Buscar
-
When Should You Consider Hospice? 5 Important Signs
Deciding on hospice care for a loved one is a deeply personal and challenging decision, balancing their wishes and medical realities. Rebecca Edwards, DNP, from Renown Hospice Care, explains the signs indicating when it might be time for hospice and offers guidance on navigating this decision with compassion and clarity. Understanding Hospice Care Before exploring the decision-making process, it’s crucial to have a clear understanding of what hospice means. Hospice care represents a shift in how we approach living with a terminal condition, emphasizing comfort, dignity, and quality of life above all else. When there is no longer a pathway to a cure, side effects of treatment outweigh the benefits, or someone is simply tired of frequent hospital visits, then it may be time for hospice. Hospice care is mainly done in the home, where most people wish to be. It's a compassionate, team approach to care that focuses on meeting the physical, emotional, and spiritual needs, supporting their families, and honoring individual preferences. 5 Critical Signs to Be Aware Of Decline in Overall Health: When a loved one's health continues to decline despite ongoing medical interventions, this may be a sign that these treatments are no longer effective. Increasing Pain and Symptoms: When managing symptoms such as pain, nausea, fatigue or shortness of breath becomes increasingly challenging, hospice can offer specialized support and expertise in symptom management. Frequent Hospitalizations: Repeated hospitalizations or emergency room visits can signify that the disease has progressed to a point where managing symptoms and providing comfort at home or in a hospice setting is a more appropriate approach. Difficulty with Daily Activities: If your loved one is experiencing difficult with activity of daily living such as dressing, bathing, or mobility, it may be a sign that they require additional support and assistance. Prognosis of Six to 12 Months: Hospice Care is typically recommended for patients with a prognosis of about one year or less if the disease follows its normal course. However, it’s important to remember that every individual is unique and prognosis can vary.
Read More About When Should You Consider Hospice? 5 Important Signs
-
Departamento destacado: Surgery & Procedure Scheduling
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
Perfect Peanut Butter and Pumpkin Puppy Treats
This holiday season, sprinkle some extra joy for your favorite furry pals by whipping up these easy, AKC-approved dog treats. With simple ingredients and quick baking times, they're the perfect last-minute surprise to show your pet some love. Turn it into a delightful gift by snagging some adorable, budget-friendly canisters (easily found at dollar or thrift stores) and fill them to the brim with these homemade goodies. It's a merry, tail-wagging gift that's sure to make this season the most pet-friendly one yet! 🎄🐾🍪
Read More About Perfect Peanut Butter and Pumpkin Puppy Treats
-
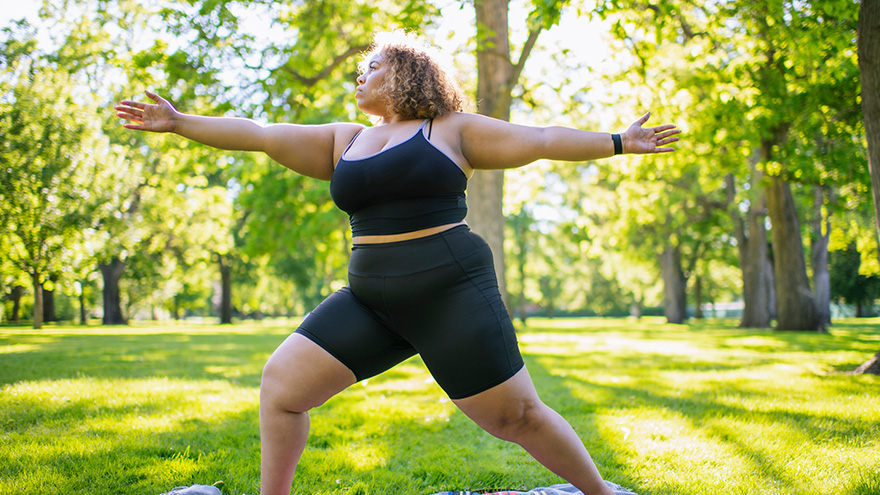
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Meet Raven: A Renown Therapy Dog
If you’ve ever spent time at Renown, you may have noticed there are some four-legged volunteers roaming the halls greeting patients, visitors, and staff. Since 1997, Renown has been fortunate enough to have its very own therapy dog program. As of today, there are 43 dogs in the program, and each of them have gone through countless hours of training to offer healing, comfort and support to those seeking treatment within our health system. Each of these therapy dogs have their own special personalities, but they all share the same mission: to make a paws-itive impact on everyone they meet. One therapy dog that has touched many lives at Renown is Raven, a five-year old Belgian Malinois mix. Raven's Story In March of 2019, Reno residents Richard and Vickie Lange rescued Raven from an animal shelter in Portola, California. When the Langes made Raven part of their family, they immediately started her in obedience training. After seeing her do so well, they thought of an idea that would not only help Raven reach her full potential but also allow them to give back to others – they decided to train Raven to be a therapy dog.
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
3 datos importantes de atención médica para la generación milenial
Many millennials are fortunate to have good health, but it’s important to be prepared for your next doctor’s visit. Here are three things that millennials should stay on top of for tracking and maintaining their health. For many millennials, doctor visits and preventive healthcare fall by the wayside. Alison Lynch, MD, a family medicine provider with Renown Medical Group says there are a few key things you can do now to set yourself up for a healthy future. 1. Establish with a Primary Care Provider Millennials are more likely to go to urgent care or consult the internet when a healthcare issue arises. While these are helpful tools, here’s a better one: a primary care provider. The benefit of establishing with a primary care provider is that your medical records, history and a baseline for your health will be documented. That means that when a problem or question comes up, your doctor will already have helpful information on file and can help you navigate your needs. Having a primary care provider is often required for prescription refills and referrals to a specialist. By establishing now, you’ll be able to get what you need in the future much faster. Make an Appointment Today 2. Protect Yourself and Your Community There are a few vaccinations and screenings that Dr. Lynch recommends for millennials. Flu Shots: These are available every year and are recommended for protecting not only yourself against the flu but also others you may come into contact with. Flu shots are usually available from August through December through your healthcare provider, pharmacies and pop-up events. Tetanus or Tdap: Most people receive a tetanus shot as a child, but it’s recommended that everyone get a booster every 10 years. If you are overdue, talk to your primary care provider or pharmacist about getting updated. Pap smear: If you’re a woman, a pap smear is recommended every three years in your 20s and every five years in your 30s. HPV vaccine: This vaccine helps prevent the virus that causes cervical cancer as well as the majority of head and neck cancers and warts. The HPV vaccine is recommended for all genders up until age 45. STD screening: Consider an STI/STD screening if you’re sexually active.
-
Getting to Know Renown's Canine Companions
A slobbery kiss, a wagging tail, a judgement-free smile. There are few things better than the love and attention of a canine companion. At Renown Health, we have a loyal and playful group of pet therapy teams. This volunteer program uses animal-assisted interactions (AAI) and animal-assisted therapy (AAT) to provide comfort, reduce boredom, increase social interactions, improve mood, boost general well-being and – perhaps most importantly – bring smiles to our patients’ faces. Benefits of AAT & AAI: Lowers blood pressure and heart rate by relieving anxiety Helps in pain management Eases feelings of depression, loneliness, boredom and isolation Stimulates communication Encourages physical activity For more information about the program, a complete list of our teams or to get involved, click here. Meet Keno and Linda Linda, Keno’s human, has volunteered as one-half of a therapy dog team for more than 14 years. Keno is her third Newfoundland, and he is a sweet and cuddly 2-year-old pup, who, according to Linds, thinks is a lap dog. “My mother was in assisted living for almost 10 years, and I saw what an impact a therapy dog can have,” Linda said. When she moved to Reno from Portland six years ago, she immediately contacted Renown. A Memory the Stands Out: A patient in the ICU was not responsive because of oxygen deprivation due to almost drowning. Linda and Keno went into the patient’s room at his physical therapist’s request, and the therapist asked the patient to reach out and pet the dog. After the third request, he moved his hand toward the dog, and his mother burst into tears. It was the first time the patient had moved since his accident. Linda and Keno went back several days in a row, and soon the patient was talking, sitting up and eating on his own. Meet Madi and Clark Madi, Clark’s human, is an employee at Renown, and Clark made it a family affair by joining the team in Sept. 2021. Clark is a unique pup with an amazing demeanor who adores everyone as much as they adore him. He is a hardworking Goldendoodle who loves to be a goofball at home when he’s off the clock. Why They Became a Therapy Dog Team: Madi was inspired to get Clark trained as a therapy dog because, as an employee at Renown, she was always so happy to see dogs walking around, and she knew that I wanted to provide that same relief to others. Her favorite thing about being a Renown volunteer is the joy it spreads to those working and the patients they are caring for. Meet Richard and Raven Raven is a four old Belgian Malinois who has been working as a therapy dog for two and a half years. She is calm, friendly and loves having her tummy rubbed. “The therapy dog teams are just one little part of Fighting the Good Fight,” Raven’s human Richard said. A Memory that Stands Out: Raven and Richard were assigned to the Sierra oncology ward one shift and visited a woman who had a picture of her dog displayed next to her bed. Raven immediately went to the bedside and the patient started petting her. As she spent more time petting Raven, Richard could see the stress disappearing from her face. He later learned that it was the patient’s first chemotherapy infusion, and Raven gave her the peace and the strength she needed to face the chemotherapy head-on. Meet Savannah and Hallie Hallie and Savannah’s journey as a therapy dog team began in 2017 at the Morgan Stanley Children’s Hospital in New York and has also taken them to San Francisco General Hospital and Stanford Hospital. The duo moved to Reno in 2020 and immediately joined the Renown Pet Therapy Program. A friend, energetic and cuddly American Cocker Spaniel, Hallie especially loves spending time with the young children at the hospital. A Memory That Stands Out: Savannah remembers one visit to a patient in the Children’s Emergency Room who was struggling with suicidal thoughts. Having struggled with mental health herself, Savannah felt a deep connection to the patient and a need to help. She recalls placing Hallie on the patient’s bed a seeing a “very small hint of a smile.” Savannah later learned that the Renown nurses hadn’t seen the patient smile in days. It was that moment that made Savannah realize what a profound impact Hallie can have on patients. Meet Chivas and Donna Chivas was a McNab/Border Collie mix who volunteered at Renown with her human Donna for two years. With help from Donna, Chivas was a master at reading situations in the hospital and reacting accordingly. For example, if a patient was afraid of dogs, she would sit with her back to the person so she didn’t come off as threatening. Contrarily, she would lie down on the floor when playing with young children to let them pet her on their level. Why They Became a Pet Therapy Team: This dynamic duo started out as a member of a local pet therapy group. During the height of the COVID-19 shutdown, they participated in outdoor pet therapy parades for various hospitals in the area. Donna and Chivas met Renown Volunteer Coordinator Wendy Peuket at one of the parades and she inspired Donna to pursue becoming a registered therapy dog team for Renown's Therapy Dog Program. Chivas sadly passed away unexpectedly in early December 2021, and the world is a whole lot dimmer place without Chivas’ light shining brightly.
-
Healthy Aging 5 Tips to Improve Happiness and Quality of Life
There are a few simple ways to encourage healthy aging that can translate to an improved quality of life. Here are some expert tips. What does healthy aging mean to you? If you’re like most people, you’re looking forward to removing the negative from your life — negative energy, thoughts, people and activities that don’t contribute to your best life. And while that’s a noble goal, too often we forget about ways to strengthen the positive parts of our lives. Expert Herbert “Buddy” Coard III, Ed.D, psychologist with Renown Behavioral Health, provides us with five positive behaviors to focus on to improve happiness and life satisfaction. Healthy Aging in 5 Easy Steps: 1. Connect – Make connections with friends, family, colleagues and neighbors. When you build strong connections, they can help enrich your life with new experiences and opportunities. Besides, having a support system to call upon when you need a favor is valuable as you age. 2. Be Active – Make time to get moving and work those muscles. Being active can include walking, practicing yoga, playing a game of pickleball or dancing. Exercise makes you feel good and keeps you health. Pick a physical activity that you enjoy, and don’t make excuses. Not only will being active help you build stronger muscles, it also helps you build strong connections with others. If you need a workout buddy, Meetup is a great resource to find like-minded people that share common exercise goals. 3. Take Notice – Be mindful and become more curious. Like a child, see the wonder and beauty of the world. Notice the things around you — the weather, the landscape, the mood and feelings of the people around you. By taking notice, it’s easier to learn to appreciate the things that matter. 4. Keep Learning – We never stop learning. Keep trying something new — a new course you’ve always wanted to try or a more challenging task someone has solicited for your help. Challenges keep us on our toes and increase our confidence and excitement in our day. OLLI (Osher Lifelong Learning Institute at the University of Nevada, Reno), brings diverse educational and social opportunities to active older adult learners (50+). EPIC (Educational Programs Inspiring the Community), offers a divers curriculum ranging from art classes to Accelerated training certificate courses. 5. Give – Be generous with your time, your knowledge and your talents by giving to friends, family and even strangers. Some easy ways to give is to show thankfulness, smile at people and volunteer. Sharing of yourself to a wider audience gives you a greater reward than just doing things for yourself. Nevada Volunteers Volunteer at Renown Health Practice these five tips to improve happiness and quality of life at any age.
Read More About Healthy Aging 5 Tips to Improve Happiness and Quality of Life
-
Cuidadores serviciales hacen realidad el sueño de una boda
A wedding is a big day for the wedding couple, but it’s also special for loved ones. A patient at Renown, Ken, got to take part in his daughter’s special day as her wedding plans changed to accommodate his medical condition. Grab some tissues and read how Renown’s team of compassionate caregivers and chaplains planned a wedding in Fianna’s Healing Garden. Ken was hospitalized at Renown Regional Medical Center where he was battling a lung problem – which was unrelated to COVID-19 – and his condition worsened rapidly on Wednesday, Aug. 12. His family made the decision to transition him to palliative care, which helps patients near the end of their lives remain comfortable, while supporting their dignity and quality of life. Ken’s medical condition altered wedding plans for his daughter, Chandra, and her fiancé, Tyler, who were planning to tie the knot later in 2020. Chandra wanted her father there, but knew he could not leave the hospital. That’s why Chandra’s sister, Heather, approached Ken’s care team with a request to have a small wedding ceremony at the hospital. Planning the Wedding A member of Ken’s care team, Amy Heston, registered nurse (RN), began planning how the wedding could be held outdoors in Fianna's Healing Garden in the E. L. Wiegand Pavilion, which was donated by the E. L. Wiegand Foundation. In 24 hours, Amy planned a wedding ceremony with the help of her colleague, Breyanna Aufiero, RN; the Renown Spiritual Care team; and nursing leaders on the coronary intensive care unit (ICU). Together, they decorated the aisle in the garden with flowers and battery-operated candles. They also made a sign for Ken’s hospital bed, which read, “Father of the Bride,” and crafted a bow tie for him to wear for the special occasion. With visitor restrictions in place at the hospital due to coronavirus (COVID-19), having the wedding outside in the Healing Garden allowed for more members of Ken’s family to attend including his wife, Charlotte, and his dog, Bella. Every step in planning the wedding required thoughtful and thorough care coordination so Ken could participate. His breathing was supported by oxygen and special arrangements were made to transport the oxygen tanks he needed to take part in his daughter’s wedding. Amy worked with respiratory technician, Kasey Benfield, and critical care technician, Ruben Duckworth, to ensure Ken’s oxygen needs were met using portable machines. Celebrating Love and Life Together Ken’s team of caregivers bathed him and shaved his face so he could look and feel his best for the ceremony. They put on his bow tie, covered his bed in decorations and his favorite blue, flannel blanket, and wheeled his bed outside for the ceremony. Renown associate chaplains Terri Domitrovich and Susan Palwick coordinated music and performed the ceremony for Chandra and Tyler on Thursday, Aug. 13, 2020. The bride and groom shared their first dance in the garden and Ken’s care team provided water and treats to give the family a full wedding experience. Shortly after the ceremony, Ken passed away. This wedding provided Ken and his family meaningful memories for their big life-changing moments as they celebrated and said goodbye. “Seeing Ken surrounded by family he never would have gotten to see again while in the hospital, watching him get to share a father-daughter dance with Chandra on her wedding day, and having him tell me that this day meant more to them than we would ever know were some of the most moving moments I’ve witnessed as a nurse,” Amy said. “I am so thankful for the team we have here. I know that this beautiful day wouldn’t have happened without the help of every single person who gave their time, money, creativity and passion to make it a day to remember.”
Read More About Helpful Caregivers Make a Wedding Dream Come True