical Engineering team. With the constant workflow of equipment coming into the shop, every team member has learned how to be experts at prioritizing, especially based on the needs of our organization. Even though their jobs can bring a lot of intensity, this department’s positive attitude radiates throughout the hospital. Upon entering the workshop, everyone is greeted with a smile from every team member, along with an immediate willingness to dive into the complex world of engineering. “The experience of helping other people with their unique needs is invaluable,” said Taylor Gray. If this work environment sounds enticing, great news – the Clinical Engineering team is growing. Motivated, aspiring engineers with a passion for healthcare and an associate’s degree in a related field are welcome. Military experience is also valued very highly in this team. As many of our military servicemen and servicewomen gain specialized engineering experience while enlisted, the military-to-engineer career ladder at Renown is especially strong. In fact, according to Paul Joseph, a Clinical Engineering Technician at Renown, the majority of their teammates come from a military background. Above all, being capable of prioritizing on the fly, thinking critically, having an open-mined outlook and being self-driven are the top skills that this department values. As Ed Trejo states, “If you’re willing to wear different hats, you will do very well here." “Go with the flow, and expect the unexpected,” added Rylie Nickerson. Those who join this team feel at home. The warm embrace of the team’s kind nature and the supportive environment they all foster inspires an efficient workflow that helps our entire hospital system function at the top of its game. At the end of the day, everyone who joins the team, or anyone who even interacts with the team in any capacity, will be in good hands. Mandy Noriega, a Clinical Engineering Technician for Renown, closes these thoughts with a great reminder to each and every one of us: “After all, teamwork makes the dream work.”
-
Prevention Against STIs Matters
According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new sexually transmitted infection (STI) cases in the United States each year, with rates continuing to increase. What you may not know is most STIs are preventable. We talked with Renown Adolescent Medicine Specialist, Caroline Barangan, MD to learn more about STIs. How Can You Get an STI? The CDC (Center for Disease Control) says that STIs are acquired through sexual contact. There are bacteria, viruses or parasites that can cause an STI which may pass from person to person in blood, semen, vaginal and other bodily fluids. How Do You Know if You Have an STI? STIs can have a range of signs and symptoms such as: Warts, bumps or sores on or near the penis, vagina, mouth or anus Swelling, redness or severe itching near the penis or vagina Discharge from the penis Vaginal bleeding that’s not your period Painful or uncomfortable sex Vaginal discharge that has an unpleasant odor, causes irritation or is a different color or amount than usual Weight loss, diarrhea or night sweats Aches, pains, fever and chills Jaundice (yellowing of the skin and whites of the eyes) Painful or frequent urination Sore throat if you engage in oral sex It’s important to know that the majority of people who have an STI commonly have no symptoms at all, which is why it’s important to get regularly tested once you have had any sexual activity. Young people less than 25 years of age should be screened on a yearly basis at minimum.
-
La seguridad en las residencias universitarias y la meningitis bacteriana
Bacterial meningitis is probably the last thing on your mind as you help your child prepare for college. Buying books and stocking up on necessities may top your list, but it’s a good idea to ensure your student is up-to-date on their meningitis vaccine. How Bacterial Meningitis Spreads According to the Centers for Disease Control and Prevention, people living in close quarters are more likely to spread this illness to one another. For example, you may have heard about the higher risk of meningococcal (or bacterial) meningitis for new college students. The risk is so serious that many colleges and universities require proof of a vaccine for new students moving into campus housing. This includes the University of Nevada, Reno. To clarify, all incoming freshmen under 23 years of age must show proof of their up-to-date meningitis shot. “Bacterial meningitis is considered a medical emergency, and anyone with the signs and symptoms should be evaluated in the emergency room immediately,” says Vanessa Slots, MD, Renown pediatrician. Symptoms of Bacterial Meningitis Fever Nausea Vomiting Irritability Headache Confusion Back pain Stiff or painful neck Leg pain Light sensitivity Rash on the torso or lower extremities It’s important to know many of these symptoms for both bacterial and viral meningitis are the same. However, the viral type is more common, often clearing up in seven to 10 days without complications. Nonetheless, you should go to the emergency room to be looked at, as the signs are similar for both illnesses. Why is Bacterial Meningitis Dangerous? This illness moves quickly, and in some cases, it can seem like the flu or severe strep throat and take a few days to develop. Or, it can hit in just hours. “Bacterial meningitis has an overall death rate of 10 to 15 percent despite treatment with antibiotics,” Dr. Slots warns. Another critical point is problems after recovery can also be severe. Frequently these include brain damage, amputations, infections around the heart, seizures and shock.
-
Celebrating Renown Health's Nursing Excellence Conference
Renown Health recently wrapped up the twentieth annual Nursing Excellence and Excellence in Critical Care Conferences, the conference theme was the Courageous Calling and over 400 nurses from specialty fields across the region attended to learn, reflect, build relationships and obtain continuing education units (CEUs). Celebrating The Courageous Calling During the first day of the Nursing Excellence Conference, local and national leaders presented topics including redefining resilience, documentation liability, transgender healthcare and caring for the homeless population. Among the list of impressive speakers were Chief Nurse Executive at Renown Health, Melodie Osborn, and Nora McInerny, writer and host of the "Terrible Thanks for Asking" podcast. On day two,speakers focused on the critical care specialties within nursing, including intensive care, emergency room, pediatric intensive care and neonatal intensive care. Topics covered included post-COVID-19 pulmonology with Dr. Graham, traumatic brain injuries with Dr. Demers, COVID-19 reflections with Anicia Beckwith, a discussion about "Mis C” with Dr. Healy, innovations in imaging with Dr. Rangaswamy and cardiology with Dr. Danaf. Thank you to our sponsors and raffle donors for making this event possible: Erik Olson and Larry Duncan, Jana Elliott, Melodie Osborn, Becky Haase, Lori Tuntland, Dr. Akbar, Dr. Lous, Mel Morris, Grand Sierra Resort, Renown Health Gift Shops, Renown Health Directors of Nursing, Renown Health Marketing & Communications Department, Renown Health Dermatology, Laser, & Skin Care and Renown Health Foundation. Learn more about finding purpose in the health of our community when working at Renown Health here.
Read More About Celebrating Renown Health's Nursing Excellence Conference