Buscar
-
What is an Ovarian Cyst, and How is it Treated?
Abdominal pain is one of the most common reasons for an Emergency Room visit. The abdomen is an area that encompasses multiple organs and functions. So how would you know when the pain you are feeling is an ovarian cyst or something else, and when should you seek medical attention? Dr. Carilyn Hoffman, at Renown Women's Health, explains. Ovarian Function Defined Located on each side of the uterus, the ovaries are part of the female reproductive organs and produce eggs (ova), released during the menstrual cycle, allowing for fertilization and pregnancy. They also produce hormones such as estrogen and progesterone, which play an important role in female traits, bone health, cardiovascular health and pregnancy. Symptoms of an Ovarian Cyst Cysts are solid or fluid-filled masses. Ovarian cysts can be in the ovary or on its surface. When cysts are enlarged or rupture, they can create a dull ache or sharp pain below the belly button. Besides discomfort and pain, other symptoms of ovarian cysts may include bloating, fullness, pressure or heaviness. "Ovarian cysts are common; most are physiologic and will go away on their own. They are frequently found incidentally on ultrasound and are present in the middle of the menstrual cycle," says Dr. Hoffman. "However, if a woman experiences sudden and severe pelvic pain they should seek immediate medical attention. Sometimes ovarian cysts can become large and twist on themselves. This is called ovarian torsion and is a surgical emergency. Other times, cysts can rupture and bleed. This is called a hemorrhagic cyst and can also be a surgical emergency." Diagnosis and Treatment If an ovarian cyst is suspected, your doctor will perform a pelvic exam and order an ultrasound. There are certain ultrasound findings that suggest that the cyst is benign. There are other ultrasound findings that are concerning for cancer. Small simple cysts often resolve on their own, whereas solid or very large cysts may require surgery.
Read More About What is an Ovarian Cyst, and How is it Treated?
-
Why Am I So Tired? 9 Reasons for Your Chronic Exhaustion
Do you find yourself struggling to stay awake during the day or having no energy? You’re not alone. Whether you’re a full-time employee, a student or retiree, that “I’m tired” feeling comes in all shapes and sizes. What’s even more frustrating is not knowing the source of your exhaustion. Dr. Brandon Flores, a sleep medicine physician with Renown Medical Group, breaks down nine key reasons why you may be feeling so fatigued. You did not get enough sleep, or your quality of sleep is poor. This may seem obvious, but in today’s “rise and grind” culture, sleep can be considered a luxury rather than what it really is: a necessity. Ensuring you get adequate hours of sleep between 6-9 hours and quality sleep is essential. You may not be breathing well during sleep. Interruptions to your breathing, such as snoring, can decrease airflow at night causing your sleep to be less restorative. This is often due to Obstructive Sleep Apnea (OSA). OSA can lead to daytime fatigue and sleepiness and can also impact other chronic health conditions, such as hypertension, diabetes, acid reflux, migraines and heart rhythm. You are not getting enough regular exercise, or you are exercising too much. Incorporating at least 30 minutes a day of physical activity can help keep you energized throughout the day. It has also been shown to increase deep slow wave sleep, which is often associated with feeling rested. On the other hand, getting too much exercise can tire you out more easily and heighten stress levels. You drink too much caffeine. This one may seem counterintuitive – caffeine is supposed to keep you awake, right? Well, overdoing it with your favorite coffee or soda could affect your sleep quality. Pay attention to your caffeine limits and have a cut-off time, as most caffeine should not be consumed past noon. You have a food allergy or intolerance. If you find yourself feeling especially tired after eating a lot of a certain food, you could have an allergy or intolerance to it – and vice versa. Consider speaking with your primary care provider (PCP) about a food allergy test or being referred to an allergist. You’re drinking too many alcoholic beverages. Alcohol is a depressant, which as the word implies, can make you feel especially tired during the day. It can also affect your breathing at night and disrupt your sleep cycle. Cutting back on alcoholic drinks may be beneficial to your overall health. You are anemic. This is the leading cause of fatigue in women but can affect people of all genders. It can be associated with low iron. Eating foods high in iron, including leafy greens and many different meats, can help your iron levels. A blood test ordered by your PCP can help you understand if you are iron deficient. You are experiencing depression or anxiety. Emotional exhaustion can be just as taxing as physical exhaustion. Prolonged feelings of sadness, hopelessness, nervousness or panic can be signs and symptoms of depression or anxiety. Speak with your provider about the many resources available to help you. You have an underactive thyroid. Feeling fatigued can also be a symptom of hypothyroidism, which affects your metabolism and energy levels. Medication can help get your thyroid back to normal. Your PCP can order a blood test to determine your thyroid levels. If you experience severe exhaustion that lasts six months or longer, worsens after physical or mental exertion and does not get better after resting, it could be a sign of myalgic encephalomyelitis, otherwise known as chronic fatigue syndrome (CFS). This is a diagnosis of exclusion, and other causes must be ruled out. While there are no tests that detect CFS, your provider can order blood and urine tests to rule out other causes of your fatigue and help develop a care plan.
Read More About Why Am I So Tired? 9 Reasons for Your Chronic Exhaustion
-
Eight Lessons from an MD-PhD Candidate at UNR Med
Meet newly minted Dr. Majid Khan, PhD., a native of Reno, and current MD-PhD candidate and first-generation medical student at the University of Nevada, Reno School of Medicine, who is on his way to a career as a Neurosurgery. While most graduate students often choose between pursuing a medical degree (MD) or a doctorate in philosophy (PhD), Majid has boldly picked both. He is one of three medical students currently in the UNR Med MD-PhD Program run by Dr. Caroline Cobine, PhD and Dr. Violeta Mutafova-Yambolieva, MD, PhD. "Research is not merely an act of sitting at a computer and reading papers – it's about answering the thought-provoking questions about things we come across on a daily basis. By critically evaluating these ideas we can implement solutions to enhance various aspects of the medical field and patient care with an overall goal of improving patient outcomes," Majid said. Majid recognizes that modern research extends beyond academia and holds significant value for hospitals. “Research contributes to improving patient outcomes. By reviewing the data from peer-reviewed research studies, medical professionals can be better prepared to deliver effective care following the most up-to-date guidelines and data,” he said. Majid's journey to pursuing his MD-PhD with a goal of becoming a physician-scientist-surgeon began following a summer in the PathMaker Cancer Research Program at the Huntsman Cancer Institute at the University of Utah. "It was by fate that I stumbled into this field – ever since I saw my first brain surgery, I haven’t been able to look back," Majid said. Here are some of the valuable lessons that Majid has learned along the way. 1. Beyond the 9 to 5, Embrace both 5 to 9s To avoid burnout and nurture personal passions, make your time spent outside of work and school intentional. Harness any free time to reconnect with friends, pursue hobbies and engage with mentors and mentees. 2. Collaboration is Key Work collectively with colleagues locally, nationwide and even worldwide. Cultivate environments to share knowledge and innovation, as well as wisdom, which will evidently lead to more impactful outcomes. 3. Shine a Spotlight on Your Colleagues Acknowledge and celebrate your colleagues in group settings when you notice something outstanding that they’ve said or done – it could anything big or small. Shining the spotlight onto those who are making positive changes within the hospital can inspire a beautiful culture of academic healthcare, which ultimately improves patient outcomes. 4. Redefine Mentorship Mentorship does not need to be confined to traditional frameworks. Seek out guidance in unexpected and untraditional places; sometimes, the most enlightening lessons and opportunities emerge from the most unlikely sources. 5. Diversify Your Experiences Embracing a diverse range of experiences enriches one's medical acumen. You never know when a seemingly unrelated job or experience will help in a scenario in your career. 6. Live By the Mamba Mentality Follow the late Kobe Bryant’s approach to life and work, the Mamba Mentality. This includes planning long-term goals, placing meaning in everything, striving for constant personal growth, following your passions and focusing on the process rather than the end goal. 7. Make Time for Your Loved Ones Don’t forget who helped you get to where you are in your life, specifically your family, friends, teachers and mentors. By making time for the most important and loving people in your life, you will be surrounded by positivity which will help propel you to new heights. 8. Plan your Next Five Moves We all have the ability to come from nothing and become something. Take the time to plan out everything and execute your moves with careful precision. Majid has plans to return to the Biggest Little City after completing Neurological Surgery Residency Program. If you would like to get in touch with Majid, please reach out to him via email at majidk@med.unr.edu.
Read More About Eight Lessons from an MD-PhD Candidate at UNR Med
-
Departamento destacado: Float Pool
Ring in the New Year and the rest of the holiday season by celebrating Renown’s Float Pool team! After coming out of the COVID-19 pandemic, it's no mystery that healthcare across the country has shifted and adapted to the growing needs and new demands of our patient populations. Renown Health is no different. As the largest not-for-profit health system in the region, we are no stranger to change, even when change presents challenges. Who do we call on when a unit needs more team members in the eleventh hour? Who can help when our patient volume spikes up with seconds to spare? This is where the Float Pool at Renown comes to the rescue. Skilled in a wide variety of healthcare specialties, from acute care nursing and critical care to care aiding and patient safety, this is the team that can seamlessly step in to provide crucial patient care to the units that need it most, whether a team is understaffed for the day or needs extra all-hands-on-deck for a specific patient or procedure. Float Pool team members are equipped to work in virtually any clinical area at Renown, making a genuine difference with every patient they encounter. A Pool of Relief Teams across Renown can breathe a sigh of relief knowing that Float Pool has their back in times of need. As the backbone of our health system, these dedicated team members possess a wealth of clinical knowledge and the ability to navigate diverse medical environments. Their flexibility allows them to fill staffing gaps and provide essential support to many different units. “We fill in the gaps of staffing to make everyone's day better,” said Patti Crepps, Critical Care Float Pool RN. “A float nurse has to be flexible and able to adapt to different situations and places – basically, ‘go with the flow.’ Patient care is basically the same all over; we make patient care possible by being familiar with all the various specialties and providing the specific care needed depending on the population we are taking care of on that shift.” “Float Pool staff members are like healthcare chameleons, transitioning between different departments,” added Shelby Riach, Acute Float Pool RN. “We incorporate flexibility, teamwork and a commitment to ensuring patients receive the best care, regardless of the setting or circumstances.” This team thrives in uncertainty; in fact, no workday is the same in Float Pool – and that’s exactly the way they like it. Working with many different teams across a multitude of specialties, these Care Aides, RNs, Critical Care Techs, Patient Safety Assistants (PSAs), Certified Nurses Assistants (CNAs) and more enjoy facing change, while they all share a goal of providing the best patient care possible. “No day looks the same; since we are the Float Pool, we are assigned a different assignment on Smart Square every day, whether it be as a care aide, a patient safety assistant, a unit clerk or patient transport,” said Melina Castenada, Care Aide. “If we are assigned as a care aide on the floor, we help assist with call lights and help with whatever nurses and CNAs may need, including feeding, transporting, walking, helping patients use the restroom, etc. When we are assigned as a PSA ‘sitter,’ we sit for the patient to help keep them safe. If we are assigned as unit clerk, we help answer phones and direct patients appropriately, file paperwork, answer call lights if needed and assist with office work.” “I love that every day is a different floor with different tasks and a different atmosphere,” added Julia Chappell, Critical Care Technician. “I find out which floor that I will be on right before my shift starts and head to the floor to find out my assignment for the day. Depending on the specialty, such as the medical-surgical floor versus an intensive care unit (ICU), my daily job tasks can vary.” When it comes to high-risk patients, who require special attention, PSAs within Float Pool step in to help. “The PSA role within Float Pool largely consists of adverse event prevention for our high-risk patients, and being a Float Pool employee allows us to work wherever we are needed,” said Dimitri Macouin, Patient Safety Assistant. “Whether it be in the emergency department, neurology or pediatrics, the PSA will be the eyes and ears for the nurses working with this patient population.” “Great strides have been made to ensure that PSAs remain vigilant and are recognized as an integral part of the patients' care team rather than 'just a sitter,’” added Karla Phillips, Patient Safety Assistant. Float Pool also oversees our Discharge Lounge, which offers patients and their families a dedicated space to reconnect and prepare for their discharge from the hospital. “The increase in utilization of the Discharge Lounge is something we are very proud of,” said Kara Abshier, Care Aide. “We assist in discharging patients from all over the hospital to help the floor and get new patients into rooms.” Every day brings a new challenge for Float Pool. As these team members wake up with uncertainty, they are ready to embrace the diverse demands of caring for patients of all ages. “The fact that Float Pool exists is amazing,” said Hannah Luccshesi, Acute Float Pool RN. “We wake up with no clue as to whether we will be working with babies, children or adults and then fill in the needs of the hospital.”
-
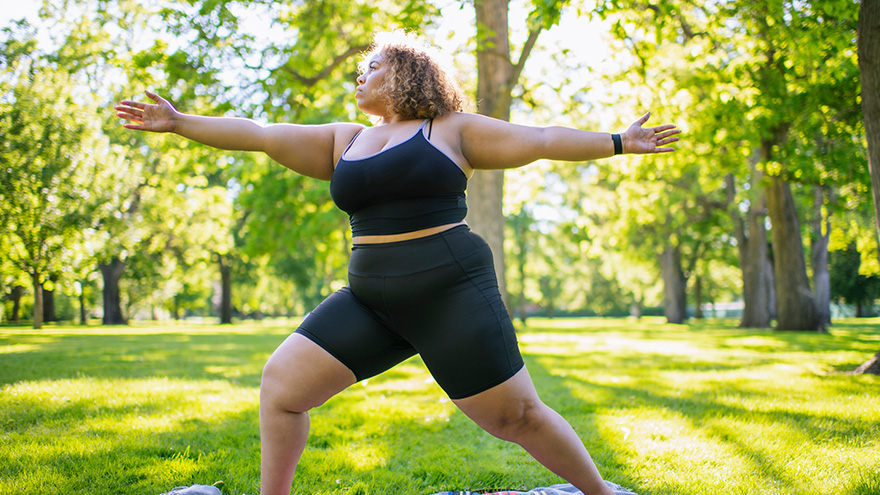
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
Ensuring a healthier and more inclusive future for LGBTQIA+ children and teens is of utmost importance to health systems in our community, especially Renown. Supporting the physical and mental health of youth in this community is key to those efforts, especially as they face unique challenges in terms of identity acceptance and social integration. Dr. Caroline Barangan, Adolescent Medicine Physician with Renown Children’s Pediatric Specialty Care, discusses what you as a parent, caregiver, friend or support system can do to be a safe space for children and teens who identify as LGBTQIA+. 1. Create a Safe Space at Home The most important action you can take for your LGBTQIA+ teen or child is to accept and support them for who they are, regardless of how they identify. “Being a teenager is already difficult enough, especially within the LGBTQIA+ community, which puts them at risk of being stigmatized, rejected and targets for bullying,” said Dr. Barangan. Your supportive words and actions can make a huge difference as a profound expression of love and understanding. Being patient and willing to learn are the foundations to a healthy and loving relationship with your LGBTQIA+ teen or child. 2. Encourage Regular Check-Ups with a Primary Care Provider (PCP) Establishing your child or teen with a PCP is not only important when an illness occurs but also for annual preventative visits and regular check-ups. “A primary care provider can screen for high-risk behaviors that would put a patient’s health in jeopardy, such as sexual experience, substance use, suicidality and self-harm,” said. Dr Barangan. “These screenings are an opportunity to provide the education and support these kids and teens need to stay healthy.” One of the main concerns LGBTQIA+ youth often have is that they will experience judgment from their provider, or the PCP will disclose sensitive information, including their sexuality or gender identity to their parents, when they are not ready to do so. Dr. Barangan emphatically reminds us that this legally cannot happen. “If a patient asks me to keep something confidential, unless they disclose that they have plans to harm themselves or others, I am legally not allowed to share that information with anyone without their permission,” said Dr. Barangan. 3. Locate Local Resources Northern Nevada is home to a variety of resources for the LGBTQIA+ community at large, including youth members of this community. "Finding resources to help them develop in a positive way and provide them with the information they need, whether it be in school, the household, the community or through a medical or mental health provider, is incredibly important,” said Dr. Barangan. Below is a list of local LGBTQIA+ community resources open to you and your children: Our Center LGBTQIA+ Health Services at Northern Nevada HOPES Northern Nevada Pride Festival & Community Parade (happens every July in Reno) Sassabration (happens every September in Carson City) Lake Tahoe Pride (events and resources shared on Facebook)
Read More About 3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
-
Foods to Avoid When Taking Heart Medications
Did you know certain medications can interact with everyday food and drink? We asked VP of Pharmacy Services Adam Porath how to take these important medications safely. One in five Americans between the ages of 40 and 75 are currently taking a statin drug to reduce their cholesterol level or to prevent atherosclerosis (hardening of the arteries). Many others also take anticoagulants (blood thinners) to prevent blood clots from forming, which can increase the risk of stroke. Adam Porath, VP of Pharmacy Services at Renown Health, explains how to safely take these medications. What is a statin? A statin is a drug that can lower cholesterol by helping your body absorb cholesterol or by blocking a substance your body needs to make it. The American Heart Association cites a global study reporting the benefit of statins to help reduce heart attacks and strokes. Common statins include atorvastatin (Lipitor), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor). Which foods or drinks should be avoided while taking statin drugs? Grapefruit juice is the only food or drink that has a direct interaction with statins. Statins do not directly interact with any food but people taking statins should moderate their intake of saturated fats to help lower their LDL cholesterol and overall risk of cardiovascular disease. What is a blood thinning drug? Blood thinning drugs, such as warfarin, rivaroxaban (Xarelto), apixiban (Eliquis), dabigatran (Pradaxa) and edoxaban (Savaysa), are used to prevent stroke. Which foods or drugs should be avoided while taking blood thinning drugs? If taking warfarin, alcohol and cranberries (including juice) should be avoided. Patients taking warfarin should be aware of foods that contain Vitamin K (green leafy vegetables) and try to maintain a consistent diet of these foods. Warfarin interacts with many over the counter and prescription medications. Patients should consult a pharmacist when starting, stopping, or changing doses of any medication when taking warfarin. Also, patients taking any blood thinning medication should avoid over-the-counter pain relievers (i.e. aspirin, ibuprofen, etc.) How do I know whether to take my medication with food or not? Consulting with a pharmacist is the best resource to determine if a medication should be taken with or without food. In general, all statins and blood thinners can be taken with or without food. The only exception is Xarelto (rivaroxaban), which should be taken with the largest meal of the day If you are a Renown patient you can also review your prescriptions online, request a refill or ask a question via MyChart. With MyChart, you can access all your healthcare information securely 24/7.
Read More About Foods to Avoid When Taking Heart Medications
-
Guide to Injury Healing: Heat or Ice?
Heat and ice are two of the most common treatments used to relieve pain and reduce swelling in injuries. However, each one is better suited for certain types of injuries Dr. Luis Palacio, MD explores the differences between the two. When it comes to treating aches and pains, the debate between heat and ice has been ongoing for quite some time. Both have their benefits making it crucial to understand which option is better suited for your specific needs. Determining which method is better depends on various factors such as the type of injury or pain you are experiencing. For instance, if you have recently sprained your ankle or pulled a muscle during exercise, applying ice within the first 48 hours can help minimize swelling and alleviate discomfort. It's worth noting that some individuals find alternating between heat and ice therapy beneficial as well. This approach combines the benefits of both methods by using heat to increase blood flow followed by ice to reduce inflammation. Cold Therapy Cold therapy can help to reduce inflammation after an injury, heat can have the opposite effect. Therefore, heat therapy should be reserved for those who have chronic pain issues and are not dealing with an acute injury. Cold therapy is often recommended immediately after an injury or during the initial stages of inflammation. Cold therapy such as ice packs are especially effective in treating: Sprains Strains Any injury that involves swelling Heat Therapy Heat therapy is known for its ability to relax muscles, increase blood flow and soothe pain. It is often used for chronic conditions or injuries that are not inflamed. Applying heat can help alleviate stiffness, promote healing and provide a comforting sensation. This increased circulation can bring more nutrients and oxygen to the area, helping it to heal faster. Heat therapy such as heating packs are especially effective in treating: Stiffness with associated pain Injuries that are not inflamed Muscle pain
-
6 Healthcare Action Items for the LGBTQIA+ Community
Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
Take a Stand Against Domestic Violence
October is Domestic Violence Awareness Month in the United States. We spoke with Renown Health experts and local domestic violence prevention organizations who gave us a deeper look into understanding the warning signs of abuse and the many proactive and reactive resources in our community that you can reach out to today. Domestic violence, also referred to as domestic abuse, is an everyone issue. Whether you identify as male or female, an adult or a child, single or partnered – domestic violence can affect anyone. In fact, it may be closer to home than you might think. According to the Nevada Quality Parenting Initiative, in Nevada, 43.8% of women and 32.8% of men experience domestic violence in their lifetime, and the risk of that figure rising is imminent. This year alone, the Domestic Violence Resource Center (DVRC) in Reno experienced a 55% increase in overnight emergency stays, according to the Reno Gazette-Journal. This problem also, unfortunately, extends to children. More than 5,000 children in Nevada were reportedly primary or secondary victims of domestic abuse in 2021, as stated by the Nevada Coalition to End Domestic and Sexual Violence. “Domestic violence can manifest in many different ways,” said Kami Price, Supervisor of Social Services for Renown Health. “Abuse isn’t always strictly physical. It can also be emotional, verbal, sexual and even digital. Understanding those differences can help you prepare accordingly and respond safely if you or a loved one are experiencing domestic violence.” Knowing what to look out for is crucial in protecting yourself and others against the effects of domestic abuse and taking action when warning signs appear. The National Domestic Violence Hotline shares the common signs of an abusive partner, no matter how old they are or what gender they identify as: Telling you that you never do anything right. Showing extreme jealousy of your friends or time spent away from them. Preventing or discouraging you from spending time with friends, family members or peers. Insulting, demeaning or shaming you, especially in front of other people. Preventing you from making your own decisions, including about working or attending school. Controlling finances, including taking your money or withholding money for needed expenses. Pressuring you to perform sexual acts you’re not comfortable with. Pressuring you to use drugs or alcohol. Intimidating you through threatening looks or actions. Threatening to harm or take away your children or pets. Intimidating you with weapons. Destroying your belongings or your home. "People experiencing domestic violence may feel as though they are trapped,” said Kami Price. “The reality is – this often couldn’t be further from the truth, especially with the resources we have at our disposal in northern Nevada.” Respected Resources Ending the Silence on Domestic Violence While these facts and figures might be staggering, those experiencing domestic violence at any age are not alone. There is hope at the end of the tunnel, especially here locally. Devoted to meeting the growing needs of the communities we serve, Renown Health proudly supports and sponsors several organizations in our community that are committed to educating children and adults on the signs and symptoms of domestic violence, along with what each child and family member can do today to prevent abuse in the household. These essential organizations are on the frontlines of shifting attitudes from “I don’t want to get involved” to “How can I help?” Serving children across northern Nevada, the Child Assault Prevention (CAP) Project offers “education and prevention programs designed to increase children’s safety from bullying, abuse and assault” and break the cycle of domestic abuse. During 2021 and the first half of 2022, CAP led about 500 different workshops, teaching 10,000 second-grade and fourth-grade children in Washoe, Storey, Lyon and Churchill Counties how to keep themselves safe from domestic violence. “As domestic violence is on the rise, open communication, early intervention and education are key to protecting children from the effects of domestic violence," said Rebecca LeBeau, Executive Director of the CAP Project. “That’s why I begin speaking about child assault prevention and stranger danger to kids as young as six years old. It's important to explain the true reality of domestic violence to both children and adults, tailoring language specifically to whatever age they are, and allowing them to process it. Kids of all ages will learn how to deal with extremely dangerous situations this way.” According to Rebecca, common symptoms of abuse to be on the lookout for at school include grades dropping, a lack of focus and feelings of not wanting to return home after the school day ends. If someone in a child’s home is being hurt or abused, children are always encouraged to speak with a trusted adult or school counselor. From there, organizations like the CAP Project develop a safety plan moving forward. Adults and family units aren’t alone either. The DVRC provides a wide variety of services to Washoe County residents experiencing domestic abuse. To date, the DVRC has helped more than 100,000 victims of domestic violence, and with the recent launch of their crisis text line, they are poised to serve many more. Like the CAP Project, the DVRC also believes that education is one of the first lines of defense against domestic violence. “Education on what domestic violence looks like is so much more than talking about physical violence,” said Aria Overli, Volunteer Coordinator at the DVRC. “Educating the community, and particularly youth, about what healthy relationships look like is a major factor in preventing abuse. Understanding the intersection of how other issues – such as race, mental illness and immigration status – affect domestic violence risk factors is key to addressing those issues.” The list doesn’t stop there. Renown Health Foundation has provided financial support for many more organizations that are dedicated to ending the silence on domestic violence, sexual violence and family abuse, including: The Children’s Cabinet – A child-focused organization offering many support services for youths and families, including Safe Place, a program that partners with local businesses to offer safe locations for children to seek help if they feel threatened at school or at home. The organization also provides free family counseling, providing a pathway to better communication for families experiencing a myriad of issues ranging from domestic violence to substance abuse. Awaken – A nonprofit committed to increasing awareness and education regarding sex trafficking and providing housing and healing to all survivors. Safe Embrace – The largest and most inclusive safe house in Reno-Sparks for survivors of domestic and sexual violence, offering a wide range of resources including counseling, emergency transportation, court support and more. Eddy House – A safe space for at-risk individuals aged 18-24 recovering from the effects of domestic abuse, unsafe housing conditions, homelessness and more. Being an advocate starts with us – if you see something, say something. Keeping a transparent line of communication is key to preventing, noticing and combating domestic violence. “The more you reach out and talk about the issues, the better,” closed Kami Price. “No one has to go through their struggles alone.”
-
Keeping Kids Safe on Halloween
Halloween is around the corner. So while you're prepping pumpkins for carving, putting together creative costumes and coordinating trick-or-treating plans, safety is one more detail to remember. Masks, haunted houses, witches, ghosts and ghouls — it all spells Halloween, and what could be more frighteningly fun, right? For children, however, Halloween can indeed be frightening and not so fun. According to Dr. Kristina Deeter, Physician-in-Chief of Renown Children’s Hospital and Chair of Pediatrics for the University of Nevada, Reno School of Medicine, it is common for younger children to express Halloween fears — being afraid of monsters, the dark or really anything out of the norm. “It's normal for children to struggle with separating reality from fantasy,” she explains. For children who fall into this category, the month of October can be traumatizing. Halloween may not come until the end of the month. Still, in the weeks building up to the spookiest night of the year, little ones are bombarded on all sides with decorations — mummies, skeletons, coffins, vampires, you name it. For a child with a blossoming imagination who, as Dr. Deeter said, is still learning to differentiate real from pretend, this can cause additional fears and anxieties. In commemoration of Halloween Safety Month, Dr. Deeter shares safety tips for the spooky holiday from the American Academy of Pediatrics: Dressing Up & Heading Out Plan costumes that are bright and reflective. Ensure shoes fit well and that costumes are short enough to prevent tripping, tangling or coming into contact with flames. Consider adding reflective tape or striping to costumes and trick-or-treat bags and baskets for greater visibility. Masks can limit or block eyesight. Instead, consider non-toxic makeup and hats, which should fit properly to prevent them from sliding over the eyes. Test makeup ahead of time on a small patch of skin to test for allergies before full application. When shopping for costumes, wigs and accessories, look for and purchase those with a label clearly indicating they are flame resistant. If a sword, cane or stick is a part of your child's costume, make sure it is not sharp or long. A child may be easily hurt by these accessories if he stumbles or trips. Do not use decorative contact lenses without an eye examination and a prescription from an eye care professional. While the packaging on decorative lenses will often make claims such as "one size fits all," or "no need to see an eye specialist," obtaining decorative contact lenses without a prescription is both dangerous and illegal. This can cause pain, inflammation, serious eye disorders and infections, which may lead to permanent vision loss. Review with children how to call 9-1-1 (or their local emergency number) if they ever have an emergency or become lost. Carving Pumpkins Leave the carving to the grownups. Have children draw the pumpkin design with markers, but keep knives away. Consider using a flashlight or glow stick instead of a candle to light your pumpkin. If you do use a candle, a votive candle is safest. Candlelit pumpkins should be placed on a sturdy table, away from curtains and other flammable objects, and not on a porch or any path where visitors may pass close by. They should never be left unattended. Prepping Your Home Keep your entryway safe for trick-or-treaters by removing all items from the porch or front yard that a child could trip over, like garden hoses, toys, bikes and lawn decorations. To ensure visibility, check outdoor lights and replace burned-out bulbs. Sweep leaves (or snow) from sidewalks and steps. If there are dogs in the home, take steps to ensure they don't jump on trick-or-treaters. Hunting for Treats Young children should always be accompanied by a parent or responsible adult. Give each child and adult a flashlight (with fresh batteries). If older children are heading out to trick-or-treat alone, plan and review a route you can agree on, as well as a specific time they are supposed to return home. Only visit homes with a lit porch light. Never enter a home or a car for a treat. Notify law enforcement authorities of any suspicious or unlawful activity immediately. Since pedestrian injuries are the most common injuries to children on Halloween, remind youngsters to take crosswalk safety precautions. For more key tips regarding Halloween safety for your young trick-or-treaters, visit our partners at Safe Kids Worldwide for a variety of spooky safety resources.
-
Departamento destacado: Security
“Safety is Number One,” isn’t just a saying – it's a fact of life, especially at Renown Health. The safety of all patients, visitors, staff and volunteers is always the top priority, and our Security Department takes that commitment seriously. This team is devoted in their efforts to provide a safe environment for all, building cooperative and proactive security processes leveraging crime prevention techniques and state-of-the-art technology. Renown Security sets the safety and well-being bar high, and they continually exceed that standard day in, day out at all of our hospitals and urgent care, primary care and lab locations. Specially Trained, Continually Present Our Security Department isn’t staffed with your run-of-the-mill Security Officers; these team members surpass security and safety expectations. Think city and state police-level standards. You read that right – many of Renown’s Security Officers come from Nevada Highway Patrol, the Washoe County and Carson City Sheriff’s Offices, the state probation and parole board and more. This team fosters specialized training in a collaborative environment. Every member of the security team has extensive training in compassion, empathy and de-escalation techniques to provide the highest levels of safety and security. They implement this training in all their daily duties, whether they are saying a simple ‘hello’ to a patient passing by or preventing harm to a staff member. Before their shift begins, the team meets to debrief meeting to discuss major incidents that occurred on the previous shift. These meetings ensure the next shift is aware of situations to be on special alert for and individuals to look out for. After, the team members head off to their assignments. “The day could be as mellow as greeting someone at the welcome table, or it could be as chaotic as de-escalating someone in distress,” said Emmanuel Fernandez-Orozco, Supervisor of Security at Renown Regional. “Regardless of the day, every experience is rewarding in its own way. The only thing that is promised is that every day will be different.” While every Security Officer has varying experiences, one aspect of their job always stays the same: they are always on alert for any potential safety issue. Even on the “slowest” days, it is important for this team to stay vigilant in order to mitigate any potential risks. There are several security programs that the team uses to keep everyone at Renown safe and secure: Renown's security operations center team (also known as dispatch) monitors all cameras in real time, with security officers patrolling parking areas 24/7. Security escorts are always available for any employee, patient or guest at every Renown location. Security Officers can escort anyone to their designated site, check surroundings for danger and monitor the person until they safely leave for their next destination. Rescue officers are available for any Renown location where an employee feels unsafe. Security maintains a strong relationship with the Reno Police Department (RPD) and assists with reporting and providing information that aids RPD in pursuing and deterring criminal activity. “In security, we are a counselor, teacher and rule enforcement officer, all rolled into one,” said Bob Stone, Supervisor of Security for Renown Health. Talk about master multitaskers! Protection is only one part of the job. Through positive and meaningful interactions with guests, patients, community and staff, regardless of where they are posted, the Security Department continually helps Renown achieve its mission of making a difference for the people they serve. Devoted Dispatch Speaking of multitasking, no one does this better than the Security Dispatch Center. Security Dispatchers are the “eagle eyes in the sky” at Renown, keeping a close watch on everything that happens within every Renown location, as well as REMSA (including Care Flight). From overlooking the many cameras around campus and administering codes over the PA system to manning the radio and phones to ensure Security Officers are dispatched quickly, our dispatch team helps ensure every safety or security issue at Renown is immediately addressed. When a call comes in, dispatchers like Jessica Fernandez, Security Dispatcher for Renown Health, go through a quick discovery process (sometimes in seconds) to figure out the details of the situation or code and what level of security is needed to assess and de-escalate. According to Jessica, the ability to prioritize is something she values in her work. “80 percent of our duties are on the phone and the radios, and we are skilled in prioritizing concerns based on the sheer volume of calls we get,” she said. Jessica and her teammates are proud of the outcomes from their calls. Their attentiveness to every nook and cranny at Renown and their quick response times to make them not only a valued partner to the Security Department but also a necessity to our health system. Your In-House De-Escalation Experts Being in a hospital environment is undoubtedly stressful for any patient, and many factors can increase these emotions. The Security Department takes these feelings seriously and never hesitates to take appropriate action to ensure the safety of everyone at Renown. With the unfortunate rise of violence against healthcare workers, especially amid the pandemic, our first-rate security team has been crucial in countering violence with specialized de-escalation techniques. The key to de-escalating, according to the Security Department, is to put yourself in the shoes of whoever you are working with. As stated by Bob Stone, the team approaches each situation by asking themselves: How would I want to be treated if I was in the same circumstance? “Being empathetic to their situation and listening to what is going on in their lives is key to re-directing them accordingly,” said Bob. “Applying real-life experience to similar circumstances can make them feel like they are not alone. Educating people on hospital policies can also help them reduce their anxieties and solve the problems.” Jhorddy Lopez, Security Officer at Renown Regional, approaches each situation with the mindset of knowing that each person’s reactions are different. “Different techniques need to be implemented every time,” said Jhorddy. “You have to use your best judgment call.” Quick and effective judgment calls are a task that the Security Department has conquered. Rosie Garcia, Security Officer at Renown Regional, knows that using your best judgment means getting both sides of the story. “Whenever I need to step in and de-escalate a situation, I first speak with whoever is attending to the patient and gather information,” said Rosie. “Then, I always get the patient’s side as well. I want to understand how they’re feeling, so both the staff member and the patient can meet in the middle and come up with a collaborative solution.” An example of the heroism and advanced de-escalation displayed by our Security Officers takes us back to last spring. In the middle of the night, a Care Flight helicopter transporting a patient and their family was about to touch down on the landing pad outside of Renown Regional. Right as the helicopter was about to land, an individual jumped over the safety barricade and onto the landing pad. Alexander Pico, a former Security Officer Lead at Renown Regional (who recently joined the Carson City Sheriff’s Department) immediately communicated with the individual to leave the area. The individual then went under the rear blade, which is the most dangerous part of the helicopter. Knowing that he had to risk his own life at this point to save another, Alexander ran around the back of the helicopter and tackled the individual, preventing catastrophic injury or even death. Steve Perkins now uses this example of a swift judgment call, which was captured on dispatch cameras, as training material for new staff. Exceptional character, compassion and emotional intelligence are the attributes that every member of the Security Department holds. As noted by Steve Perkins, these attributes “allow for a quick assessment of each situation in order to de-escalate and move towards the best possible solution." Securing the Job The Security Department at Renown is actively hiring caring, dedicated team members who are ready to jump in and perform exceptional high-risk healthcare security services for our health system. “We seek people with the right combination of ability and demeanor,” said Steve Perkins. "The training and skills development we provide result in a high caliber of success.” Every team member in the Security Department is passionate about the same thing: helping others. And in a healthcare environment, this is important. “Working a healthcare security job is far different than working any other security job,” said Jhorddy Lopez. “At a hospital, you get the chance to interact with people one-on-one. I get to experience the feeling of, ‘I can make a difference in this person’s life.’” Any interaction can change the course of a person’s day, and the Security Department embraces this fact. “I really do love helping people so much, whether it be an elderly patient who needs help with their wheelchair or a situation where I need to step in and de-escalate,” said Rosie Garcia. In order to succeed in this fast-paced department, being a collaborative team member is crucial. “A good coworker is a team player – someone that loves to work in a team atmosphere,” said Emmanuel Fernandez-Orozco. Jhorddy Lopez reiterates this, adding that “communication and trust are also extremely important. Everyone has to have great communication skills and have each other’s backs.” For people like Bob Stone, having a special connection to Renown inspires him to serve. As someone who experienced two life-saving hospital stays here, he is proud to give back to the organization that gave so much to him. “It was only natural to return to a facility I was familiar with my entire life,” said Bob. “After serving as a paramedic and transporting patients into Renown from Plumas County, I knew I was not done giving back to the community. Renown was the place to do exactly that.” All Genders Welcome A common misconception about the security field is that it is strictly a “man’s job.” In Renown’s Security Department, that couldn’t be further from the truth. As a female Security Officer, Rosie Garcia is a prime example of proving that idea wrong. As a master patroller and de-escalation expert, she ensures everything is running smoothly and that everyone feels safe at all times. “When I first started here, I knew right away that nobody that works here is biased,” said Rosie. “Everyone is equal, and I am treated as an equal in this department. I know I can do the job as well as any man." Both Rosie and her counterparts in the Security Department firmly believe that this line of work is for everyone, and they continually lift each other up and support one another. “No matter your gender, as long as you have confidence and integrity, you will do well,” adds Rosie. The Bottom Line If you are passionate about creating a secure environment to ensure patients get the care they deserve and employees receive the safety they merit, the Security Department is your team to join. “I come into work with pride,” said Jhorddy Lopez. “Knowing that I can change someone’s life – that makes me proud to work here.” “You’re in good hands with us,” closes Steve Perkins.



.png?rev=fcd27802b7604a96bf1056b050ef90c5)