Buscar
-
Departamento destacado: Surgery & Procedure Scheduling
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
Departamento destacado: Children’s Infusion Services
Help us celebrate the holiday season by sharing joy with our Children’s Infusion Services team! Thinking about blood can make any of us squeamish, and seeing it can be even more intimidating to the children in our lives. Being treated for a condition that requires blood transfusions or chemotherapy infusions is no easy feat, especially during the holiday season. This time of year, we are proud that we can offer our pediatric patients the power of proximity and excellence by having access to high level care close to home. The Children’s Infusion Services (CIS) department at Renown Children’s Hospital is committed to bringing the gift of quality care to our community’s youngest patients. Whether they are caring for a child with a blood disorder or giving expert infusion care for a child battling cancer, no team does what they do better than these expert nurses, medical assistants, intake coordinators and physicians. ‘Tis the Season to Bring Hope As the only pediatric oncology and hematology program in the region, the CIS department has a lot of responsibility on their shoulders. From inpatient chemotherapy to outpatient infusion services, this team treats a long list of pediatric blood conditions including: Pediatric cancers Anemias Immune-mediated blood disorders Sickle-cell disease Bone marrow failure syndromes Bleeding disorders “Our team provides a large variety of services from labs draws, sedations for procedures, infusions for diagnoses such as Crohn's disease, blood transfusions, as well as chemotherapy,” said Jen Torres, RN. “Our team works extremely well together. We try to go above and beyond for our patients every day. It may be something as simple as a hug to comfort a parent or a special birthday gift for a patient.” “My job allows me to work with several departments and providers when coordinating care for our littlest of patients,” added Jane Strawn, Intake Coordinator. “I assure proper authorizations are in place for the care that is needed, I communicate with our families when scheduling appointments, I organize End of Treatment Celebrations, as well as birthday shout outs and work closely with our Child Life team to help make the challenging appointment little easier.” To best serve their patients, the team thrives on being expert multitaskers. Central line care, chemotherapy administration, blood transfusions, medication management, preventative injections, lab draws, lumbar punctures, biopsies, imaging – you name it, they do it. And they do it all with the utmost focus on safety and support. “Our days have a lot of variation, as we perform a number of different services,” said Meagan Bertotti, RN. “We provide infusions for patients with chronic or acute medical conditions and chemotherapy/biotherapy treatment to patients undergoing cancer treatments. Overall, though, we work as a team to make these difficult procedures and treatments as easy as possible for the patients and families by providing engagement and support.” “While we handle a lot of chemotherapy treatments for pediatric patients, we also do other infusions and transfusions as well such as blood and platelet transfusions, enzyme replacement therapies, different types of injections such as Rabies vaccine or Synagis for high-risk babies who need that extra protection during the RSV season, and lab draws,” said Chelsea Angues, RN. “We care for patients that get their therapies from outside hospitals, but the patient lives within the Reno area. We receive orders from those outside hospitals to care for those patients, so they can still be with their families and not have to travel.” As members of the Children’s Oncology Group, a highly-regarded clinical trials group where over 90% of pediatric cancer patients across the U.S. receive treatment, teams like CIS in Renown Children’s Hospital deliver the highest standard of care. This partnership is a true testament to the devoted collaboration and relationship-building this team commits to on behalf of their patients every day. "One of the biggest accomplishments of our team is the fact that we became a member of the Children’s Oncology Group, and the Children's Infusion Center and Pediatric Oncology became one unit,” said Shelby Nolte. "Instead of being a clinic on one side and an infusion center on the other, we really came together to make it a whole unit that collaborates on almost everything.” “We've put much time into trying to understand other departments, their flow, their rationales and their processes so we can come to a solution that benefits our patients the greatest,” added Tiffany Macie, RN. “We've taken the last few years to really build our relationships with our pharmacy staff, our lab staff and our central supply resources. Our relationship building extends beyond the walls of the Renown building as well and out to the community providers too. In the past few years, we've been able to build relationships with the providers in the community where they trust they can send us their patients for treatment and lab draws. Finally, we've spent much time working on the relationships as a team. It's emotional work we do on our unit, and these families become our family. It's important to us that we take the time to be together outside of our shifts to enjoy one another and laugh!” In the compassionate realm of pediatric healthcare, CIS knows that the complexities of a cancer or blood disorder diagnosis can take an emotional toll on their patients and families. The team firmly believes that emotional support can be as important as the physical and medical support throughout each patient’s unique care journey, striving to be a comforting presence during daunting times. “The most important part of my day is collaborating with the Children's Infusion team to make life manageable for the families that are going through this experience,” added Shelby Nolte, Senior Medical Assistant. “We work as a team to make life easier for the blow of a cancer diagnosis. We are there for our families in every way. If they need a shoulder to cry on, an ear to listen or just someone to play cards with or tell a funny story too, we are there.” “One of the things our team does extremely well to help our patients and their families with new diagnoses is to simply meet them where they are,” said Tiffany Macie. “That looks different for every family and every patient. We work in an environment where can build relationships with our patients and their families. This allows us the unique opportunity to really get to know them. We learn their fears, their joys, their worries, what their family lives are like, and we learn how to best meet them where they are.” Transcending the conventional boundaries of care, the CIS department closely supports each patient, offering them solace tailored to the unique fabric of each family's life.
Read More About Department Spotlight: Children’s Infusion Services
-
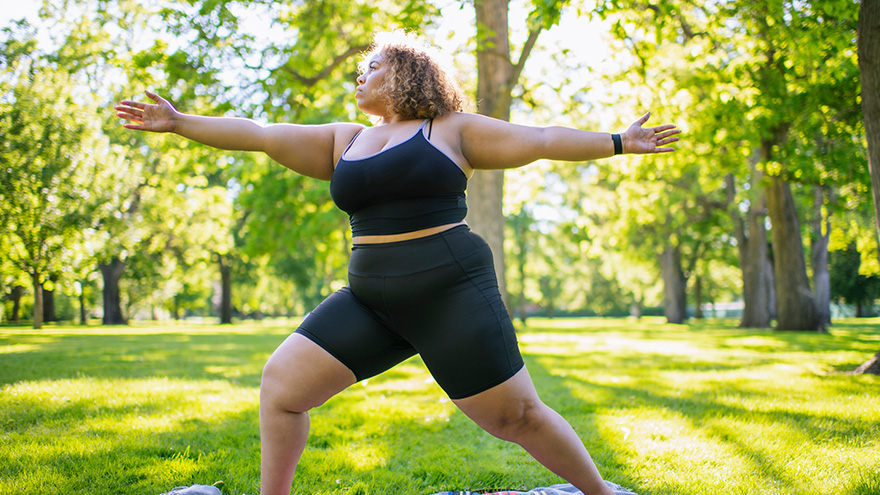
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Top Safe Sleep Tips for Your Baby
Becoming a parent for the first time means lots of new unknowns – from learning to breastfeed and swaddle to buckling your newborn into the car seat for the first time. But when it comes to putting them to bed safely, it’s important to remember it really can mean life or death. It’s something we’re taught before our little one is even here: the correct way to put your baby to bed safely. Sadly though, the number of infant deaths continues to climb. The main culprit of sleep-related infant death continues to be all the items parents leave in the crib with their babies. According to the Center for Disease Control and Prevention, there are about 3,500 sleep-related deaths among babies each year. “The best advice is ‘bare is best.’ Keep your infant’s sleep space clutter free – no blankets, bumpers, toys or pillows,” said Karen Wagner, Pediatric Nurse Practitioner. Follow the ABCs for Safe Sleep Remembering the ABCs is an easy way to remember how to put your little one to bed safely. A: Alone No blankets, toys or pillows. “We do recommend using a sleep sack as a blanket alternative,” said Karen. “It prevents the risk of suffocation and keeps your baby warm.” Keep in mind, the greatest risk for suffocation happens when babies are under 1 year of age, so it’s best to save the toys, blankets and pillows for their “big kid bed,” or around 18 months old. B: Back The slogan “back is best” is another good reminder. Keeping your baby on their back until they’re old enough to rollover helps reduce the risk of Sudden Infant Death Syndrome (SIDS). C: Crib It is best to have your baby sleep alone in their crib. While co-sleeping may be enticing, especially after a late-night feed, it increases the risks of possible suffocation. However, “having your child in your room, in their own crib or bassinet, is protective for SIDS,” Karen said. “In fact, we think co-rooming reduces SIDS risk by almost 50 percent.” Co-rooming allows parents to keep new babies in close reach and helps parents oversee their baby’s sleep, just in case something happens.
-
3 datos importantes de atención médica para la generación milenial
Many millennials are fortunate to have good health, but it’s important to be prepared for your next doctor’s visit. Here are three things that millennials should stay on top of for tracking and maintaining their health. For many millennials, doctor visits and preventive healthcare fall by the wayside. Alison Lynch, MD, a family medicine provider with Renown Medical Group says there are a few key things you can do now to set yourself up for a healthy future. 1. Establish with a Primary Care Provider Millennials are more likely to go to urgent care or consult the internet when a healthcare issue arises. While these are helpful tools, here’s a better one: a primary care provider. The benefit of establishing with a primary care provider is that your medical records, history and a baseline for your health will be documented. That means that when a problem or question comes up, your doctor will already have helpful information on file and can help you navigate your needs. Having a primary care provider is often required for prescription refills and referrals to a specialist. By establishing now, you’ll be able to get what you need in the future much faster. Make an Appointment Today 2. Protect Yourself and Your Community There are a few vaccinations and screenings that Dr. Lynch recommends for millennials. Flu Shots: These are available every year and are recommended for protecting not only yourself against the flu but also others you may come into contact with. Flu shots are usually available from August through December through your healthcare provider, pharmacies and pop-up events. Tetanus or Tdap: Most people receive a tetanus shot as a child, but it’s recommended that everyone get a booster every 10 years. If you are overdue, talk to your primary care provider or pharmacist about getting updated. Pap smear: If you’re a woman, a pap smear is recommended every three years in your 20s and every five years in your 30s. HPV vaccine: This vaccine helps prevent the virus that causes cervical cancer as well as the majority of head and neck cancers and warts. The HPV vaccine is recommended for all genders up until age 45. STD screening: Consider an STI/STD screening if you’re sexually active.
-
Cuidado confiable desde el hogar
Renown Health has always been on the frontlines of technological advancement, and that innovation remained unwavering during the COVID-19 pandemic. Our telehealth teams heeded the call to provide home monitoring for our patients, transforming how we provide care. The care providers at Renown successfully monitored lower acuity COVID-19 patients from the comfort of their own homes. Bernard Lee was diagnosed with COVID-19 and pneumonia, and was able to return home to continue his recovery with a home monitoring system. While at home, Bernard’s health took a turn for the worse while he was sleeping, but thanks to the continuous monitoring of Health at Home, his worsening vitals did not go unnoticed. “This monitoring system really saved my life,” Bernard said. “It was telling me that my sats were low, but I didn’t even feel the common COVID symptoms; I just felt tired.” Because of his low oxygen saturation (sats) and the continuous monitoring, he woke up to providers calling to check on him in the early morning. He was immediately transferred to the Renown Intensive Care Unit to be cared for and monitored by our expert care teams. Today Bernard is recovering, feeling great and continuously refers to the team and the home monitoring system as his guardian angels.
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
A Family's Legacy
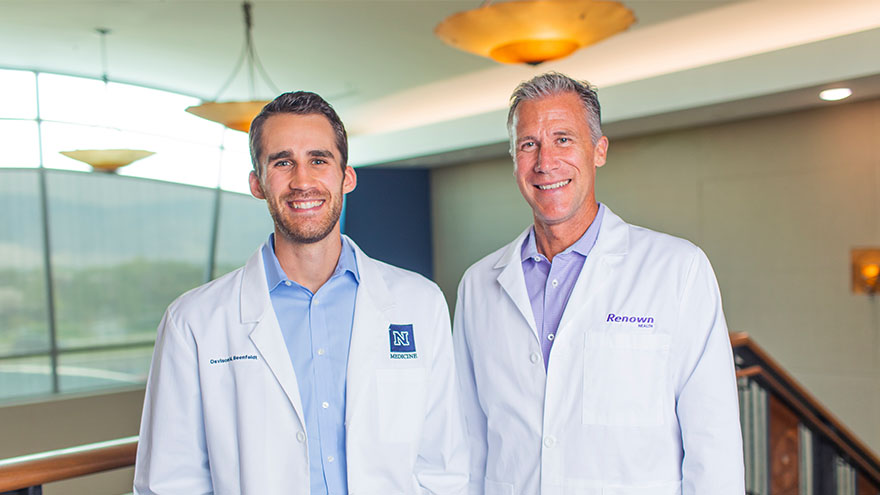
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school
-
El camino hacia la recuperación cerca del hogar
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.
-
What Foods to Eat and What to Avoid When Pregnant
Eating a well-balanced and nutritious diet when pregnant is one of the more essential things you can do for your baby and yourself. The basic principles of what to eat when pregnant are quite similar to how we should be eating all the time. This includes focusing on fruits, vegetables, whole grains, lean protein and healthy fats. Of course, there are a few areas that you should pay close attention to when you’re pregnant and a few foods you should avoid. We consulted Renown Health’s Caitlin Bus, RD, LD, CDE to learn more about pregnancy nutrition. Foods to Eat Regularly: Veggies Vegetables of all kinds -- and in all forms -- are beneficial for you and your baby during pregnancy. Veggies ensure your body is getting the fiber, vitamins and minerals it needs. However, fresh or frozen veggies are considered best, but if you choose to eat canned veggies, make sure you choose a low sodium product. The more greens, the better! If you have an aversion to vegetables, especially in the first trimester, try sneaking them into smoothies. Healthy Proteins Protein-rich foods support your baby's growth while giving your body the nutrients to build and repair tissues, including your muscles, hair, skin and nails. Although protein requirements vary from person to person, a pregnant woman needs additional protein for her baby's growth, especially in the second and third trimesters. Regularly eating high protein foods -- like fish, chicken, turkey, eggs, peanut butter, nuts and beans –– promotes your baby's healthy brain and heart development. Grains Food like brown rice, quinoa, whole-wheat pasta and oatmeal are great to eat while pregnant. They are rich in fiber, iron, B vitamins and folic acid, which are all beneficial to physical development. Grains also help alleviate constipation and hemorrhoids. Fruits Fruit can help satisfy any sugar cravings you have when pregnant while also supplying your baby with nutrients – it's a win-win. Some people advise against fruit consumption while pregnant, but this is a myth. Like with all foods, moderation is key. Fruit can be high in sugar, so it is important to be aware of your intake. Also, make sure you are mindful of your preparation – thoroughly rinse produce under running water for 30 seconds to help avoid foodborne illness. Pasteurized Dairy Dairy products like milk, cheese and yogurt can be great sources of protein and calcium needed for the healthy development of a baby's bones, teeth and muscles. These foods also help with ensuring healthy heart function and nerve transmission. When buying these products, make sure to choose pasteurized products to avoid exposing your body to germs and bacteria. The American College of Obstetrics and Gynecology recommends 1,000mg of calcium per day for pregnant and lactating women. This equates to 4 servings of dairy or calcium-rich foods such as leafy greens, broccoli, tofu, almonds or dried figs. DHA Omega-3 Fats Omega-3s like DHA help support the health of a baby's brain and parts of their eyes. Women who are pregnant or breastfeeding should eat at least 8 ounces and up to 12 ounces of seafood each week. Ideally, food sources that offer DHA omega-3 and that are lower in mercury should be emphasized in your diet, including fish like salmon, sardines and anchovies. If you do not eat fish or omega-3 fortified foods, a DHA omega-3 supplement is recommended. Choline Did you know that 92% of pregnant women fail to meet the daily choline recommendation? Choline is crucial for an infant's brain and central nervous system development. One egg supplies 33% of the recommended daily intake. Although choline is often absent or low in prenatal vitamins, the best food sources include eggs, meats, fish, dairy, navy beans, Brussels sprouts, broccoli and spinach. Iron and Folic Acid Iron is the most common nutrient deficiency during pregnancy. Foods with high and moderate amounts of iron include red meat, chicken, fish, fortified cereals, spinach and beans. Folic acid is used to make the extra blood your body needs during pregnancy. Consuming adequate folic acid early in pregnancy reduces the risk of birth defects that affect the spinal cord. It is recommended to consume 400 micrograms (mcg) per day for pregnant women. This amount is included in your prenatal vitamins. Water Staying hydrated is one of the best things you can do for yourself and your baby when pregnant. In addition to just being good for you, hydration alleviates morning sickness and nausea, while dehydration can lead to contractions and even pre-term labor. Aim for 10 cups of fluids per day, on top of the water naturally occurring in foods. Foods to Avoid: Raw Fish and Fish with High Mercury Content Sorry sushi fans, according to the Center for Disease Control and Prevention, pregnant women are 10 times more likely to get infected by Listeria, a bacteria found in raw or undercooked fish. Also, avoid fish often found to be high in mercury, including swordfish, king mackerel, tuna and marlin. Processed or Raw Meat Similar to eating raw fish, eating undercooked or raw meat increases your risk of infection while pregnant. Hot dogs and lunch meats should also be avoided, unless they have been reheated to be steaming hot (for example, in a microwave). Alcohol Drinking alcohol when pregnant can impact your baby’s brain development and increases your risk of premature birth, low birth weight or miscarriage. Just don’t do it! Minimize Caffeine High caffeine intake during pregnancy can restrict your baby’s growth; therefore, it is recommended that pregnant people limit their caffeine intake to less than 200 mg per day – that’s roughly two cups (16 fl oz) of coffee per day. Runny Eggs Eating raw or runny eggs when pregnant increases your risk of Salmonella, which can cause fever, nausea, vomiting, stomach cramps and diarrhea. Always make sure your eggs are cooked through or use pasteurized eggs.
Read More About What Foods to Eat and What to Avoid When Pregnant
-
La lactancia no tiene por qué significar dolor en los pezones
If you think sore nipples are just a normal part of breastfeeding, think again. Robin Hollen, APRN, and Breastfeeding Medicine Specialist, says that nursing can be an enjoyable experience for mom and baby without pain and discomfort. A top concern of nursing moms within the first week after delivery is how to prevent sore nipples. Even moms who’ve nursed before struggle with this common issue. While many women think it is a regular part of the nursing experience, it is actually a sign that something isn’t quite right. “Nursing your baby should be enjoyable,” says Robin Hollen, Breastfeeding Medicine Specialist with Renown Health. For over 30 years Robin has been supporting moms to breastfeed. Below she shares some valuable information and tips, helping you create a happy and healthy breastfeeding experience for you and your baby. What causes sore nipples? The most common cause of sore nipples involves incorrect latching. For a proper latch, a baby’s mouth takes in the entire nipple and some of the breast, so that the nipple rests at the back of the mouth where the palate is soft. With an improper latch, the mouth may slip down to the tip of the nipple while the baby nurses. This constant pressure on your sensitive skin may cause discomfort and pain. A board-certified lactation consultant can help assess if your baby is latched correctly and troubleshoot your breastfeeding concerns. Less common causes of sore nipples include: • Improper tongue placement of baby • Clenching • Incorrect breast pump use How can a mother prevent sore nipples from an improper latch? Breastfeeding is a learning experience for both mom and baby. Ask for help with the latch so your baby learns it correctly and maintains its depth. In the past, new mothers were surrounded by a community of women — their own mothers, grandmothers, or other family and friends — to provide assistance and guidance with every latch at the beginning of an infant’s life. In today’s culture, new moms can find themselves on their own with no extended family to lend their knowledge. Nurses, pediatricians and lactation consultants now fill that role; they are the eyes and hands along with the much-needed experience to guide new mothers. Our Breastfeeding Medicine experts assist nursing moms with latch every day. Even a single visit with a lactation consultant observing your breastfeeding baby can provide valuable insight on achieving, and maintaining, the proper latch - preventing future nipple soreness and discomfort. How to heal sore nipples from breastfeeding To heal sore nipples, you must first fix the cause, and correcting the latch prevents further damage. A lactation consultant can also help you address the pain. Below are some breast healing tips: • Your own expressed breast milk is excellent to rub into the nipple for anti-bacterial protection. • For those moms who need more lubricant or fat than breast milk offers, use a lanolin or a cream that is labeled safe for the baby. • Soothies are a gel pads providing comfort in between feedings, but should not be used with lanolin products. • Breast shells, not to be confused with shields, can guard the nipples from irritation or pressure in between feedings. If you have more questions about preventing and healing sore nipples or general breastfeeding concerns, talk to your pediatrician or a Renown Health Breastfeeding Medicine specialist at 775-982-6365.
Read More About Breast Feeding Doesn't Have To Mean Sore Nipples