Buscar
-
¡Damas! Hágase un examen de detección de cáncer de mama
Early detection is a significant piece of the breast cancer puzzle. Susan Cox, Renown Health Senior Director of Cancer Operations, discusses what you need to watch for and how the latest technology can help detect potential cancer sooner. When should women start getting breast exams? It depends on risk factors: Average-risk women: Most medical organizations recommend the first mammogram between 40 and 44. Higher-risk women: Dependent on their high risk, which will dictate when they start screening, but generally around the age of 30 and not before 25 years old.
-
Cómo comenzar y actualizar su testamento
August is National Make-a-Will Month. We talked to Abbey Stephenson, Planned Giving Officer at Renown Health Foundation, to learn more about wills, trusts and estate plans and why you should feel motivated this month to get started. Why Make a Will There are so many reasons why it is difficult to make a will or put an estate plan in place. These include: Lack of time or money to prepare a plan The misperception that “only rich people need an ‘estate plan’” How intimidating legal documents can be General discomfort with planning for the future Given the barriers to making a plan, it’s not surprising that only 32% of Americans have a will or trust in place. But having a will or trust matters because these are the documents where you can say who will inherit your assets, who will manage your assets and estate, and who should be guardian of a minor or a child with a disability. Where to Begin If you have been thinking about putting together a will and don’t know where to begin, here are some next steps you can take. 1. Learn the terms. If you have never created a will, trust, or an estate plan, the language can be hard to get used to. A few important terms to know include: Last will and testament (also known as a will): a legal document that describes how you would like your property and other assets to be distributed after your death. This is also the document where you can nominate a guardian for a minor or disabled child. Personal representative (also known as an executor): a person named in a will responsible for collecting your assets, paying your debts and final taxes, and distributing the remaining assets to those stated in your will. Personal representatives must be formally appointed by a judge and report certain information to the judge for review and approval. Living trust (also known as a revocable or family trust): a legal arrangement set up through a document called a trust instrument or a declaration of trust that gives someone called the trustee power to make decisions about the trust creator’s money or property held in the trust. Estate plan: a collection of documents that help organize what happens to you and your assets upon your disability and death. Your estate plan is comprised of documents such as a will, trust, and advance health care directive. If you want to learn more about these terms and estate planning in general, you are invited to attend a free one-hour estate planning education session on Aug. 22, 2024, at 10 a.m. or Oct. 21, 2024, at 11 a.m., hosted by Renown Health Foundation. Click here for more information and to register. 2. Create a list of assets. Start by creating a list of your assets including real estate, investments, bank accounts, retirement accounts, business ownership interests, vehicles, life insurance, valuable personal property like jewelry or artwork, and any other significant assets. Click here and read our free estate planning guide. 3. Put together a list of 2-3 people you trust. When you create your will, you need to name a personal representative who will collect all your assets, pay your debts, and work with the probate court to distribute the balance to the people and charities you name in your will. If you create a trust, you need to name a trustee to manage the trust assets under the terms of the trust document. It is a good idea to include at least two people who can take on these roles in case the first person becomes unavailable. If you do not have anyone you would trust as a personal representative or trustee, there are trust companies, banks, and other professionals and institutions who may be able to assist you. If you are the parent of a child who is under 18 or has a disability, you will also nominate a guardian in your will to care for that child if you and the other parent are gone. 4. Start a list of who you would like to inherit your assets. Which people and organizations would you like to inherit the assets you own at the time of your passing? And which assets or how much would you like them to receive? You might want to consider who relies on you for support such as family members or charities, individuals and organizations that have made a difference in your life, or those you have a special fondness for. It is important to use the legal names of individuals you include as beneficiaries and the Tax ID number for any charity you include. If you decide to make a gift to Renown as part of your will or estate plan and notify us, you will be included in the Renown Legacy Society. Legacy Society members enjoy invitations to exclusive events, special acknowledgments, and other unique benefits. Click here to learn more about the Renown Legacy Society. 5. Put together a list of your professional advisors and enlist their help. Write down the names and contact details for any professional advisors you work with such as your accountant, financial advisor, investment manager, attorney, insurance agent, and planned giving officer. You may want to seek their advice on how best to proceed and which assets are best gifted to which individuals and organizations from a tax standpoint. Collaboration among the professionals with whom you work can help your plan to run more smoothly when it is needed. Depending on your circumstances, it may make sense for you to introduce your trusted individuals to these professionals. 6. Start drafting. Once you have these items in place, you will be in a good position to begin the drafting process. There are many capable estate planning attorneys in our community who can help you with drafting. There are other drafting resources available as well, but only a licensed attorney can provide you with legal advice. Click here to attend the free Family Estate Planning Series sponsored by Renown and presented by PBS Reno and the Community Foundation of Northern Nevada.
Read More About How to Get Started and Make Updates to Your Will
-
¿Las mamografías duelen? 4 Mitos desacreditados
Mammograms are an effective means for early detection of breast cancer. Still, many women shy away from them for fear of pain or discomfort. Let us debunk a few mammogram myths that will remove your worries and encourage proactive breast health. Reviewed by Dr. Colleen O'Kelly-Priddy, MD, FACS, breast surgical oncologist at Renown Women's Health. Myth 1: Mammograms Are Painful Reality: Although some women experience discomfort during a mammogram, most say it is not painful. Breast compression, which is important to get a clear image, can cause a sensation of pressure, but this lasts for a few seconds. Let your technician know how much pressure you can handle so you're not uncomfortable. Myth 2: Discomfort Persists Long After the Procedure Reality: The sensation of pressure developed through the compression process diminishes quickly after the procedure. Most women go about their day afterward without experiencing any residual pain.
-
7 Síntomas del cáncer de mama en mujeres jóvenes
Cancer can develop at any age, and that’s why the experts at Renown are ready to help you stay ahead of breast cancer, especially if you're in your 20s or 30s. We're talking about early detection, signs to be aware of, and why being proactive is a big deal. Studies show there has been an increase in breast cancer in younger women. Although breast cancer is rare in women under 40, when it occurs, it tends to be aggressive. The tricky part? Many young women don't think it can happen to them, so they don't check for the signs as often as they should. Reviewed by Dr. Colleen O'Kelly-Priddy, MD, FACS, breast surgical oncologist at Renown Women's Health. Early Signs and Symptoms New or Different Lump in the Breast: A lump is probably the most well-known symptom. Breast cancer is usually painless and firm, but it can also be soft. If you find a new lump, don't panic, but don't ignore it either. Changes in Breast Size or Shape: Have you noticed that one breast looks a little different? Whether it's swelling, shrinking, bulging, dimpling, or seems off, it's worth mentioning to your doctor. Skin Changes: If the skin on your breast starts to thicken or turn red, it's time to pay attention. If your skin starts looking like an orange peel (thickened, with prominent pores), that warrants evaluation. Nipple Discharge: Spontaneous drainage coming from your nipple that isn't breast milk—especially if it's clear or bloody—should be checked out. Nipple Changes: If your nipple starts to invert, flatten, or look different, call your doctor. Breast Pain: Continuous pain in your breast or nipple that isn't linked to your menstrual cycle is another symptom to note. However, breast pain is very common and is only rarely a sign of cancer, so don’t panic. Swelling or Lumps in the Armpit: When it spreads, breast cancer usually first goes to the lymph nodes in the armpit, so swelling or lumps under your arm should be on your radar.
-
Guía para exámenes de detección de cáncer
One of the most crucial aspects of maintaining health and wellness is staying proactive about regular cancer screenings. Early cancer detection significantly increases the chances of successful treatment and survival. The multidisciplinary care team at the William N. Pennington Cancer Institute at Renown Health provides compassionate care and support to the community for early detection and diagnoses. This comprehensive guide outlines the various cancer screenings available for breast, colorectal, lung, cervical, prostate and skin cancer. Breast Cancer Screening Who Should Get Screened? Mammograms are recommended starting age 40 for those considered at average risk for breast cancer. Women with a family history or other risk factors should discuss appropriate screening options with their healthcare provider. Women under 40 with a family history should discuss risk factors with a healthcare provider. Screening Methods Mammogram: This provides an X-ray of the breast and can detect tumors that are not yet palpable. Breast MRI: This type of scan is recommended for women at high risk for breast cancer due to genetic factors or family history. Screening Breast Ultrasound: This scan can help in identifying masses in denser breast tissue that might not be visible on mammogram. It is recommended in addition to a mammogram for patients at a higher risk for breast cancer. What to Expect During a mammogram, the breast is compressed between two plates to capture X-ray images. Some pressure or discomfort may be felt, but the procedure is brief and critical for early detection. Colorectal Cancer Screening Who Should Get Screened? Adults aged 45 to 75 should undergo regular colorectal screenings. Some adults under 45 may need to be screened earlier depending on family history or other genetic risks. Those over 75 should consult with their healthcare provider to determine if continued screening is necessary. Screening Methods Colonoscopy: This procedure uses a flexible tube with a camera to examine the entire colon. Fecal Immunochemical Test (FIT): A non-invasive test that detects hidden blood in the stool. CT Colonography (Virtual Colonoscopy): Uses Computed tomography (CT) imaging to provide detailed views of the colon. What to Expect A colonoscopy can detect changes or abnormalities in the large intestine (colon) and rectum. Screening is usually advised every ten years, but if you are at risk, screening may be recommended every 3 to 5 years after your initial colonoscopy. Colonoscopy preparation includes bowel cleansing the day before and sedation during the procedure. FIT is a simple at-home test requiring no special preparation. Lung Cancer Screening Who Should Get Screened? Adults aged 50 to 80 with a significant smoking history (20 pack years or more) and who currently smoke or have quit within the past 15 years. Screening Methods Low-dose Computed Tomography (LDCT): A CT scan with low radiation doses to create detailed images of the lungs. What to Expect LDCT is a non-invasive scan that requires you to hold your breath for a few seconds. Cervical Cancer Screening Who Should Get Screened? Women aged 21 to 65 should undergo regular screenings. Women aged 21 to 29 should have a Pap test every three years. Women aged 30 to 65 should have a Pap test and HPV test every five years, or a Pap test alone every three years. Screening Methods Pap Test (sometimes called a Pap Smear): Collects cells from the cervix to detect precancers. HPV Test: Identifies high-risk human papillomavirus (HPV) types that can cause cervical cancer. What to Expect The Pap test involves collecting cells from the cervix using a small brush. Some discomfort may be felt, but the procedure is brief and crucial for early detection. Prostate Cancer Screening Who Should Get Screened? Men aged 50 and older should discuss screening options with their healthcare provider. Men at higher risk (African American men and those with a family history of prostate cancer or are a BRCA2 gene carrier) should begin discussing screenings at age 40. Screening Methods Prostate-Specific Antigen (PSA) Test: Measures PSA levels in the blood. Digital Rectal Exam (DRE): A physical examination where the provider feels the prostate through the rectum to detect abnormalities. What to Expect The PSA test is a simple blood test. The DRE may cause slight discomfort but is quick and essential for early detection. Skin Cancer Screening Who Should Get Screened? Anyone with a suspicious lesion or abnormal area on their skin. Individuals with more than 50 moles or dysplastic moles. Those with a personal history of melanoma or history of other skin cancers. Those who have more than one member of immediate family with a history of cancers (melanoma, breast cancer, pancreatic cancer) or a family member who was diagnosed with melanoma before they were 50 years old. Positive gene testing for BRACA2, Lynch syndrome genes (MLH1, MSH2, MSH6, PMS2 or EPCAM). Screening Methods Skin Exam: A visual examination by your provider to check for unusual moles, birthmarks, or other skin changes. Biopsy: Removal of a small sample of skin for testing if an abnormal area is identified. What to Expect A skin exam is non-invasive and visual. A biopsy involves minor discomfort and local anesthesia if needed. Expert Advice Although the cadence of these skin screenings may or may not be annual, as one's age increases, the risk of many cancers rises. Everyone benefits from attentive sun protection, including avoiding direct sun between 10 a.m. and 4 p.m. by seeking shade and wearing hats, clothing and sunscreen. When purchasing sunscreen, look for SPF 50, UVA/UVB broad spectrum. Questions to Discuss with Your Healthcare Provider What is my risk level for different types of cancer? Which screening tests do you recommend for me and why? What are the potential risks and benefits of each test? How often should I get screened? What steps to follow if a test result is abnormal? Importance of Cancer Screenings Regular cancer screenings are vital for maintaining your health and catching cancer early, when it is most treatable. Renown Health is dedicated to guiding you through the process and providing the highest quality of care. Consult with your healthcare provider to determine the appropriate screenings for your specific needs and to take proactive steps toward a healthier future.
-
Cómo detectar la depresión en los hombres
Is a man in your life struggling with depression? Many men find it difficult to acknowledge when they need help. Recognize their unique warning signs of depression with insights from psychologist Dr. Herbert Coard. Over 6 million men are diagnosed annually, often displaying symptoms like anger and aggression instead of sadness. Learn how to support them and understand these often-misinterpreted indicators. Behavioral Signs of Depression in Men High levels of the hormone cortisol are released during stressful situations affecting the neurotransmitter, serotonin (a feel-good hormone), contributing to depression. You can identify depression or suicidal tendencies by paying close attention to the following behavioral changes: Anger, irritability, or aggression Avoiding family or social situations Losing interest in family responsibilities, passions and hobbies Lack of sex drive Becoming controlling/abusive in relationships Risk-taking behavior such as; unsafe sex, overspending or gambling Not being able to concentrate or remember details Excessive drinking or drug use Having frequent thoughts about death Talking about suicide Attempting suicide Factors That Lead to Depression in Men Life Events Work stress or long-term unemployment can be huge contributing factors relating to depression. This type of life event can be overwhelming, making it impossible for a man to cope. Changes in Relationships The loss of a relationship can be a significant contributing factor to the emergence of depressive symptoms and past experienced physical, sexual, or emotionally abusive relationships. With this in mind, counseling can often help individual to overcome this type of trauma. Grief and Loss Overwhelming sadness due to the loss of a loved one can trigger depression. Although normal, each person goes through their own grieving period. For example, normal responses to death are insomnia, poor appetite and loss of interest in activities. Pay attention if grief seems prolonged or out of the ordinary. Health Problems In particular, depression coexists with medical conditions. As men age, this can be passed off as normal aging, but it could be more serious. In addition, illnesses such as thyroid disorders, Addison’s disease and liver disease can cause depressive symptoms. Diabetes, cancer, heart disease, or Parkinson’s disease can affect any age, thus triggering or worsening depression. Some older men also feel like they may be suffering from dementia because of difficulties with memory this may be a symptom of depression. A trip to the doctor may be in order to help alleviate concern and worry. Depression in Men and Suicide Frequently the emotional pain occurring with depression can distort a man’s ability to see a solution beyond suicide. Individuals with depression become very rigid and constricted in the way they solve problems. The statistics below speak for themselves, helping us understand the need to reach out to those who need our support. Male suicide rates are on rising – men die by suicide 3.53 times more often than women, accounting for 70% of all suicides. Sadly, every day 129 men commit suicide. White males accounted for 69.67% of suicide deaths in 2017. In 2017, firearms accounted for 50.57% of all suicide deaths. Middle aged Men who are middle aged have the highest suicide rates. 40% of those identifying as transgender have attempted suicide in their lifetime. Males who are guy or transgendered are at an increased risk for suicide attempts, especially before age 25. Veterans often suffer from post-traumatic stress disorder (PTSD) and depression, and are more likely to act on a suicide plan. How You Can Help Now that you can identify some of the warning signs of depression, here’s how you can help: Talk about your concern and communicate that you’re there to help him. Let him know depression is a medical condition and will usually get better with treatment. Suggest professional help from a Primary Care Provider, Psychologist or Therapist. Help set up appointments and offer to accompany him – let him make the decision, but make it clear you’re there for him, no matter what he decides. If you feel he is in a dire or life-threatening situation, contact 911. Call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to talk to a trained counselor. Call the Veteran’s Crisis Line at 1-800-273-TALK (1-800-273-8255) and press “1”
-
Departamento destacado: Programación de cirugías y procedimientos
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
Lo que necesita saber sobre el ahogamiento por agua fría
Northern Nevada's stunning lakes, including Lake Tahoe, with its average summer water temperature of 50 degrees, present a potential risk of hypothermia. Unlike mild 50-degree air, water at the same temperature poses severe, life-threatening risks, including rapid-onset hypothermia and drowning. Awareness of the symptoms and taking proper precautions are crucial to prevent cold-water drowning. The 4 Phases of Cold-Water Drowning 1. Cold Shock Response: This response affects breathing and happens within the first minute. An automatic gasp reflex occurs in response to rapid skin cooling. If the head goes below water, water may be breathed into the lungs, resulting in drowning. A life jacket will help keep your head above water during this critical phase. Additionally, hyperventilation, like the gasp reflex, is a response to the cold and will subside. Panic will make this worse, so the key is to control breathing. 2. Cold Incapacitation: This response occurs within the first five to 15 minutes in cold water. In order to preserve core heat, vasoconstriction takes place decreasing blood flow to the extremities to protect the vital organs. The result is a loss of movement to hands, feet, arms and legs. Unless a life jacket is being worn, the ability to stay afloat is next to impossible. 3. Hypothermia: Important to note, it can take 30 minutes or more for most adults to become hypothermic. So there’s time to take action and survive. Keeping panic at bay is critical, as you have more survival time than you think. Symptoms include: Shivering Slow and shallow breathing Confusion Drowsiness or exhaustion Slurred speech Loss of coordination Weak pulse 4. Circum-rescue Collapse: This experience can happen just before rescue and is not well understood. Symptoms range anywhere from fainting to death. Some experts believe an abrupt drop in blood pressure may cause this final stage of cold water drowning, post-rescue. Additional Safety Tips and Helpful Resources Always wear a personal flotation device as well as a wetsuit or drysuit. Your personal flotation device is the most important piece of water safety gear. Try not to panic as the first phases will subside. Controlled breathing is to staying calm. Research suggests the body can withstand the cold longer than we think. The Heat Escape Lessening Posture (HELP) is a position which helps conserve energy if you’re wearing a personal flotation device. By hugging your knees to your chest, this posture helps maintain body heat for some time.
Read More About What You Need To Know About Cold Water Drowning
-
Departamento destacado: Ingeniería de instalaciones
When an appliance or fixture stops working at home, who do you contact? If your lights stop working, you call an electrician. Is your air conditioning unit out of order? Reach out to an HVAC (heating, ventilation and air conditioning) technician. What about if your sewer drains start backing up? Time to contact a plumber. And if your fire safety equipment needs servicing? Better call a fire safety technician. Regular maintenance and repairs on the inner workings of your household are always important, and when something goes wrong, it can be distressing and inconvenient to you and everyone living with you. You feel the need to get the issue resolved as quickly as possible, right? Now imagine that those needs are magnified – to the tune of hundreds of thousands of people every year. Who could potentially take on such a monumental task? Enter: Facilities Engineering at Renown Health. Crucial to ensuring our health system performs at its peak, these team members step in to make sure every patient, team member and visitor who walks through any of our doors are able to access the facilities they need and make their time with us as comfortable – and as successful – as possible. The Silent Heroes As our care teams move heroic mountains to save lives, another set of heroes emerge behind-the-scenes. As a strong backbone of our health system, the Facilities Engineering department plays a key role in maintaining the infrastructure that supports patient care, from ensuring the HVAC systems are functioning optimally to maintaining the plumbing and electrical systems that keep the lights on and the equipment running smoothly. Renown is fortunate to have some of the most dedicated journeymen in the business. This team boasts many experts, including: Plumbers Fire Safety Technicians Craftsmen HVAC Journeymen Electricians Boiler Operators Facilities Technicians As one can imagine, every day brings on a new challenge for our Facilities team members. “Each workday is always different; it could be water, power or HVAC issues or anything in between,” said Nhil Dado, Supervisor of Facilities Services. “We are proud of the services we provide for the needs of patients and employees.” “Every day, we have a variety of equipment to work on,” added Alfred Santos, HVAC Journeyman. “Whether it’s facility upkeep, plumbing, HVAC or electrical, we want to help,” added Brian McCarty, Facilities Technician. This department works around the clock to ensure that every aspect of our hospitals and outpatient care locations meets the highest standards of safety and efficiency, from routine maintenance and equipment improvements to emergency repairs. These are huge responsibilities – all of which they perform with pride. “As an HVAC journeyman, we are responsible for making sure the air circulating in the hospital is clean,” said Christopher Bobis, HVAC Journeyman. “It is also our job to make sure the air is positive and negative in isolation rooms and ensure patients are satisfied with the temperature in their rooms.” “In addition to performing regular maintenance tasks like changing air and water filters, we complete any random work order that may come up,” added Brett Courtney, Facilities Technician. “We also recently switched out our lighting at Renown South Meadows to LED lights, which helps with energy savings.” “I overlook the boiler house equipment and coordinate the fixing of maintenance issues reported by hospital staff,” added Arnt Utnes, Boiler Operator. “We also respond to every single alarm." It’s difficult for us to imagine what our health system would be like without the Facilities team providing us with the comfortable and safe environment our patients need and deserve. Luckily, we’re never alone in our efforts to keep us running, and this department expertly leads that charge. “Along with writing down the PSI readings in the gas rooms and answering calls from dispatch and the boiler rooms, I go through all the daily work orders and complete them,” said Ken Carrillo, Facilities Technician. “It always feels good to see when we complete all the work orders for the day, especially as the next shift arrives.” “We fix, replace and dispose of pieces that are no longer in service – bottom line, we help keep the building up and running,” added Alejandro Cardenas, Craftsman. But it doesn’t stop there – Facilities Engineering is currently in the midst of creating a whole new fleet vehicle program to improve the operations of our many on-site vehicles, including trucks, forklifts and more. “I am the point of contact for all things fleet,” said Michelle Bay, Administrative Assistant. “We are building a new fleet program and working closely with leadership to move the program forward. I am involved with setting up new fleet fuel cards and can set up the program in the best interest of our internal customers while looking to the future for growth.” It’s clear that the Facilities team is indispensable to Renown. Through their expertise, professionalism and commitment to quality, they stop at nothing to keep our health system functioning at its highest level.
Read More About Department Spotlight: Facilities Engineering
-
Optimización de las mamografías: Un enfoque genético para un cronograma de pruebas de detección personalizado
© Arthon Meekodong via Canva.com Breast cancer screening has long been a cornerstone of women's healthcare. With 1 in 8 women diagnosed with breast cancer in their lifetime1, the United States Preventive Services Task Force (USPSTF) has developed screening recommendations to help detect early-stage cancer. Notably in 2023, the USPSTF revised the recommended age for biennial mammogram screenings for women with average risk to start at age 40 instead of 502, estimated to result in 19% more lives being saved3 by starting screening earlier. While initiating screening at an earlier age offers advantages to a wide demographic, concerns about the potential of over-screening prompted research into the feasibility of identifying women with lower breast cancer risk who could safely delay mammograms. While guidelines address high-risk individuals, a notable gap exists in providing recommendations tailored to those at lower risk. To gain insight into a patient's risk level, physicians are able to utilize genetic testing to understand an individual's genetic makeup, providing precise insights into their predisposition to various health conditions, including breast cancer. Armed with this genetic information, healthcare providers could craft tailored screening strategies that align with an individual’s specific risk profile. This genetic risk-based approach underscores the value of genetics in individualizing the onset of screening to help avoid over-screening and its associated costs. Surprisingly, genetic information is not currently being widely utilized to identify women at risk of breast cancer or other diseases in clinical practice, despite its potential to make a significant positive impact for patients. A recent retrospective analysis of 25,591 women from the Healthy Nevada Project4 sheds light on the potential benefits of this genetic risk-based approach. The study classified 2,338 (9.1%) of these women as having a low genetic risk for breast cancer. What's remarkable is that these women exhibited a significantly lower and later onset of breast cancer compared to their average or high-risk counterparts. This finding suggests that it might be safe for low-risk women to delay mammogram screening by 5 to 10 years without compromising their health.
-
Departamento destacado: Piscina flotante
Ring in the New Year and the rest of the holiday season by celebrating Renown’s Float Pool team! After coming out of the COVID-19 pandemic, it's no mystery that healthcare across the country has shifted and adapted to the growing needs and new demands of our patient populations. Renown Health is no different. As the largest not-for-profit health system in the region, we are no stranger to change, even when change presents challenges. Who do we call on when a unit needs more team members in the eleventh hour? Who can help when our patient volume spikes up with seconds to spare? This is where the Float Pool at Renown comes to the rescue. Skilled in a wide variety of healthcare specialties, from acute care nursing and critical care to care aiding and patient safety, this is the team that can seamlessly step in to provide crucial patient care to the units that need it most, whether a team is understaffed for the day or needs extra all-hands-on-deck for a specific patient or procedure. Float Pool team members are equipped to work in virtually any clinical area at Renown, making a genuine difference with every patient they encounter. A Pool of Relief Teams across Renown can breathe a sigh of relief knowing that Float Pool has their back in times of need. As the backbone of our health system, these dedicated team members possess a wealth of clinical knowledge and the ability to navigate diverse medical environments. Their flexibility allows them to fill staffing gaps and provide essential support to many different units. “We fill in the gaps of staffing to make everyone's day better,” said Patti Crepps, Critical Care Float Pool RN. “A float nurse has to be flexible and able to adapt to different situations and places – basically, ‘go with the flow.’ Patient care is basically the same all over; we make patient care possible by being familiar with all the various specialties and providing the specific care needed depending on the population we are taking care of on that shift.” “Float Pool staff members are like healthcare chameleons, transitioning between different departments,” added Shelby Riach, Acute Float Pool RN. “We incorporate flexibility, teamwork and a commitment to ensuring patients receive the best care, regardless of the setting or circumstances.” This team thrives in uncertainty; in fact, no workday is the same in Float Pool – and that’s exactly the way they like it. Working with many different teams across a multitude of specialties, these Care Aides, RNs, Critical Care Techs, Patient Safety Assistants (PSAs), Certified Nurses Assistants (CNAs) and more enjoy facing change, while they all share a goal of providing the best patient care possible. “No day looks the same; since we are the Float Pool, we are assigned a different assignment on Smart Square every day, whether it be as a care aide, a patient safety assistant, a unit clerk or patient transport,” said Melina Castenada, Care Aide. “If we are assigned as a care aide on the floor, we help assist with call lights and help with whatever nurses and CNAs may need, including feeding, transporting, walking, helping patients use the restroom, etc. When we are assigned as a PSA ‘sitter,’ we sit for the patient to help keep them safe. If we are assigned as unit clerk, we help answer phones and direct patients appropriately, file paperwork, answer call lights if needed and assist with office work.” “I love that every day is a different floor with different tasks and a different atmosphere,” added Julia Chappell, Critical Care Technician. “I find out which floor that I will be on right before my shift starts and head to the floor to find out my assignment for the day. Depending on the specialty, such as the medical-surgical floor versus an intensive care unit (ICU), my daily job tasks can vary.” When it comes to high-risk patients, who require special attention, PSAs within Float Pool step in to help. “The PSA role within Float Pool largely consists of adverse event prevention for our high-risk patients, and being a Float Pool employee allows us to work wherever we are needed,” said Dimitri Macouin, Patient Safety Assistant. “Whether it be in the emergency department, neurology or pediatrics, the PSA will be the eyes and ears for the nurses working with this patient population.” “Great strides have been made to ensure that PSAs remain vigilant and are recognized as an integral part of the patients' care team rather than 'just a sitter,’” added Karla Phillips, Patient Safety Assistant. Float Pool also oversees our Discharge Lounge, which offers patients and their families a dedicated space to reconnect and prepare for their discharge from the hospital. “The increase in utilization of the Discharge Lounge is something we are very proud of,” said Kara Abshier, Care Aide. “We assist in discharging patients from all over the hospital to help the floor and get new patients into rooms.” Every day brings a new challenge for Float Pool. As these team members wake up with uncertainty, they are ready to embrace the diverse demands of caring for patients of all ages. “The fact that Float Pool exists is amazing,” said Hannah Luccshesi, Acute Float Pool RN. “We wake up with no clue as to whether we will be working with babies, children or adults and then fill in the needs of the hospital.”
-
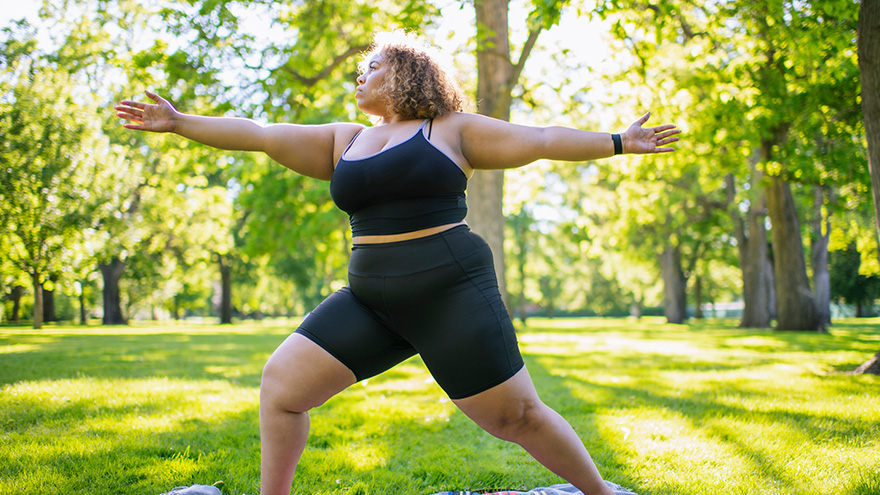
Estrategias para una pérdida de peso duradera
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery










.png?rev=fcd27802b7604a96bf1056b050ef90c5)