Buscar
-
When Should You Consider Hospice? 5 Important Signs
Deciding on hospice care for a loved one is a deeply personal and challenging decision, balancing their wishes and medical realities. Rebecca Edwards, DNP, from Renown Hospice Care, explains the signs indicating when it might be time for hospice and offers guidance on navigating this decision with compassion and clarity. Understanding Hospice Care Before exploring the decision-making process, it’s crucial to have a clear understanding of what hospice means. Hospice care represents a shift in how we approach living with a terminal condition, emphasizing comfort, dignity, and quality of life above all else. When there is no longer a pathway to a cure, side effects of treatment outweigh the benefits, or someone is simply tired of frequent hospital visits, then it may be time for hospice. Hospice care is mainly done in the home, where most people wish to be. It's a compassionate, team approach to care that focuses on meeting the physical, emotional, and spiritual needs, supporting their families, and honoring individual preferences. 5 Critical Signs to Be Aware Of Decline in Overall Health: When a loved one's health continues to decline despite ongoing medical interventions, this may be a sign that these treatments are no longer effective. Increasing Pain and Symptoms: When managing symptoms such as pain, nausea, fatigue or shortness of breath becomes increasingly challenging, hospice can offer specialized support and expertise in symptom management. Frequent Hospitalizations: Repeated hospitalizations or emergency room visits can signify that the disease has progressed to a point where managing symptoms and providing comfort at home or in a hospice setting is a more appropriate approach. Difficulty with Daily Activities: If your loved one is experiencing difficult with activity of daily living such as dressing, bathing, or mobility, it may be a sign that they require additional support and assistance. Prognosis of Six to 12 Months: Hospice Care is typically recommended for patients with a prognosis of about one year or less if the disease follows its normal course. However, it’s important to remember that every individual is unique and prognosis can vary.
Read More About When Should You Consider Hospice? 5 Important Signs
-
Departamento destacado: Surgery & Procedure Scheduling
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
Department Spotlight Clinical Research
May 20 is National Clinical Trials Day. Celebrate with us by recognizing the Clinical Research team at Renown Health! The root of every medication, treatment and procedure in healthcare can be traced back to research. From the beginning of the history of medicine, research has always played a crucial role in improving the lives of patients around the world, leaving a permanent mark on how we expand our medical capabilities to this day. Renown Health’s Clinical Research team, in partnership with the University of Nevada, Reno School of Medicine (UNR Med), are leading that effort in our very own community. As our in-house leaders of clinical trials, this team is dedicated to advancing the science of medicine to help further our bottom line of making a genuine difference in the health and well-being of the patients they serve. Trial by (Medical) Jury Every day looks different for the Clinical Research team, especially when it comes to interacting with patients, providers and “sponsors,” which are the organizations providing the treatment for the study. One fact always remains true: communication and collaboration are key, especially among the team who act as the face of this process. Meet Lisa English (pictured above on the far right in a blue shirt), a Lead Clinical Research Coordinator at Renown who serves as the study "project manager." One aspect of Lisa’s day-to-day is seeing patients through their clinical trials from start to finish. It all begins with the setup. “Before we can launch a study, there is a lot of back-and-forth dialogue between everyone involved to ensure the best fit,” said Lisa. “Sponsors will come to us with novel treatments, such as medications or devices, and the inclusion criteria that patients need to meet in order to qualify for the study. We then immediately jump into working with the providers, looking closely at the science and comparing the treatments to what is on the market already.” From there, Lisa coordinates conversations between the providers, sponsors and study teams to gauge everyone’s capacity based on the length of the study, ensuring everyone involved has the time to dedicate to the process. Next, the providers identify patients that meet the criteria for the study, and together, the team decides where the patient visits will happen and discusses any potential barriers that may affect patient retention. The budget is clearly defined at this stage, set up to make sure no patient is ever billed for medical costs incurred as a result of the study. Often, research participants are seen within the specialty clinics throughout the health system, while other times the Clinical Research Coordinators see patients at the recently centralized Clinical Research Office at Renown Regional Medical Center. This location provides an essential public-facing space for the community to learn more about clinical trials and demonstrates the breadth of resources available at Renown to sponsors to strengthen external partnerships and research funding opportunities. Once the study officially begins, team members like Lisa will set patients up for a “screening/qualifying visit.” During this appointment, she makes sure patients get scheduled for their lab work, imaging scans and anything else the provider may need to make an executive decision on whether or not the patient is a good candidate for the study. “I build it all in Epic,” said Lisa. “The study information, directions, requirements and next steps are all loaded in Epic for easy tracking. We are also required to input any notes in the sponsor’s electronic data capture website. All the information I track is inputted without protected health information (PHI), so every patient is completely anonymous.” After the patient officially qualifies, the study goes full steam ahead. Team members like Lisa and the providers receive continual updates from sponsors on the status of the study. “Throughout the entire process, I make sure patients get scheduled for everything that meets the requirements for the study,” said Lisa. “I meet with patients one-on-one to discuss their needs and concerns and ask questions about the study, organize their appointments and charts and deal with any issues or pivots that may arise. It’s very important that every patient fully understands what is going to happen with their care.” The Clinical Research department strives to serve as a care partner to patients, providers and clinics they work with. The majority of our Clinical Research Coordinators are trained phlebotomists and medical assistants, performing their own assessments such as lab draws and electrocardiograms (ECGs) to streamline the research visit process and reduce resource constraints on the clinics and health system. Lisa typically sees a couple of patients per week, depending on the study and where patients are in the cycle. Depending on the complexity of the trial, patients may see the research team only one time or several times over many years. Typically, clinical trial patients are seen in clinic every 2-4 weeks. There are many tasks required before, during and after a research visit to ensure everything runs smoothly, so Clinical Research Coordinators dedicate an average of 5-11 hours of work per patient, per visit. Regardless of patient load, each employee in the Clinical Research department – as well as participating teams across Renown and UNR Med – always step in to help each other out. According to Lisa, the environment is immensely supportive. “We have a program here at Renown to train employees who have never done clinical trials,” said Lisa. “We love seeing people get more engaged with the important work we do, and every department has been great at collaborating with us. Everyone brings a different perspective.” At the end of the study, Lisa gathers all the information and collects notes into a zip drive or paper binder for archiving. The sponsor lets the Clinical Research team, providers and patients know whether they are on the trial drug or on the placebo. The teams use the data gathered during the study to publish a report or present at conferences, promoting the critical research done to better the lives of patients in our community, and potentially, the world. “I appreciate the time everyone gives us to make sure our research is successful,” said Lisa. “It feels great to work together to make a difference, improve healthcare quality and save lives.” Behind-the-Scenes, Yet on the Frontlines The impact of research studies transcends hospital walls, and this can all be attributed to the dedication of our Clinical Research department. The constant collaboration between this team, lab science, medical assistants and providers, cardiology technologists, sonographers, finance teams and our partners at UNR Med is crucial to safeguarding the success of the studies. Devoted to keeping research close to home, Renown and UNR Med teamed up to form the Clinical Research Office (CRO) in 2021. With the strength of northern Nevada's largest not-for-profit health system and Nevada’s first medical school, this team is dedicated to giving our community access to the latest care innovations. “At UNR Med, we are working with students, residents and academic faculty; on the Renown side, we are working with clinicians and community participants,” said Amber Emerson, Manager for Community Outreach and Research Engagement for UNR Med. “Everything we do is data-driven,” added Kristen Gurnea, Manager of Clinical Research for Renown. “Our main goal is to optimize our impact and provide a community benefit for our patients. The scope of our roles in the Clinical Research office is very diverse.” To help meet the growing need locally for healthcare and cutting-edge treatment solutions, the CRO has continued to grow, expanding its research capabilities and helping bring new medications, medical devices and more to patients across northern Nevada and northeastern California. “Once upon a time, our team had only six members; today we have grown to a team of 25,” added Diana Torres, Research Resource Analyst for Renown. “We used to be considered one department, including Medical Education, and we have since branched off into our own cost center. We branched off even further and created a separate Genetics department that runs the Healthy Nevada Project. Throughout this process, the Clinical Research department was always the main point of the umbrella.” “We participate in hospital-wide outreach and marketing, and we feel this has really helped us get the word out about our department,” added Raul Arellano, Research Resource Analyst for Renown. “In fact, we doubled our clinical trial portfolio from last year.” The CRO currently operates over 100 clinical trials locally in cardiology, endocrinology, infectious disease, neurology, pediatric and adult oncology, pediatric sub-specialties and pulmonology. Behind the curtains of in-person research, the CRO is home to several experts who help turn our research studies into a reality, from budgeting and billing to barrier-breaking and building relationships. “I help with barriers patients and Clinical Research Coordinators are facing, building connections and relationships inside and outside of our health system,” said Kristen Gurnea. “I enjoy handling all the supporting pieces that are required for studies to happen.” “My role changes every day,” added Jenna Berger, Administrative Assistant for the CRO at Renown. “Some days, I’ll be helping coordinate patient stipends and going through document management to ensure we have all necessary signatures. Other days, I will be planning events – like Clinical Trials Week – for our department and creating marketing materials and fliers.” “Our day-to-day involves going over anything related to research financials,” added Diana Torres. “We handle sponsor billings, process efficiency and collecting revenue for research contracts, and we collaborate closely with our Finance department and Revenue Integrity in order to accomplish this. It’s important for us to make sure all billing on both the sponsor and patient side is taken care of, especially because patients should never receive a bill for medical services they receive for the trial. A year and a half ago, we started doing budget negotiations for research contracts,” said Diana Torres. “We are proud to help clinical teams with any training they may need on these negotiations as well as billing reviews and allocations.” Seeing patients progress during a study and transform before their eyes inspires the CRO team to continue doing what they do every day. “I’ve been here for many years, first working on the floor as an oncology nurse and transitioning to oncology research in 2005,” said Anna Winchell, Cancer Protocol Nurse for Renown. “I love getting to know the patients and seeing them progress into a healthy lifestyle.” Medical students and residents at UNR Med also play a significant role in the research process, advancing medicine by exploring causes and novel treatments for a wide range of conditions, including HIV, muscular dystrophy, gastrointestinal disorders, infectious diseases and more. Medical research at UNR Med is headed by committed research coordinators, community outreach managers, grants managers, pharmacists and physicians. “I oversee scientific review and help the physicians that come to us for those resources,” said Amil Trujillo-King, Medical Research Coordinator at UNR Med. “I guide medical students in their research protocols and help with different projects to improve research activities for both students and medical residents.” It takes a village to make clinical research happen. Because of that, the ACRO cannot thank the following teams enough for moving mountains for the future of medicine: Renown Health and UNR Med leadership for demonstrating the integrated health system’s commitment to expanding access to clinical research in our community within both the Renown / UNR Med affiliation and Renown active strategic plans. Renown Pharmacy especially Research Clinical Pharmacist Tim Morton, who supports all clinical trial medication dispensing and patient education across all clinical trials at Renown. Accounts Payable for having a huge impact on patient and employee reimbursement. Renown Medical Group for their participating providers, especially in oncology, cardiology, pulmonology, pediatrics, endocrinology and neurology, who are involved in research year after year. Marketing and Communications for helping with printed materials and raising awareness for clinical research at Renown and UNR Med. An Affiliation to Last Through the Ages A collective, shared vision of exploring community health – that is the impetus behind the affiliation between Renown and UNR Med. By leveraging resources across both institutions, the CRO has maximized their impact, giving the people of northern Nevada greater access to new interventions and treatments and promoting an impassioned culture with patients, providers, residents and medical students. “Community-based research always sat well with me,” said Amber Emerson. “As Renown and UNR Med, we have this unique opportunity to shape clinical research here in northern Nevada. We always make sure we present research in a meaningful way that speaks to the work we produce and demonstrates the opportunities we offer. After all, participating in clinical research doesn’t mean our patients are ‘guinea pigs’ – quite the opposite! They are partners in their health care, and we support them through providing access to novel treatments.” “Research is my passion, and my career has spanned broadly from grants administration to study coordination,” added Valerie Smith, Clinical Research Center Administrative Manager at UNR Med. “I am excited to be at the forefront of research frontiers in northern Nevada.” Through robust engagement and collaboration with healthcare providers, department administrators, internal research team members and leadership, the strength of this affiliation is unmeasurable. The CRO’s ultimate goal is to have clinical trials be the standard of care for every condition that Renown and UNR Med treats. Clinical research participation is all about patient autonomy, shared decision-making between patients and their providers and advancing medicine to save lives. From their beginnings as a small group of passionate researchers to their present reality as a leader in the research space in northern Nevada, their efforts do not go unnoticed. “The success of our department is inspiring,” said Amil Trujillo-King. “Renown and UNR Med supports the wellbeing of all employees and contributes directly to the growth of the department.” “When I first joined Renown in Patient Access, I didn’t realize that we had a research department; with a strong healthcare background in my family, I knew I wanted to grow in my career, and our expanding Clinical Research office was that next step,” said Raul Arellano. “With our affiliation with UNR Med, it’s especially inspiring to be able to apply what I learned as a Patient Access Representative to help further outcomes for our patients through managing our finances.” Through their unwavering commitment to research excellence and patient-centered care, the CRO will continue to pave the way for groundbreaking medical discoveries and improved outcomes for patients for years to come. “Fundamentally, we’re working to build a culture of research in our community because we believe it is the right thing to do. Our community deserves to have access to clinical trials and novel care close to home with a dedicated team to support them every step of the way,” closes Kristen Gurnea.
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
3 datos importantes de atención médica para la generación milenial
Many millennials are fortunate to have good health, but it’s important to be prepared for your next doctor’s visit. Here are three things that millennials should stay on top of for tracking and maintaining their health. For many millennials, doctor visits and preventive healthcare fall by the wayside. Alison Lynch, MD, a family medicine provider with Renown Medical Group says there are a few key things you can do now to set yourself up for a healthy future. 1. Establish with a Primary Care Provider Millennials are more likely to go to urgent care or consult the internet when a healthcare issue arises. While these are helpful tools, here’s a better one: a primary care provider. The benefit of establishing with a primary care provider is that your medical records, history and a baseline for your health will be documented. That means that when a problem or question comes up, your doctor will already have helpful information on file and can help you navigate your needs. Having a primary care provider is often required for prescription refills and referrals to a specialist. By establishing now, you’ll be able to get what you need in the future much faster. Make an Appointment Today 2. Protect Yourself and Your Community There are a few vaccinations and screenings that Dr. Lynch recommends for millennials. Flu Shots: These are available every year and are recommended for protecting not only yourself against the flu but also others you may come into contact with. Flu shots are usually available from August through December through your healthcare provider, pharmacies and pop-up events. Tetanus or Tdap: Most people receive a tetanus shot as a child, but it’s recommended that everyone get a booster every 10 years. If you are overdue, talk to your primary care provider or pharmacist about getting updated. Pap smear: If you’re a woman, a pap smear is recommended every three years in your 20s and every five years in your 30s. HPV vaccine: This vaccine helps prevent the virus that causes cervical cancer as well as the majority of head and neck cancers and warts. The HPV vaccine is recommended for all genders up until age 45. STD screening: Consider an STI/STD screening if you’re sexually active.
-
Celebrating Renown Health's Nursing Excellence Conference
Renown Health recently wrapped up the twentieth annual Nursing Excellence and Excellence in Critical Care Conferences, the conference theme was the Courageous Calling and over 400 nurses from specialty fields across the region attended to learn, reflect, build relationships and obtain continuing education units (CEUs). Celebrating The Courageous Calling During the first day of the Nursing Excellence Conference, local and national leaders presented topics including redefining resilience, documentation liability, transgender healthcare and caring for the homeless population. Among the list of impressive speakers were Chief Nurse Executive at Renown Health, Melodie Osborn, and Nora McInerny, writer and host of the "Terrible Thanks for Asking" podcast. On day two,speakers focused on the critical care specialties within nursing, including intensive care, emergency room, pediatric intensive care and neonatal intensive care. Topics covered included post-COVID-19 pulmonology with Dr. Graham, traumatic brain injuries with Dr. Demers, COVID-19 reflections with Anicia Beckwith, a discussion about "Mis C” with Dr. Healy, innovations in imaging with Dr. Rangaswamy and cardiology with Dr. Danaf. Thank you to our sponsors and raffle donors for making this event possible: Erik Olson and Larry Duncan, Jana Elliott, Melodie Osborn, Becky Haase, Lori Tuntland, Dr. Akbar, Dr. Lous, Mel Morris, Grand Sierra Resort, Renown Health Gift Shops, Renown Health Directors of Nursing, Renown Health Marketing & Communications Department, Renown Health Dermatology, Laser, & Skin Care and Renown Health Foundation. Learn more about finding purpose in the health of our community when working at Renown Health here.
Read More About Celebrating Renown Health's Nursing Excellence Conference
-
Renown Regional Medical Center Recognized Among Nations Top Hospitals In Critical Care
The region’s only trauma center receives top honors from Healthgrades What is Healthgrades? Healthgrades, a leading national resource for trusted information about physicians and hospitals, recently announced the recipients of their 2021 Specialty Excellence Awards. These awards recognize hospitals with superior performance and have selected Renown Regional Medical Center in Reno, Nv. as northern Nevada’s top hospital for critical care. Hospitals in this ranking demonstrate excellent patient clinical outcomes in treating pulmonary embolism, respiratory system failure, sepsis, and diabetic emergencies. Health grades further distinguishes hospitals that stand out as America’s 100 Best Hospitals for Specialty Care™, with Renown Regional Medical Center identified as Nevada’s only critical care hospital to be bestowed with this honor. What this Award Means To Us “At Renown, I am honored to work beside dedicated healthcare heroes who are working tirelessly to make a genuine difference in the health and well-being of every patient and family we serve,” says Tony Slonim, MD, D.Ph., FACHE, president and CEO of Renown. “Having trained and served as a pediatric intensive care physician, this honor from Healthgrades does so much to recognize the compassion, skill, and determination of this incredible team. I join with our community in saluting the Renown Regional Medical Center’s critical care team as one of the best critical care hospitals in the nation.” “As the only accredited trauma center between Sacramento and Salt Lake City, we receive and care for critically-injured patients from over 100,000 square miles. Our communities depend on Renown Regional Medical Center for outstanding critical care,” says Dawn D. Ahner, DSc, FACHE, Chief Operating Officer, Acute Services. “Our multi-disciplinary critical care and intensive care healthcare teams are specially-staffed, equipped and designed to care for, closely monitor, and comprehensively care for patients with life-threatening conditions.” “Having a specialty-trained team of physicians, nurses, respiratory therapists, care managers, physical and occupational therapists around the clock, every day ensures that, no matter the illness or injury, a patient will be treated with the highest degree of care right away,” says Paul Sierzenski, MD, MSHQS, CPE, FACEP, Chief Medical Officer, Acute Services. “What it comes down to is this; the quicker and more accurately you get treated, the better your outcome will be. That's what makes being one of the most respected critical care teams in the country, so vital to all of us.” “At Renown, we have done so much over the years, to prepare to meet the need for rapid surges in critically ill or injured patients. Through this pandemic, many patients suffering from complications of COVID-19 have needed intensive care services,” says Erik Olson, MHA, Chief Executive Officer of Renown Regional Medical Center. “As the demand for critical care and intensive care continues to increase, the ratio of ICU beds to hospital beds will continue to rise as the ICU occupies an ever-larger role at the center of acute hospital care. We appreciate the recognition from Healthgrades demonstrating the Renown team’s unwavering commitment to the highest level of patient care and safety.” About Renown Health Renown Health is the region’s largest, locally owned and governed, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe, and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination, and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group, an urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health. Renown’s institute model addresses social determinants of health and includes Child Health, Behavioral Health & Addiction, Healthy Aging, and Health Innovation. Clinical institutes include Cancer, Heart, and Vascular Heath, Neurosciences, and Robotic Surgery. Renown is currently enrolling participants in the world’s largest community-based genetic population health study, the Healthy Nevada Project®. For more information, visit renown.org. About Healthgrades Healthgrades is dedicated to empowering stronger and more meaningful connections between patients and their healthcare providers. At Healthgrades, we help millions of consumers each month find and schedule appointments with their provider of choice. With our scheduling solutions and advanced analytics applications, we help our health system and life sciences clients cultivate new patient relationships, improve patient access, and build customer loyalty. At Healthgrades, better health gets a head start.
-
Renown Neuro Diagnostic Laboratory Nationally Recognized
Earning its third five-year accreditation, Renown’s neuro-diagnostic lab remains Nevada’s only accredited ABRET facility. The Renown Institute for Neurosciences is pleased to announce that the neuro-diagnostic lab at Renown Regional Medical Center has been re-accredited by the American Board of Registration of Electroencephalographic and Evoked Potential Technologists (ABRET). ABRET’s lab accreditation process evaluates technical standards, the quality of a laboratory’s output, and lab management. “Renown Health is a leader and a destination for health in treating neurological disorders and advancing innovations in neurology. The specialists at the Renown Institute for Neurosciences provide comprehensive brain, nerve and surgical support along with a full range of diagnostic and additional procedures and a disease-specific, patient-focused approach to care,” says Tony Slonim, MD, DrPH, FACHE, President and CEO, Renown Health. “This prestigious honor from ABRET means Renown’s Electroencephalogram (EEG) Laboratory has met strict standards and is recognized as a place where patients and physicians can confidently receive quality diagnostics.” “In addition to re-accreditation from ABRET, the Institute for Neurosciences has earned a Gold Seal of Approval by the Joint Commission and offers advanced treatment options including t-PA (Tissue Plasminogen Activator) and biplane angiography. The Level III accredited Epilepsy laboratory implements some of the newest treatments available,” said Renown’s Chief Medical Officer, Paul Sierzenski, MD, MSHQS, CPE, FACEP. “Renown patients also have access to the most promising new therapies through national clinical trials, which have been shown to significantly improve patients’ health and well-being.” “I am proud to recognize our dedicated team of caregivers for their continued passion and excellence in maintaining the highest standards in patient care,” said Renown Institute for Neurosciences’ Division Chief, Dr. Rolando Ania. “It is all thanks to their tremendous efforts that we remain the only ABRET accredited laboratory, as well as the only nationally accredited epilepsy center (NAEC Level III), in the state of Nevada.” Using a collaborative approach, specialists at the Renown Institute for Neurosciences use leading-edge diagnostic tools to identify neurological conditions and treat patients with the most effective techniques available. What is a Neuro-diagnostic Lab? A neuro-diagnostic lab allows care teams the technology to evaluate how a patient’s peripheral, autonomic, and central nervous systems function, and aid in diagnosing and treating conditions such as epilepsy, multiple sclerosis, Parkinson’s disease, stroke, and other diseases of the nervous system. What is an Electroencephalogram (EEG)? An Electroencephalogram (EEG) is a test that measures and records the electrical activity of the brain. During the test, special sensors called electrodes are attached to the patient’s head and hooked by wires to a computer. The computer then records the brain’s electrical activity on the screen. Using a collaborative approach, specialists at the Renown Institute for Neurosciences use leading-edge diagnostic tools to identify neurological conditions and treat patients with the most effective techniques available. Renown Health hospitals are ranked as Nevada’s top hospitals by U.S. News & World Report.
Read More About Renown Neuro Diagnostic Laboratory Nationally Recognized
-
Thomas S Dolan Pulmonary Rehabilitation Program
The program becomes first of its kind to be accredited in Nevada Renown Health is pleased to announce the certification of the Thomas S. Dolan Pulmonary Rehabilitation program at Renown South Meadows Medical Center by the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). AACVPR certification demonstrates that an organization's Pulmonary Rehabilitation Program is aligned with current guidelines set by the American Association of Cardiovascular and Pulmonary Rehabilitation for appropriate and effective early outpatient care of patients with cardiac or pulmonary issues. Certification offers peace of mind, so that patients can feel confident in knowing that staff has the experience and skills necessary to coordinate the many issues faced by people receiving a life-changing cardiac or pulmonary diagnosis. Pulmonary rehabilitation programs help people with health issues such as asthma, chronic bronchitis, pulmonary fibrosis, or chronic obstructive pulmonary disease (COPD) recover faster and live healthier. “Having access to quality pulmonary rehabilitation services so close to home, staffed by a highly skilled group of compassionate care providers, truly is a gift to our community,” said Tony Slonim,MD, D.Ph., president and CEO of Renown. “We are extremely proud of the work being done in our pulmonary rehabilitation program, and also forever grateful for Tom Dolan’s donation to the program in 2019, which empowers Nevadans to improve both their health and quality of life.” “Thomas S. Dolan Pulmonary Rehabilitation is the only accredited pulmonary rehabilitation program in the state of Nevada,” said Renown South Meadows Medical Center and Rehabilitation Hospital Vice President Chris Nicholas. “We take pride in this distinguished honor from the AACVPR as it acknowledges and amplifies the life-changing work happening here. Our dedicated caregivers provide support to our patients every step of the way, helping them lead vibrant and fulfilling lives despite their health conditions.” The comprehensive pulmonary rehabilitation program at Renown South Meadows Medical Center offers treadmills, stationary bicycles, strength training and an education classroom to help patients achieve health goals. To earn accreditation, Renown’s pulmonary rehabilitation program participated in an application process requiring extensive documentation of the program’s practices. AACVPR Program Certification is the only peer-review accreditation process designed to review individual programs for adherence to standards and guidelines developed and published by AACVPR and other related professional societies. In November 2019, Tom Dolan, owner and founder of Dolan Auto Group, donated to the Pulmonary Rehabilitation at Renown South Meadows Medical Center after his personal experience thriving in pulmonary rehabilitation brought northern Nevada’s capabilities, and needs to his attention. His generous donation has allowed Renown to double the number of patients who receive treatment and increase the access to pulmonary rehab in our community. “As a former patient myself, I found so much benefit in my pulmonary rehab,” said Dolan. “I have always wanted to support this program and increase the number of people it serves. It’s great to see that we now have the only certified pulmonary rehab in Nevada. “The most essential component of lung health is breaking the cycle of inactivity associated with lung disease,” said Lung Critical Care Physician Dr. Farah Madhani-Lovely. “Our community is fortunate to have an accredited program like this to empower our patients.” About AACVPR Founded in 1985, the American Association of Cardiovascular and Pulmonary Rehabilitation is a multidisciplinary organization dedicated to the mission of reducing morbidity, mortality and disability from cardiovascular and pulmonary disease through education, prevention, rehabilitation, research and disease management. Central to the core mission is improving the quality of life for patients and their families. Learn more about AACVPR at www.aacvpr.org.
Read More About Thomas S Dolan Pulmonary Rehabilitation Program
-
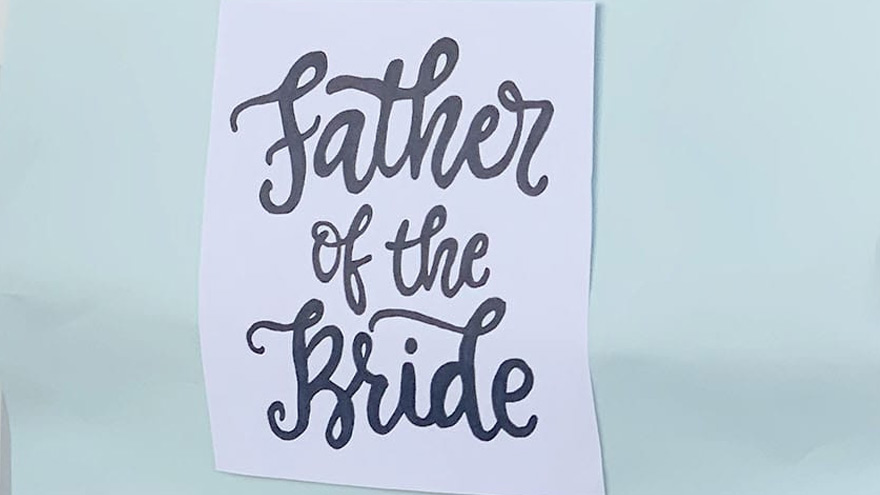
Cuidadores serviciales hacen realidad el sueño de una boda
A wedding is a big day for the wedding couple, but it’s also special for loved ones. A patient at Renown, Ken, got to take part in his daughter’s special day as her wedding plans changed to accommodate his medical condition. Grab some tissues and read how Renown’s team of compassionate caregivers and chaplains planned a wedding in Fianna’s Healing Garden. Ken was hospitalized at Renown Regional Medical Center where he was battling a lung problem – which was unrelated to COVID-19 – and his condition worsened rapidly on Wednesday, Aug. 12. His family made the decision to transition him to palliative care, which helps patients near the end of their lives remain comfortable, while supporting their dignity and quality of life. Ken’s medical condition altered wedding plans for his daughter, Chandra, and her fiancé, Tyler, who were planning to tie the knot later in 2020. Chandra wanted her father there, but knew he could not leave the hospital. That’s why Chandra’s sister, Heather, approached Ken’s care team with a request to have a small wedding ceremony at the hospital. Planning the Wedding A member of Ken’s care team, Amy Heston, registered nurse (RN), began planning how the wedding could be held outdoors in Fianna's Healing Garden in the E. L. Wiegand Pavilion, which was donated by the E. L. Wiegand Foundation. In 24 hours, Amy planned a wedding ceremony with the help of her colleague, Breyanna Aufiero, RN; the Renown Spiritual Care team; and nursing leaders on the coronary intensive care unit (ICU). Together, they decorated the aisle in the garden with flowers and battery-operated candles. They also made a sign for Ken’s hospital bed, which read, “Father of the Bride,” and crafted a bow tie for him to wear for the special occasion. With visitor restrictions in place at the hospital due to coronavirus (COVID-19), having the wedding outside in the Healing Garden allowed for more members of Ken’s family to attend including his wife, Charlotte, and his dog, Bella. Every step in planning the wedding required thoughtful and thorough care coordination so Ken could participate. His breathing was supported by oxygen and special arrangements were made to transport the oxygen tanks he needed to take part in his daughter’s wedding. Amy worked with respiratory technician, Kasey Benfield, and critical care technician, Ruben Duckworth, to ensure Ken’s oxygen needs were met using portable machines. Celebrating Love and Life Together Ken’s team of caregivers bathed him and shaved his face so he could look and feel his best for the ceremony. They put on his bow tie, covered his bed in decorations and his favorite blue, flannel blanket, and wheeled his bed outside for the ceremony. Renown associate chaplains Terri Domitrovich and Susan Palwick coordinated music and performed the ceremony for Chandra and Tyler on Thursday, Aug. 13, 2020. The bride and groom shared their first dance in the garden and Ken’s care team provided water and treats to give the family a full wedding experience. Shortly after the ceremony, Ken passed away. This wedding provided Ken and his family meaningful memories for their big life-changing moments as they celebrated and said goodbye. “Seeing Ken surrounded by family he never would have gotten to see again while in the hospital, watching him get to share a father-daughter dance with Chandra on her wedding day, and having him tell me that this day meant more to them than we would ever know were some of the most moving moments I’ve witnessed as a nurse,” Amy said. “I am so thankful for the team we have here. I know that this beautiful day wouldn’t have happened without the help of every single person who gave their time, money, creativity and passion to make it a day to remember.”
Read More About Helpful Caregivers Make a Wedding Dream Come True
-
South Meadows Medical Center Named Number 1 Hospital
U.S. News & World Report recently released their 2020-21 Best Hospitals rankings naming Renown South Meadows Medical Center as the number one hospital in Nevada. U.S. News looked at 4,554 hospitals, which represent nearly all U.S. facilities providing inpatient care. Hospitals are evaluated across a wide range of conditions and procedures, including 16 medical specialty areas of care. “We are committed to be among the best in the nation for quality, safety and patient experience,” said Tony Slonim, MD, D.Ph., FACHE, president and CEO of Renown. “This ranking confirms what Renown has always been dedicated to — providing the best patient care possible. Quality and safety are the responsibility of every employee and physician at Renown, and we are proud that Renown South Meadows has been chosen as the best in the state and among the best in the nation.” “We thank the incredible physicians, nurses and employees at Renown South Meadows Medical Center and across Renown for their dedication to excellent patient care – our employees, patients and our community are the true award winners,” said Chris Nicholas, Vice President & Administrator, Renown South Meadows & Renown Rehabilitation Hospital. “We applaud them as being not only the best in the state, but among the best in the nation.” “We are proud that Renown South Meadows is one of Nevada’s highest rated hospitals, and it’s exciting to have that recognition. Over the last year both our acute care hospitals – South Meadows and Renown Regional Medical Center, have made substantial improvements. We are working every day to ensure we are delivering the highest quality, safest care to our patients and our community,” said Dawn D. Ahner, DSc, FACHE, Chief Operating Officer — Acute Services for Renown. Renown South Meadows has been recognized by several national organizations for excellence and quality, including the Joint Commission, Leapfrog and Health Insight. Renown South Meadows Medical Center is an Accredited Chest Pain Center, and a Pathway Designated hospital for nursing excellence. Renown South Meadows provides an emergency department staffed 24/7 with board-certified emergency physicians, a wide range of services including primary and urgent care medical offices, a lab and health improvement programs. Renown is currently recruiting outstanding employees at https://careers.renown.org/.
Read More About South Meadows Medical Center Named Number 1 Hospital