Buscar
-
3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
Ensuring a healthier and more inclusive future for LGBTQIA+ children and teens is of utmost importance to health systems in our community, especially Renown. Supporting the physical and mental health of youth in this community is key to those efforts, especially as they face unique challenges in terms of identity acceptance and social integration. Dr. Caroline Barangan, Adolescent Medicine Physician with Renown Children’s Pediatric Specialty Care, discusses what you as a parent, caregiver, friend or support system can do to be a safe space for children and teens who identify as LGBTQIA+. 1. Create a Safe Space at Home The most important action you can take for your LGBTQIA+ teen or child is to accept and support them for who they are, regardless of how they identify. “Being a teenager is already difficult enough, especially within the LGBTQIA+ community, which puts them at risk of being stigmatized, rejected and targets for bullying,” said Dr. Barangan. Your supportive words and actions can make a huge difference as a profound expression of love and understanding. Being patient and willing to learn are the foundations to a healthy and loving relationship with your LGBTQIA+ teen or child. 2. Encourage Regular Check-Ups with a Primary Care Provider (PCP) Establishing your child or teen with a PCP is not only important when an illness occurs but also for annual preventative visits and regular check-ups. “A primary care provider can screen for high-risk behaviors that would put a patient’s health in jeopardy, such as sexual experience, substance use, suicidality and self-harm,” said. Dr Barangan. “These screenings are an opportunity to provide the education and support these kids and teens need to stay healthy.” One of the main concerns LGBTQIA+ youth often have is that they will experience judgment from their provider, or the PCP will disclose sensitive information, including their sexuality or gender identity to their parents, when they are not ready to do so. Dr. Barangan emphatically reminds us that this legally cannot happen. “If a patient asks me to keep something confidential, unless they disclose that they have plans to harm themselves or others, I am legally not allowed to share that information with anyone without their permission,” said Dr. Barangan. 3. Locate Local Resources Northern Nevada is home to a variety of resources for the LGBTQIA+ community at large, including youth members of this community. "Finding resources to help them develop in a positive way and provide them with the information they need, whether it be in school, the household, the community or through a medical or mental health provider, is incredibly important,” said Dr. Barangan. Below is a list of local LGBTQIA+ community resources open to you and your children: Our Center LGBTQIA+ Health Services at Northern Nevada HOPES Northern Nevada Pride Festival & Community Parade (happens every July in Reno) Sassabration (happens every September in Carson City) Lake Tahoe Pride (events and resources shared on Facebook)
Read More About 3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
-
Departamento destacado: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Nurturing Your Child's Back-to-School Mental Health
The back-to-school season is here, and ensuring your child's successful transition involves more than just school supplies and schedules. At Renown Children’s Hospital, and in collaboration with Nevada Pediatric Psychiatry Solutions, we understand the vital role that mental health plays in a child's overall well-being and academic performance. Below we'll guide you through essential tips for a smooth back-to-school experience, with a special focus on nurturing your child's mental health. How to Support Your Child’s Mental Health from Home Remember, the below strategies can be adapted to align with your child's personality, learning style and household dynamics. Flexibility and understanding are key in tailoring these tips to suit your child's unique needs. 1. Be Open to Communication: Recognize that effective communication is the cornerstone of understanding your child's feelings and concerns. Create a safe space where your child feels comfortable expressing their thoughts. Listen to learn, without judgment. Make it a point to validate their emotions and ensure they are heard. Encourage sharing experiences,worries, friends and challenges they may be facing. Having open conversations about sensitive topics opens the door for discussion and understanding. Make yourself available. 2. Establish a Routine: A consistent routine can offer a sense of stability and predictability for your child, and anticipation helps to decrease anxiety and establish a sense of control. Join forces and design a daily schedule that includes time for schoolwork, play, physical activity, meals and relaxation. Be flexible about the structure to allow room for last-minute changes including extra activities based on that day’s needs as well. Always add time for play and bonding. 3. Practice Compassion: Back-to-school can come with big emotions. Listening reflexively and acknowledging these feelings can help you and your child act positively on these big emotions. 4. Get Involved: Actively engage in your child's school life by participating in school events, meetings and discussions. Show interest in their educational journey, ask about their experiences and provide guidance when needed. Being present in their academic pursuits not only boosts their confidence but also strengthens the parent-child bond. 5. Use Positive Reinforcement: Celebrate your child's achievements, no matter how small they may seem. This allows for a sense of accomplishment and boosts self-esteem. Praise efforts, progress and perseverance, whether it's completing an assignment, making a new friend or overcoming a challenge. This positivity encourages a growth mindset and resilience. 6. Organize a Schoolwork Zone: Create a comfortable workspace at home dedicated to school-related tasks. Customize the area based on your child's preferences and needs. Having a designated space for studying and completing assignments promotes focus, reduces distractions and enhances their overall learning experience.
Read More About Nurturing Your Child's Back-to-School Mental Health
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Your Ultimate Cold and Flu Survival Guide
While viruses can attack year-round, colds, flus and other respiratory illnesses are typically more prevalent during fall and winter. People spend more time indoors, which allows viruses to pass more easily from one person to another. The cold, dry air can also affect the respiratory system, making it more susceptible to germs. According to the CDC, flu activity in the U.S. often begins to increase in October and peaks between December and February. “Flu season” can last as late as May. When it comes to the cold and flu, prevention and preparation are key. Getting the flu shot and a COVID-19 vaccine is the first and most crucial step in protecting against these two respiratory illnesses. Preventative actions, such as washing your hands, covering your mouth and nose when coughing or sneezing and getting enough sleep can also help you avoid getting sick. However, despite your best prevention efforts, the time may come this winter when you start to feel a little scratch in your throat or a fever coming on. By taking steps ahead of time to assemble a cold and flu survival kit, you’ll be more prepared for whenever illness strikes, allowing you to stay home, rest and avoid spreading germs. Tips for Managing Symptoms Keep these tips in mind to ease your cold or flu symptoms: Stay home and rest Drink plenty of fluids Treat aches and fever with over-the-counter medication such as ibuprofen or acetaminophen Manage a cough with over-the-counter expectorants or suppressants Run a humidifier or sit in a steamy bathroom to ease congestion What to Stock in Your Flu Survival Kit Be ready when a cold or the flu strikes by having a flu survival kit filled with these get-well essentials stocked in your pantry, fridge and medicine cabinet: Over-the-Counter Medications: Take advantage of over-the-counter medications to make yourself feel better and ease most common flu symptoms of fever, headache, cough, muscle aches, sore throat, and runny or stuffy nose Pain relievers - Ibuprofen (Motrin and Advil) or Acetaminophen (Tylenol): for fever and aches Decongestants: for sniffles and congestion Cough expectorant (guaifenesin): for a “wet” cough to help clear secretions from the lungs Cough suppressant (dextromethorphan/DM): for a severe “dry” cough to block the cough reflex Cough syrups and drops Drinks: Water Herbal tea Low-sugar sports drinks Pedialyte Foods: Chicken soup Broth Vitamin C-containing fruits and vegetables Oatmeal Toast (add some avocado, honey or egg) Miscellaneous items: Tissues Lozenges Protective mask Thermometer Humidifier When to Seek Care and Where to Go Most healthy adults who have a cold, the flu, or other mild respiratory illnesses don’t need to see a care provider and will recover at home with self-care measures. Because these are viral illnesses, antibiotics won’t work against treating them. Your care provider may be able to prescribe an antiviral medication that can relieve your symptoms and shorten the duration and severity of your illness; however, this needs to be started within 48 hours of symptom onset and is often only prescribed to individuals at high risk for developing complications from the flu or those experience severe symptoms. Primary Care or Urgent Care Contact your primary care provider or visit an Urgent Care if you are at an increased risk, including those who: Are 65 years of age or older Have chronic medical conditions Are pregnant or recently gave birth Have a weakened immune system Find a primary care provider If you are otherwise healthy and not at increased risk of complications, seek medical advice if your flu symptoms are unusually severe, such as mild difficulty breathing, a severe sore throat, coughing that produces a lot of green or yellow mucus, or feeling faint. Emergency Care Go to the Emergency Department if you are experiencing emergency warning signs such as severe pain (chest, abdomen), concern for heart attack or stroke (slurred speech, new localized weakness), severe dehydration (needing IV fluids) or severe shortness of breath.
-
Suicide Risk How to Spot a Friend in Crisis
How can you tell if a friend is in trouble or struggling with suicidal thoughts? And how can you support them in finding help? Are you feeling virtually exhausted? Life is always challenging, but the mental fallout of a global pandemic is real. Contributing to the loneliness epidemic is the shifting American lifestyle. More Americans live alone (28%) now than ever before, and fewer have kids. First, let’s acknowledge this is a time of anxiety and worry for everyone. Economic uncertainty, job transitions, grief, and loneliness are a perfect storm for mental stress. Even before the COVID-19 (coronavirus) pandemic mental health was a concerning issue, now it is a relevant topic of crisis. Secondly, anyone can struggle with suicidal thoughts. Those suffering from drug addiction are especially vulnerable. In particular the U.S. is currently seeing a rise in drug overdoses by almost 18% due to the pandemic. Unfortunately, suicide is responsible for one U.S. death every 11 minutes, according to the Centers for Disease Control and Prevention. Not to mention the millions who think about it, make a plan or attempt it. It is important to remember that suicidal thoughts, plans or intent must be helped immediately. Understanding Suicide Risk To clarify, depression is not a choice. No one wishes for endless days of feeling down, sleepless nights, and feeling as if you are in a dark tunnel. Currently, one in five Americans will experience a mental illness this year. This means one of your friends is struggling, right now. Specifically, consider this: When your body feels pain it talks to your mind. When your mind is suffering who does it talk to? So, how can you tell if a friend is in trouble? According to the National Institute of Mental Health be on the lookout for some depression clues below. Signs and Symptoms of Depression Persistent sad, anxious, or “empty” mood Feelings of hopelessness, or pessimism Irritability Loss of interest or pleasure in hobbies and activities Decreased energy or fatigue Moving or talking more slowly Feeling restless or having trouble sitting still Difficulty concentrating, remembering, or making decisions Signs and Symptoms of Suicide Risk Expressing feelings of hopelessness or having no purpose Talking about feeling trapped or being in unbearable pain Talking about being a burden to others Increasing the use of alcohol or drugs Sleeping too little or too much Withdrawing or isolation Displaying extreme mood swings. Talking about wanting to die or to kill oneself (Reference: Suicide Awareness Voices of Education) How to Help a Suicidal Friend It can feel awkward to approach the subject of suicide with a friend, but take any of the above warning signs seriously. Other ways you can help are by: Encouraging self-care and making sure they take care of basic needs Listen to their worries without judgement Ask them what they need from you, then follow through with action Let them know they are not a burden Don’t minimize or invalidate their feelings Point them to helpful resources Be their advocate and get them help If someone you know is in a life-threatening crisis situation, call 911 immediately. Suicide Risk Resources: National Suicide Prevention 24/7 Lifeline: 1-800-273-8255 Ayuda En Español: (Spanish National Suicide Prevention Lifeline) 1-800-628-9454 Crisis Text Line: Text HOME (or CONNECT) to 741741 to chat with a crisis counselor 24/7 free of charge. The National Alliance on Mental Health: 1-800-950-6264 Substance Abuse and Mental Health Services Administration: (SAMHSA) 24/7 helpline 1-800-662-4357
-
4 fantásticos beneficios para la salud de estar libre de desorden
The Benefits of Being Clutter-Free Gives you a better sense of well-being. Did you know procrastination is linked to clutter? According to a recent study clutter problems led to less life satisfaction, especially among older adults. Helps you lose weight. Constantly being in cluttered room, office or car can be stressful. All the undone cleaning tasks in the back of your of mind cause stress, which is linked to obesity. Promotes mental health. Having clutter around can make you feel anxious or overwhelmed. This prevents you from truly relaxing or focusing. Saves you money. It’s not a secret that money worries cause stress. According to a Journal of Consumer Research study, you’re more likely to make a purchase when you’re sitting in a messy room compared to a tidy room. Clutter-Free Tips Start with a plan. Make a list of your clutter-improvement priorities and the tasks needed to accomplish each one. Focus on one section of your home per week, so you don’t get overwhelmed. In fact, organizational expert Peter Walsh suggests starting with the easiest room first to gain momentum. Conversely, "The Life-Changing Magic of Tidying Up" author Marie Kondo suggests organizing by category (for example clothing or books). Experiment with an organizing plan that appeals to you. There are also many helpful on-line calendars you can use as a starting point. Delegate when you can. Include your children and spouse into your plan. Is uncle Bob an electrician? Then get him to swap out your eyesore of a ceiling fan or update an old light fixture. Of course it’s ok to outsource the duties - such as window cleaning or painting - if your budget allows. Buy less. The less you purchase the less you need to store, clean, keep track of, organize or dust. Seems simple, right? Not for everyone. On average we are bombarded with over 4,000 marketing messages a day, not to mention FOMO (Fear Of Missing Out) when we see our friends posting about their newest toys on their social media feeds. Focus on quality over quantity. When in doubt, throw it out. Still on the fence about what to throw away? Use these declutter decision-making guide questions to help you. Organize Your Health Along with taking care of your surroundings, make a commitment to get up to date on your health checkup and screenings. Preventing an illness is a bargain compared to the cost of a chronic disease. It's also a good idea to go through all of your medications and check the expiration date. Remember to properly dispose of medications. DO NOT flush medications down the drain or toilet, unless the label indicates it is safe to do so.
Read More About 4 Fantastic Health Benefits of Being Clutter-Free
-
Conexiones sociales: por qué benefician su salud
Some days a chat with a friend is all you need to feel better. Why? Because humans are social beings. Although we have more technology than ever at our fingertips, sometimes we may still feel left out or disconnected. Dr. Buddy Coard, Ed.D., Psychologist at the Stacie Mathewson Behavioral Health Addiction Institute at Renown, discusses the importance of social connections and tips on how to keep connecting, warning signs of loneliness and how to feel less lonely. Why are Social Connections Important? Dr. Coard points to significant research on the topic of loneliness and social connections. He uses the findings below to detail how social connections affect our overall health. In a recent survey 40% of participants reported they sometimes or always feel that their relationships are not meaningful and that they feel isolated. Surprisingly, this survey suggests Generation Z (18-22 years old) is the loneliest generation. Another study associates loneliness as a risk factor for early death. It indicates lack of social connection heightens health risks as much as smoking 15 cigarettes a day, or having alcohol use disorder. In fact, loneliness and social isolation are twice as harmful to physical and mental health as obesity (Perspectives on Psychological Science, Vol. 10, No. 2, 2015). A 2018 study investigated several standard measures of social isolation, including marital status, frequency of religious service attendance, club meetings/group activities and number of close friends or relatives. The findings revealed race as a strong predictor of social isolation. In particular, black men and women were more likely to be lonely than were white men and women. Loneliness also switches on your body’s long-term “fight-or-flight” stress signaling system, which negatively affects your immune system. People who feel lonely have lower immunity and more inflammation than people who don’t. Dr. Coard recommends the following tips for those who feel lonely. Tips to Increase Social Connection Get outside. More and more nature prescriptions are common. In fact even a 10 minute walk can elevate your mood and get your blood flowing. Develop a schedule of activities to accomplish in a week, setting realistic goals. Monitor your technology. Of course, watching the 24/7 news cycle can be depressing. Turn off the TV and listen to music or read a book instead. Even better, use technology to connect with family members by having a virtual game night or book club discussion. Write it out. When was the last time you sent a good old-fashioned letter or card? Or even wrote in a journal? Try to brighten someone’s day with snail mail. Writing down your hopes and fears also helps you to get worries off your mind and process your emotions. With this in mind, there are also volunteer opportunities to support others by sending a handwritten letter to others battling depression. De-clutter your surroundings. Go through those old photos and put them in an album. Clean out a drawer, cupboard or closet. You will feel a sense of accomplishment and can donate items you no longer need that others can enjoy. Increase your joy by reducing your clutter. Warning Signs of Chronic Loneliness One size does not fit all when it comes to loneliness. For this reason, loneliness can be different depending on your particular situation and your unique personality. However, if you feel some (or all) of the following symptoms, chronic loneliness may be affecting you: Lack of ‘best’ or close friends. You connect with others on a surface level, but feel no one truly understands you. People are n your life, yet you are not connecting on a deep, intimate level with them. You feel lonely even when people are around. This means feeling disengaged or not part of the group when around others. You feel less than enough. You often doubt yourself or don’t feel good enough when comparing yourself to others. And social situations feel exhausting. What Can Someone Do to Feel Less Lonely? Dr. Coard offers the following suggestion for those with a lack of social connections: Talk with your doctor, psychologist or another healthcare professional. Sometimes chronic loneliness relates to longstanding negative beliefs that an individual has about themselves. Engage in behavioral activation. For example, being more active and involved in life by scheduling activities which can potentially improve your mood and decrease feelings of isolation. Initially behavioral activation can be very challenging due to lack of motivation, but setting a reasonable schedule of activities is a good start. Pay attention to your sleep. Sometimes when people become lonely they experience significant changes in their sleep cycle. Frequently they sleep too much, or too little. Make sure to maintain a normal, healthy sleep/wake cycle, following good sleep hygiene recommendations.
Read More About Social Connections: Why They Benefit Your Health
-
Cuidado confiable desde el hogar
Renown Health has always been on the frontlines of technological advancement, and that innovation remained unwavering during the COVID-19 pandemic. Our telehealth teams heeded the call to provide home monitoring for our patients, transforming how we provide care. The care providers at Renown successfully monitored lower acuity COVID-19 patients from the comfort of their own homes. Bernard Lee was diagnosed with COVID-19 and pneumonia, and was able to return home to continue his recovery with a home monitoring system. While at home, Bernard’s health took a turn for the worse while he was sleeping, but thanks to the continuous monitoring of Health at Home, his worsening vitals did not go unnoticed. “This monitoring system really saved my life,” Bernard said. “It was telling me that my sats were low, but I didn’t even feel the common COVID symptoms; I just felt tired.” Because of his low oxygen saturation (sats) and the continuous monitoring, he woke up to providers calling to check on him in the early morning. He was immediately transferred to the Renown Intensive Care Unit to be cared for and monitored by our expert care teams. Today Bernard is recovering, feeling great and continuously refers to the team and the home monitoring system as his guardian angels.
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
A Family's Legacy
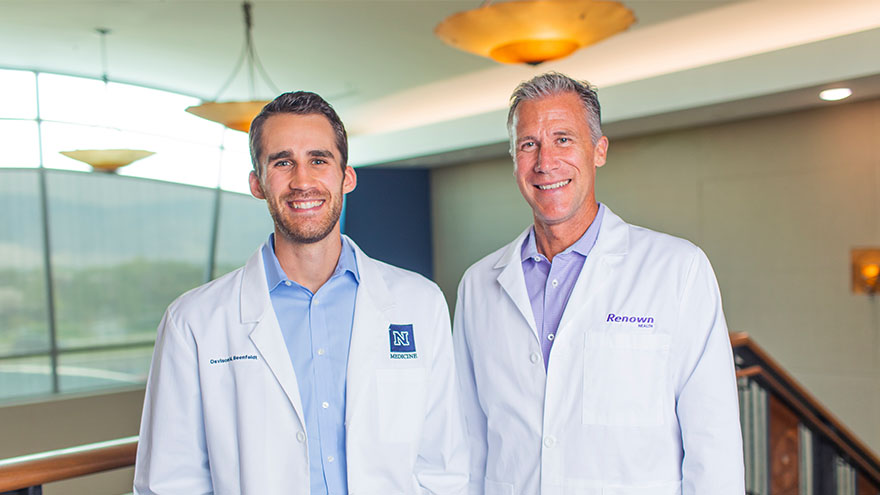
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school
-
El camino hacia la recuperación cerca del hogar
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.