Buscar
-
Un viaje de apoyo: Cómo las subvenciones de la Sociedad Americana contra el Cáncer afectan a los pacientes en Renown
For many cancer patients, a significant hurdle is simply getting to treatment. Patients from Nevada and California often face considerable financial and logistical challenges when traveling for care. Limited resources for transportation and lodging can result in missed appointments, treatment interruptions and delays in follow-up care. To address this crucial need, Renown Health Foundation partners with the American Cancer Society (ACS) to ensure our patients can access the care they need by reducing financial barriers many patients face ACS awarded $70,000 to Renown Health Foundation last year. These funds, distributed as gas cards and lodging support to qualifying patients, have proven to be a lifeline in assisting those in need. Fueling Hope with Gas Cards Through our partnership with ACS, Renown supported 128 cancer patients over the past year. This assistance provided 2,260 round trips, ensuring that patients from Nevada and California could attend their critical treatments at the William N. Pennington Cancer Institute at Renown. These patients, aged 15 to 94, traveled up to 320 miles, sometimes from remote areas such as Tonopah, Elko and Susanville, for their cancer care “We're deeply committed to supporting our patients through every step of their journey, and our partnership with the American Cancer Society is instrumental in making that happen,” said Jocelyn Mata, Oncology Social Worker at the Pennington Cancer Institute. “Without them, we wouldn't be able to provide the crucial financial assistance that many of our patients need.” Jocelyn works with qualifying patients to provide gas cards and accommodations at The Inn at Renown, a hotel at Renown Regional Medical Center. She ensures they can focus on their treatment without worrying about the financial burden. Lodging Support for Peace of Mind Along with transportation aid, we can provide safe and comfortable lodging for qualifying patients. "We encourage patients to rest and, if they have a long journey home, to stay overnight," said Dr. Max Coppes, Director of the William N. Pennington Cancer Institute. "Providing lodging support ensures they have a safe and comfortable place to recover before making the trip back." This assistance is crucial for those who travel far from home, allowing them to focus on healing without the added stress of finding and affording accommodation.
-
Las piezas del rompecabezas: Thonet LaBadie’s Breast Cancer Journey
“A breast cancer diagnosis begins much like a jigsaw puzzle to be worked through. It’s an overwhelming mess of scattered pieces that make no clear sense, poured out of the box into a crumbling pile of confusion. But slowly with persistence, focus, determination, a positive attitude and working through the challenges day by day and piece by piece, they in time both become whole and beautiful again.” – Thonet LaBadie On Feb. 13, 2015, Thonet’s life as she knew it took a drastic turn. In just one moment, everything shifted. The happy and healthy wife, mother of 17-year-old twins, former teacher and immunization specialist was about to face the fight for her life. That fateful day nearly a decade ago was when she received the unsettling news: she had breast cancer, and it had metastasized to her lymph nodes. Though she was faced with a daunting diagnosis, Thonet’s positive spirit and zest for life never wavered. Never did she think, “why me?” Nor did she think, “I’m not strong enough.” Her thought process was quite the opposite – “I am going to ride this rollercoaster until it stops, and I walk away cancer free.” With her loving family and friends rallying behind her, as well as her expert Cancer Care teams at Renown Health and Cancer Care Specialists (formerly known as Reno Oncology Consultants), Thonet knew that her journey would not be traveled alone, and she was determined to defeat cancer once and for all. She promised her daughter Jourdyn she would stay strong and not give up the fight. The Unexpected Discovery Thonet did everything she believed was right in her preventative healthcare journey. She lived an active lifestyle, she filled her life with love and happiness, she did not have any genetic markers for breast cancer and never missed a preventive check-up. Someone like her shouldn’t develop such a debilitating disease, right? As it turns out, she was told by professionals that with this disease, it’s become more often not about who develops breast cancer – but when. Breast cancer makes up for about 30% of cancer diagnoses in women across the U.S. So, when Thonet felt a lump in her breast in Nov. 2014, she knew she had better play it safe than sorry. She took her concerns to her doctors, who ran all the necessary tests. The unfortunate result: invasive ductal carcinoma (stage 2B), the most common form of breast cancer. Though Thonet was terrified, she was also tenacious. She was ready to Fight the Good Fight right then and there. Thonet chose to undergo a bilateral mastectomy. So that’s precisely what she did in April 2015 at Renown Regional Medical Center. Thonet was ready to put breast cancer behind her, but unfortunately, the trek was just beginning. During her mastectomy, her care team tested her lymph nodes. Four were removed. What came next was her most valiant fight of all: chemotherapy coupled with radiation, as well as more reconstructive breast surgeries along the way. Courageous Connections With 36 radiation treatments, 8 rounds of chemotherapy, 6 surgeries and 1 brave spirit, Thonet's healthcare journey has been nothing short of vigorous. Fortunately, she had an expert oncology team on her side every step of the way. And it goes even further – Thonet’s college acquaintance Dr. Jennifer Sutton, an oncology physician at the William N. Pennington Cancer Institute (formerly the Renown Institute for Cancer), was her radiation oncologist. She felt comfort knowing that a significant aspect of her care was in the hands of a trusted physician and a team of loving nurses, cancer care navigators and radiation therapists, whom she calls the “Renown Radiation Rockstars.” Thonet felt an immense connection not only to her warm and welcoming care team but also the other oncology patients she met along the journey. Patients facing cancer often receive radiation treatments several times a week, so Thonet had a chance to make close relationships with the other patients who were on a similar path as she was. Throughout her treatment process, Thonet participated in cancer support groups, which she believes are vital for anyone diagnosed with the disease. “Had it not been for my diagnosis, I would have never met all the amazing people I did at Renown and beyond,” she recalls. “At the end of my treatments, I knew I was going to miss them.” The love and support of Thonet’s care team, fellow patients, family, friends and community helped her remain positive throughout the entire process, always focusing on the positive – even during the most physically and emotionally tolling parts of treatment. Crossing the Finish Line Every day brought a new obstacle to overcome, whether it was a treatment, a side effect or an emotional response to the intense journey. Thonet’s motto throughout it all was “day by day, one foot in front of the other, from start to finish.” In Dec. 2016, Thonet finally made it to that finish line. With the completion of chemotherapy and radiation behind her, she walked out the front doors of the Pennington Cancer Institute, threw her fist in the air in excitement and finally got to revel in the fact that she had her health back. She had survived. Inspired by her journey and her breast cancer “sisters” she met while in treatment, Thonet wanted to give the same level of care and attention she received back to her fellow community members battling cancer. She proudly serves as a breast cancer “angel,” offering comfort and support to those who need it most. Thonet is also looking forward to the completion of the Pennington Cancer Institute’s Conrad Breast Center, currently under construction at Renown South Meadows Medical Center, noting how important it is for breast cancer patients to have expanded access to crucial cancer care in south Reno. Today, at nine years cancer-free, Thonet is thoroughly enjoying her life. She loves traveling, spending time with family and seeing her now-adult son and daughter thrive in their own lives. She also recently underwent hip replacement surgery and is proud to be back on her tandem bike with her loving husband of 33 years, Mike, who she credits for his never-ending support in sickness and in health. “No looking back – only forward to healthy living. Onward!” Thonet exclaims. And for anyone out there going through cancer treatments, Thonet has some words of wisdom to take to heart: “Cancer chose the wrong person when it tried to tackle us. Stay strong and fight on, day by day. On even the most difficult, darkest day, remember that you are stronger than you know.”
Read More About The Pieces of the Puzzle: Thonet LaBadie’s Breast Cancer Journey
-
Conozca a Haley Longfield: Un terapeuta de radiación y corredor de barril reconocido
Many Renown Health employees have deep roots in the northern Nevada community and Haley Longfield is one of them. She’s a fifth-generation northern Nevadan currently living in Fernley and commuting to Reno three days a week for her job as a Radiation Therapist for the William N. Pennington Cancer Institute at Renown Health. She’s also a wife, mother of a 1-year-old, and an avid horseback rider who enjoys the western way of life. This year, Haley is excited to compete in the Reno Rodeo for a second time. A Life-Long Passion Haley started riding horses in the fourth grade and quickly fell in love with it. A few years later, she started barrel racing and developed a profound love for the adrenaline-filled sport. “When I turned 18, my dad gave me all of the responsibility of owning a horse,” said Haley. “Ever since then, I’ve been paying for and taking care of my own horses.” As many who know and love horses would likely agree, Haley says they are therapeutic for the mind, body and soul. “Riding horses is a great way for me to use my brain and focus, or think about nothing at all,” said Haley. Recently, Haley qualified to compete in this year’s Reno Rodeo in barrel racing with her 7-year-old mare named Hershey. “The first time I competed in the Reno Rodeo was quite a few years ago with my high school rodeo horse, and Hershey is the granddaughter of that horse,” said Haley. “The thing that I’m most excited about in competing at this year’s Reno Rodeo is getting to ride a homegrown horse in my hometown rodeo – she’s gorgeous, easy-going and gives it her all.” Above: Haley Longfield on her horse Hershey at a barrel race Circle of Support Haley feels grateful to have the support of her family, friends and team at Renown. “In addition to my family and friends, I have an incredible team at Renown that cheers me on both in my professional and personal endeavors,” said Haley. “I couldn’t do it all without them.” Alongside qualifying for the Reno Rodeo, Haley also recently received her bachelor's degree in applied science with an emphasis in radiation therapy. Her career development goals consist of moving into leadership within her department. “My leader and team have been nothing but supportive of my goals. Our leader is invested in everyone’s personal development and aspirations, as well as our professional and career development,” said Haley. “I’m excited to one day follow in my leader’s footsteps and help employees in our department reach their own goals. I aspire to become a great leader like she’s been to us.”
Read More About Meet Haley Longfield: A Renown Radiation Therapist & Barrel Racer
-
¿Cuándo debe considerar el hospicio? 5 Señales importantes
Deciding on hospice care for a loved one is a deeply personal and challenging decision, balancing their wishes and medical realities. Rebecca Edwards, DNP, from Renown Hospice Care, explains the signs indicating when it might be time for hospice and offers guidance on navigating this decision with compassion and clarity. Understanding Hospice Care Before exploring the decision-making process, it’s crucial to have a clear understanding of what hospice means. Hospice care represents a shift in how we approach living with a terminal condition, emphasizing comfort, dignity, and quality of life above all else. When there is no longer a pathway to a cure, side effects of treatment outweigh the benefits, or someone is simply tired of frequent hospital visits, then it may be time for hospice. Hospice care is mainly done in the home, where most people wish to be. It's a compassionate, team approach to care that focuses on meeting the physical, emotional, and spiritual needs, supporting their families, and honoring individual preferences. 5 Critical Signs to Be Aware Of Decline in Overall Health: When a loved one's health continues to decline despite ongoing medical interventions, this may be a sign that these treatments are no longer effective. Increasing Pain and Symptoms: When managing symptoms such as pain, nausea, fatigue or shortness of breath becomes increasingly challenging, hospice can offer specialized support and expertise in symptom management. Frequent Hospitalizations: Repeated hospitalizations or emergency room visits can signify that the disease has progressed to a point where managing symptoms and providing comfort at home or in a hospice setting is a more appropriate approach. Difficulty with Daily Activities: If your loved one is experiencing difficult with activity of daily living such as dressing, bathing, or mobility, it may be a sign that they require additional support and assistance. Prognosis of Six to 12 Months: Hospice Care is typically recommended for patients with a prognosis of about one year or less if the disease follows its normal course. However, it’s important to remember that every individual is unique and prognosis can vary.
Read More About When Should You Consider Hospice? 5 Important Signs
-
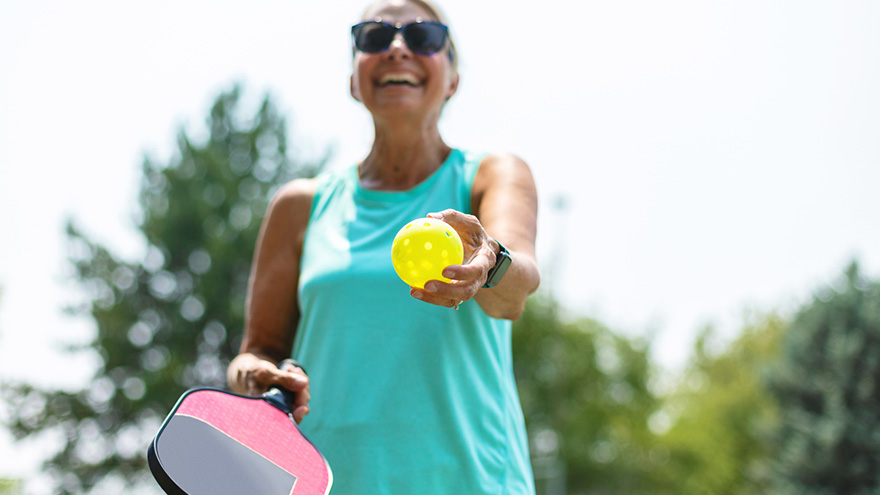
Los 5 principales beneficios para la salud de Pickleball
Over the past couple of years, pickleball has become the fastest-growing sport among people of all ages. It’s a combination of tennis, ping-pong and badminton that originated in 1965. This sport can be played indoors or outdoors on a pickleball court where two players (singles) or four (doubles) hit a perforated hollow plastic ball over a 36-inch-high net using solid-faced paddles. A pickleball court is the same size as a double’s badminton court and measures 20×44 feet. Pickleball is a fun, low-impact game that keeps people healthy and active. Kaitlyn Jacobson, Physician Assistant at Renown Urgent Care – Ryland, plays pickleball herself and is a big fan of the sport. Here she shares the top five health benefits of playing pickleball.
-
11 Consejos que los cuidadores deben conocer
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Departamento destacado: Terapia de rehabilitación de cuidados agudos
Being admitted to the hospital is never easy. Being admitted for a traumatic injury can be even harder. Whether it's learning how to walk again or powering through a new speech therapy routine, recovering from an injury that may affect the course of your life can be daunting. But it doesn’t have to be, thanks to the Acute Care Rehab Therapy team at Renown Health. The smiling faces of the Acute Care Rehab Therapy team at both Renown Regional Medical Center and Renown South Meadows Medical Center will make you see that there is a light at the end of the tunnel. Your dedicated physical therapists, occupational therapists and speech language pathologists are here to serve you and place you back on the right path to recovery and function. The Role of Acute Inpatient Therapy The Acute Care Rehab Therapy team comes in at a critical juncture in a patient’s care process after hospital admission. As one of the primary rehabilitation partners on a care team, these dedicated therapists are here to maximize every patient’s safe and independent living before they set off back home – all while reducing the risk of hospital readmission. “As physical therapists, we address musculoskeletal deficits and assess a patient’s current function after acute injury or illness from their baseline and develop a plan for functional recovery,” said Kristie Eide-Hughes, Physical Therapist at Renown Regional. “We also use our clinical expertise to assist with the discharge process and make sure each patient has the best durable medical equipment the first time around, removing the guesswork.” “On the occupational therapy side, we work with patients to facilitate their independence with basic life skills, such as dressing, bathing and using the restroom,” added Jeanne Clinesmith, Occupational Therapist at Renown Regional. “In the pediatric setting, we help babies and kids get back to what they were doing before they came into the hospital,” continued Rhonda Yeager, Pediatric Occupational Therapist at Renown Regional. “In the NICU specifically, we support the development of babies, trying to prevent problems from worsening. It’s nice to be a source of positivity in an otherwise intimidating situation.” The role of therapy in this setting reaches all ages, from babies in the neonatal intensive care unit (NICU) to adults approaching end-of-life care. Every therapeutic approach is tailored specifically to each patient. “Therapy is more of a habilitative approach for infants in the NICU, while it is more of a rehabilitative approach for kids and adults following injury or illness,” said Sara Carolla, Physical Therapist at Renown Regional. Each team member in the Acute Care Rehab Therapy department is dedicated to each patient, helping them make progress from start to finish and giving them the tools to succeed along the way. “I enjoy the variety of the patients we get to see and the ability to see them make gains from the wonderful treatment they get in the hospital from my team,” said Kelly Schwarz, Occupational Therapist at Renown South Meadows. “We provide education as each patient’s acute issues evolve,” added Nicole Leeton, Speech Language Pathologist at Renown Regional. “One of my favorite parts of my work is the patient and family education aspect, and that includes other healthcare provider education as well. It’s a moving picture.” Moreover, every team member gives each patient tools to learn how to be themselves again and empowers them to continue striving for the best possible result of their therapy “We get the opportunity to make a person’s bad experience in life better even by spending one session with them, giving them the keys to unlock something that they didn’t think they had the ability to do,” said Dana Robinson, Occupational Therapist at Renown Regional. On the Road to Independence Our dedicated therapists in the Acute Care Rehab Therapy team set the stage for a patient’s recovery process after trauma, showing them their potential for independence. With a multitude of patients coming into the hospital with many degrees of medical complexity, each day is different while the end goal is always the same: to optimize function as early as possible while overcoming any barriers and paving the way for a comfortable and effective quality of life. “Early intervention is a big piece,” said Nicole Leeton. “Us seeing patients early can get them recovered and independent more quickly and help prevent future illness and injuries. For example, in speech therapy, getting in early and facilitating communication skills for patients with impaired speech can make a huge difference.” Acute Care Rehab therapists dig deeply to see the whole picture of each patient’s situation to foster their independence – their history, social skills, support system and more. “Sometimes, we are the difference between independence and dependence,” said Dana Robinson. “We are the eyes and ears because we have so much time with the patients. Our team is extremely collaborative and develops a great rapport with patients, so they feel comfortable telling us everything going on with them.” “For kids, we teach parents ways they can help their kids by setting up their homes and the equipment they need to succeed,” added Rhonda Yeager. According to the team, one of the biggest keys to independence is repetition. A continual flow of getting up and trying again is crucial for recovery. “Repetition helps people regain their quality of life back sooner and control their recovery process,” said Megan Hough, Physical Therapist at Renown Health. “Helping people continue to get stronger and more independent makes my job so rewarding,” added Sam Brown, Physical Therapist at Renown Regional. Knowing that they have made a difference and help shape a patient’s overall development inspires each therapist to never give up, regardless of how difficult an injury presents. There is no set schedule for recovery, and the therapists are always in the patient’s corner. “This team has the most passionate, caring and dedicated individuals that I know,” said Kendra Webber, Manager of Acute Inpatient Rehab Therapy Services at Renown Regional. They give 110 percent to every patient every time to ensure they have what they need to regain function and independence.” “By tailoring therapy to the individual, the bounds are virtually limitless for what we can accomplish,” added Dana Robinson. It Takes a Village Since acute inpatient therapy is never a one-size-fits-all approach, it truly takes a village for this team to move the mountains they do for patients every day. These teams are fact-finding masters, gathering all the necessary information from the patient, their family and their care team to figure out their precise needs. “We are a consistent presence for our patients, identifying a lot of different needs and meeting those needs to help patients grow in their treatment process,” said Kelly Schwarz. “By collaborating with each patient’s diverse care team, we are able to employ the clinical judgment to help patients overcome physical, emotional and environmental struggles and set them up with the proper resources once they leave our setting.” “Our team has steady communication with physicians, nurses, acute care technicians, respiratory staff, physician assistants, case managers and more to ensure the best possible care,” added Jet Manzi, Physical Therapist at Renown Regional. Constant communication and collaboration are also necessary beyond the acute treatment process. These skills are vital in order to facilitate discharge planning, and the Acute Care Rehab therapists are an essential resource in the discharge process alongside our Hospital Care Management team. “Often times, a patient’s family needs a lot of guidance in helping their loved ones determine the next level, and we help them navigate those steps and the resources available to them,” said Mark Stumpf, Occupational Therapist at Renown Regional. “And it’s all a team effort.” “Our therapists are the most committed, generous, hardworking people,” added Courtney Phillips-Shoda, Supervisor of Rehab Therapy Services at Renown Regional. “Despite being short-staffed, we come to work every single day and give everything to our patients. They are the priority.” If you take away one thing, know this for certain: Renown’s Acute Care Rehab occupational, speech and physical therapists will always be there to help patients continue on a positive trajectory to physical, mental and emotional recovery. “Whether you are a patient or a provider, if there is a problem, never hesitate to reach out to us,” said Nicole Leeton. “We are always receptive to anyone seeking our help.” With the Acute Care Inpatient Therapy team on their side, a patient’s journey to recovery is only just beginning.
Read More About Department Spotlight: Acute Care Rehab Therapy
-
Consejos de seguridad sobre la enfermedad de Alzheimer para que los cuidadores los conozcan
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
Monkeypox: Un experto de Renown pesa
Renown Health is closely following the national outbreak of the monkeypox virus and urging healthcare providers to be alert for patients with illnesses associated with a rash. In working with the Washoe County Health District (WCHD), Renown is closely monitoring the spread of monkeypox in the community and looking to prevent and reduce the spread of monkeypox. To help to ease worries, we consulted with Paul De Leon, Infection Preventionist at Renown Health. What Exactly is Monkeypox? Monkeypox is a rare viral illness caused by the monkeypox virus — the same family of viruses that causes Smallpox. Although symptoms are similar to Smallpox, monkeypox symptoms are milder and rarely fatal. However, it's important to mention that this virus can be more severe for these susceptible groups: Immunocompromised Pregnant women A fetus or newborn baby Women who are breastfeeding Young children Those with severe skin diseases such as eczema How is Monkeypox Transmitted? The monkeypox virus is not easily transmitted but occurs through sustained person to person close contact with an infected individual. Monkeypox can also be transmitted through direct contact with infectious rash, scabs, or body fluids. Monkeypox can also be spread through prolonged intimate physical contact, such as kissing, cuddling or sex. Lastly, monkeypox can be spread through contaminated linens or bedding. Transmission through respiratory secretions is uncommon but has been reported after prolonged face-to-face contact with symptomatic individuals. In addition, pregnant women can spread the virus to their fetuses through the placenta. Monkeypox Testing If you think you have monkeypox, contact your primary care physician or other medical providers to obtain testing. Notify the provider ahead of time before entering the physical office. Signs & Symptoms This current outbreak of West African monkeypox does not have the typical presentation of classic monkeypox. Symptoms usually appear one to three weeks after infection and include: Pimple-like rash or blisters on the face, inside the mouth, and on other areas of the body, like the hands, feet, chest, genitals, or anus. The rash will go through serval stages, including scabs, before healing and may be painful or itchy. Other symptoms of monkeypox can include: Fever Headache Muscle aches and backache Swollen lymph nodes Chills Exhaustion Respiratory symptoms such as sore throat, nasal congestion, or cough Symptoms of monkeypox may occur before or after a rash with some individuals only report experience a rash. Individuals with monkeypox are infectious once symptoms begin and remain infectious until lesions form scabs, scabs fall off, and a fresh layer of skin forms. The illness typically lasts 2-4 weeks.
-
RCP que salva vidas: ¿Están sus habilidades actualizadas?
If CPR (cardiopulmonary resuscitation) is performed in the first few minutes of cardiac arrest, a person’s chance of survival can double or even triple. Troy Wiedenbeck, MD, cardiologist with the Renown Institute for Heart & Vascular Health, explains how you can be ready to perform it in case of an emergency. According to the American Heart Association, over 350,000 out-of-hospital cardiac arrests occur in the U.S. This highlights the importance of CPR to everyone, not just medical personnel. Most people do not have heart trouble at a hospital or fire station, they have it going about their everyday lives. And when someone has a heart attack outside of a hospital, their survival often depends on receiving help from a bystander. Signs of Heart Trouble First, how do you know when someone is experiencing cardiac arrest? The signs and symptoms of cardiac arrest are immediate and drastic, including: Sudden collapse No pulse Not breathing Loss of consciousness And sometimes, patients can experience symptoms beforehand, such as fatigue, fainting, blackouts, dizziness, chest pain, shortness of breath or vomiting. CPR Change Many of us know CPR as both mouth-to-mouth and pumps to the chest, but the rule now is hands-only. Can you explain the change? Hands-only CPR is exactly what the name says -- it's CPR without mouth-to-mouth. The American Heart Association recommends using only your hands. So if you see someone suddenly collapse, it’s recommended to call 9-1-1 and push hard and fast in the center of their chest. Doing this will get blood flowing back to the brain, lungs and other organs for someone having heart problems. Performing CPR on Adults vs. Children Hands-only CPR is just as effective as mouth-to-mouth and chest compressions for teens and adults who may have gone into cardiac arrest. Remember, it’s important to act fast. First, call 9-1-1 and then start chest compressions right away. If you perform CPR on someone within the first few minutes, it can double or triple their chance of survival. Keep in mind, for infants and children younger than 12 years old, regular CPR with mouth-to-mouth, as well as chest compressions, is still recommended. Two Steps to Save a Life If you see a teen or adult suddenly collapse follow these two steps: Call 911 so care providers can begin to respond. When calling 911, be specific about your location, especially if you are calling from a cell phone. Knowing the street address, building, floor and closest entry point can save precious time for first responders. Answering the dispatcher’s questions will make sure help arrives fast, and at the correct location. Push hard and fast in the center of the chest. The goal during CPR is 100 to 120 compressions per minute, about the same tempo as the song “Stayin’ Alive,” or “Thriller.” For hand placement, it’s also important to put the heel of your hand on the center of their chest and place the other hand on top. Push down on their chest at least two inches. It may seem severe at the time, but pushing this hard can truly save a life. Continue performing compressions as long as possible. If you tire, have someone take over compressions, if possible, and take turns until medical help arrives. For information on a CPR course in Reno, please contact REMSA at 775-858-5700.
Read More About Life-Saving CPR: Are Your Skills up to Date?
-
Apoyo a la salud de la comunidad LGBTQ+: por qué es importante
Renown Health has long supported northern Nevada’s LGBTQ+ community Pride events with sponsorship, and we’ve collaborated with local and regional LGBTQ+ organizations as an ally. Renown’s Pride Committee works to deepen and broaden our external and internal efforts around LGBTQ+ community engagement, advocacy, and healthcare issues related to sexual and gender minorities, which is part of the greater Diversity, Equity and Inclusion efforts Renown is undertaking. According to Harvard Chan School, data shows that nearly a sixth of LGBTQ+ adults feel they were discriminated against based on their sexual orientation and gender identity. As a result, this brings to light the important need for education within the healthcare setting. Renown Health is bridging the gap for our LGBTQ+ population, and we know more work needs to take place in order to become an inclusive organization. Below are a few ways we’re working on improving our response to LGBTQ+ needs, and celebrate, respect and honor our diversity by being inclusive. Diversity, Equity and Inclusion The Diversity, Equity and Inclusion subcommittee was formed to heighten the awareness and develop a plan on how to better serve all of our diverse populations, including our LGBTQ+ patients. As the largest healthcare provider in northern Nevada, we knew that we could do a better job. The subcommittee provides us a forum to discuss ideas and develop plans to provide better care to these populations. Updated Medical Records with Preferred Name and Pronouns Of course healthcare is personal. We meet patients at their most vulnerable states. And relating to every person by the correct pronoun shows we respect their gender identity. A new medical records update supports our doctors, nurses and care team in capturing this vital information. We are now able to capture every person’s preferred name, sex and sexual orientation to better care for them. Kathleen Zaski BSN, RN, Manager of Clinical Informatics and IT Applications at Renown explains why this is so important. “Your name and identity are core to who you are as a person, and here at Renown, we aim to take care of you as a whole person and to provide the highest level of quality care to our community – all while ensuring the experience is exceptional and tailored to the individual. In other words, having the patient’s preferred name and pronoun in the medical record is important to validate their identity, and show we care, in an already high stress environment. Specifically, giving our providers easy access to the patients preferred name and pronoun in the medical record, allows them to properly address their health concerns. This also helps the health care provider foster a closer relationship with the patient. Studies have found this actually increases the quality of care by creating a more open and comfortable environment.” Gender Neutral Restrooms Mitch Harper, Senior Program Development Manager at Renown, recognizes there’s still so much more to improve upon in becoming an inclusive organization. “At the end of the day, it’s about creating a safe and welcoming environment for our community and our employees. Access to basic human services shouldn’t be contingent on an individual’s skin color, ethnicity, sex, gender identity, sexual orientation, age, disability, or beliefs. Ensuring that private restrooms are equally available to everyone on our campus is just one way we can provide a more inclusive, caring space for the people we serve.” Updated restroom locations: Roseview Tower: 10 Sierra Tower: 14 Tahoe Tower: 14 Helping to Lead and Influence Change Sean Savoy, Manager of Spiritual Care at Renown "The foundation of spiritual care is compassion – being with people in need by caring, supporting, and showing empathy, and promoting a sense of well-being. Being a member of the LGBTQ+ community informs that deep sense of compassion and empathy in a very special and unique way. Our human value, social validity, the very reality of who and what we are, even our right to exist, love and just be, are often called into question. This, in turn, can cause many of us to question ourselves and wonder about our self-worth. This experience should engender compassion and empathy so that we can better recognize, listen to and meet others’ needs to help them achieve inner peace, explore coping strategies to overcome obstacles during illness or crisis, and even find new balance by re-conceptualizing themselves in the context of health and illness. I have found that the intersectionality of my gay and spiritual selves has been a blessing in my life." Matthew Maloy, Team Lead Applications Specialist at Renown “I am a Team Lead Epic analyst in the IT department that is responsible for clinical based workflows for ED, Trauma, and Critical Care and have worked at Renown for 15 years. Being a part of the LGBTQ+ community influences my daily work by ensuring the Electronic Health Record reflects best practices such as giving clinicians the ability to document a preferred name, and displaying that throughout the medical record for consistency. Having the ability to influence decisions that move our community toward human value for all of us is a priority in my daily work.” Our Mission Renown Health’s mission is to make a genuine difference in the health and well-being of the people and communities we serve, including the LGBTQ+ community. We continue to build relationships to improve care, fostering better health outcomes for ALL of our patients by creating a more inclusive health system.
Read More About Supporting LGBTQ+ Community Health – Why it Matters
-
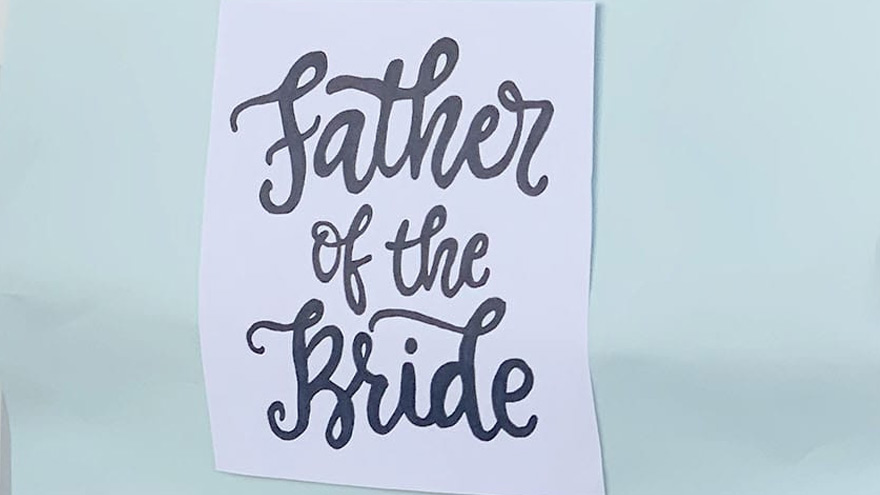
Cuidadores serviciales hacen realidad el sueño de una boda
A wedding is a big day for the wedding couple, but it’s also special for loved ones. A patient at Renown, Ken, got to take part in his daughter’s special day as her wedding plans changed to accommodate his medical condition. Grab some tissues and read how Renown’s team of compassionate caregivers and chaplains planned a wedding in Fianna’s Healing Garden. Ken was hospitalized at Renown Regional Medical Center where he was battling a lung problem – which was unrelated to COVID-19 – and his condition worsened rapidly on Wednesday, Aug. 12. His family made the decision to transition him to palliative care, which helps patients near the end of their lives remain comfortable, while supporting their dignity and quality of life. Ken’s medical condition altered wedding plans for his daughter, Chandra, and her fiancé, Tyler, who were planning to tie the knot later in 2020. Chandra wanted her father there, but knew he could not leave the hospital. That’s why Chandra’s sister, Heather, approached Ken’s care team with a request to have a small wedding ceremony at the hospital. Planning the Wedding A member of Ken’s care team, Amy Heston, registered nurse (RN), began planning how the wedding could be held outdoors in Fianna's Healing Garden in the E. L. Wiegand Pavilion, which was donated by the E. L. Wiegand Foundation. In 24 hours, Amy planned a wedding ceremony with the help of her colleague, Breyanna Aufiero, RN; the Renown Spiritual Care team; and nursing leaders on the coronary intensive care unit (ICU). Together, they decorated the aisle in the garden with flowers and battery-operated candles. They also made a sign for Ken’s hospital bed, which read, “Father of the Bride,” and crafted a bow tie for him to wear for the special occasion. With visitor restrictions in place at the hospital due to coronavirus (COVID-19), having the wedding outside in the Healing Garden allowed for more members of Ken’s family to attend including his wife, Charlotte, and his dog, Bella. Every step in planning the wedding required thoughtful and thorough care coordination so Ken could participate. His breathing was supported by oxygen and special arrangements were made to transport the oxygen tanks he needed to take part in his daughter’s wedding. Amy worked with respiratory technician, Kasey Benfield, and critical care technician, Ruben Duckworth, to ensure Ken’s oxygen needs were met using portable machines. Celebrating Love and Life Together Ken’s team of caregivers bathed him and shaved his face so he could look and feel his best for the ceremony. They put on his bow tie, covered his bed in decorations and his favorite blue, flannel blanket, and wheeled his bed outside for the ceremony. Renown associate chaplains Terri Domitrovich and Susan Palwick coordinated music and performed the ceremony for Chandra and Tyler on Thursday, Aug. 13, 2020. The bride and groom shared their first dance in the garden and Ken’s care team provided water and treats to give the family a full wedding experience. Shortly after the ceremony, Ken passed away. This wedding provided Ken and his family meaningful memories for their big life-changing moments as they celebrated and said goodbye. “Seeing Ken surrounded by family he never would have gotten to see again while in the hospital, watching him get to share a father-daughter dance with Chandra on her wedding day, and having him tell me that this day meant more to them than we would ever know were some of the most moving moments I’ve witnessed as a nurse,” Amy said. “I am so thankful for the team we have here. I know that this beautiful day wouldn’t have happened without the help of every single person who gave their time, money, creativity and passion to make it a day to remember.”
Read More About Helpful Caregivers Make a Wedding Dream Come True